No products in the cart.
Torendo Ku-tab, 2 mg 30 pcs
€14.46 €12.65
Out of stock
(E-mail when Stock is available)
Description
Mental disorders, Schizophrenia, Manic Depressive Psychosis, Alzheimer’s Disease
- The treatment of schizophrenia in adults and children from 13 years old.
- Treatment of manic episodes associated with bipolar disorder of moderate to severe degree in adults and children from 10 years.
- Short-term (up to 6 weeks) treatment of persistent aggression in patients with moderate to severe dementia due to Alzheimer’s disease that does not respond to non-pharmacological methods of correction, and if the patient risks harming himself or others.
- Short-term (up to 6 weeks) symptomatic treatment for persistent aggression as part of a behavioral disorder in children 5 years and older with intellectual disability diagnosed according to DSM-IV criteria, in which medication therapy is required due to the severity of aggression or other disruptive behavior. Pharmacotherapy should be part of a comprehensive treatment program, including psychological and educational interventions. Risperidone should be prescribed by a specialist in child neurology and child psychiatry or by a physician familiar with the treatment of conduct disorder in children and adolescents.
Indications
Indications
Treatment of schizophrenia in adults and children over 13 years of age.
Treatment of moderate to severe manic episodes associated with bipolar disorder in adults and children over 10 years of age.
Short-term (up to 6 weeks) treatment of persistent aggression in patients with moderate to severe Alzheimer’s dementia that is not amenable to non-pharmacological treatment and where the patient is at risk of causing harm to himself or others.
Short-term (up to 6 weeks) symptomatic treatment of persistent aggression in the structure of conduct disorder in children aged 5 years and older with mental retardation diagnosed in accordance with DSM-IV criteria, in which, due to the severity of aggression or other destructive behavior, drug treatment is required. Pharmacotherapy should be part of a comprehensive treatment program, including psychological and educational interventions. Risperidone should be prescribed by a specialist in child neurology and child psychiatry or a physician knowledgeable in the treatment of conduct disorders in children and adolescents.
Pharmacological effect
Pharmacological effect
antipsychotic (neuroleptic)
Special instructions
Special instructions
· Diseases of the cardiovascular system (chronic heart failure, previous myocardial infarction, cardiac muscle conduction disorders);
Hypotension (dose adjustment required);
· dehydration and hypovolemia;
· cerebrovascular accidents;
· Parkinson’s disease;
· convulsions (including history);
· severe renal and/or liver failure (see section “Method of administration and dosage”);
· drug abuse or drug dependence;
· conditions predisposing to the development of tachycardia of the “pirouette” type (bradycardia, electrolyte imbalance, simultaneous use of drugs that prolong the QT interval);
· metabolic disorders, including hyperglycemia, dyslipidemia (patient weight control is required);
· hyperprolactinemia;
Leukopenia, neutropenia, agranulocytosis;
· brain tumor, intestinal obstruction, cases of acute drug overdose, Reye’s syndrome (the antiemetic effect of risperidone may mask the symptoms of these conditions);
risk factors for the development of venous thromboembolism;
Diffuse Lewy body disease;
· use in elderly patients with cerebrovascular dementia;
· pregnancy;
· simultaneous use with furosemide.
Schizophrenia
Children from 13 years old
The recommended initial dose is 0.5 mg once daily in the morning or evening. If necessary, the dosage can be increased after at least 24 hours by 0.5-1 mg per day to the recommended dose of 3 mg per day if well tolerated. Despite the effectiveness demonstrated in the treatment of schizophrenia in adolescents with doses of 1-6 mg per day, no additional effectiveness was observed at doses above 3 mg per day, and higher doses caused more side effects. Doses higher than 6 mg per day have not been studied.
For patients who experience persistent drowsiness, it is recommended to take half the daily dose 2 times a day.
Moderate to severe manic episodes associated with bipolar disorder
Children from 10 years old
The recommended initial dose is 0.5 mg once daily in the morning or evening. If necessary, the dosage can be increased after at least 24 hours by 0.5-1 mg per day to the recommended dose of 1-2.5 mg per day if well tolerated. Despite the effectiveness demonstrated in the treatment of manic episodes associated with bipolar disorder in children with doses of 0.5-6 mg per day, no additional effectiveness was observed at doses above 2.5 mg per day, and higher doses caused more side effects. Doses higher than 6 mg per day have not been studied.
For patients who experience persistent drowsiness, it is recommended to take half the daily dose 2 times a day.
Continuous aggression in the structure of conduct disorder in children aged 5 years and older with mental retardation
Children from 5 to 18 years old
For patients weighing 50 kg or more, the recommended initial dose of Torendo® Qu-tab® is 0.5 mg once a day. If necessary, this dose can be increased by 0.5 mg 1 time per day at least after 24 hours. For most patients, the optimal dose is 1 mg once daily. However, for some patients, 0.5 mg per day is preferable, while some require an increase in dose to 1.5 mg per day.
For patients weighing less than 50 kg, the recommended initial dose of the drug is 0.25 mg once a day. If necessary, this dose can be increased by 0.25 mg 1 time per day at least after 24 hours. For most patients, the optimal dose is 0.5 mg once daily. However, for some patients, 0.25 mg per day is preferable, while some require an increase in dose to 0.75 mg per day.
As with any other symptomatic therapy, the advisability of continuing treatment with Torendo® Qu-tab® should be regularly assessed and confirmed.
Use in children under 5 years of age is not recommended due to lack of data.
Elderly patients
The recommended starting dose is 0.5 mg per dose 2 times a day. The dose can be individually increased by 0.5 mg 2 times a day to 1-2 mg 2 times a day. Experience in elderly patients is limited and caution should be exercised.
Impaired kidney and liver function
Patients with impaired renal function have a reduced ability to eliminate the active antipsychotic fraction compared to other groups of patients. In patients with impaired liver function, an increased concentration of the free fraction of risperidone in the blood plasma is observed.
The initial and maintenance dose, in accordance with the indications, should be reduced by 2 times; the dose increase in patients with impaired liver and kidney function should be carried out more slowly.
The drug Torendo® Ku-tab® should be used with caution in this category of patients.
Use in elderly patients with dementia
Increased mortality in older patients with dementia
A meta-analysis of clinical trials in elderly patients with dementia using atypical antipsychotic drugs showed an increase in mortality compared with the placebo group. Mortality rates in patients receiving risperidone or placebo were 4.0% and 3.1%, respectively. The mean age of patients who died was 86 years (range, 67–100 years). Elderly patients with dementia treated with typical antipsychotic drugs have a small increased risk of death compared with those not treated, according to two large observational studies. At present, insufficient data have been collected to accurately assess this risk. The reason for the increase in this risk is also unknown. Also unknown is the extent to which the increased mortality may be attributable to antipsychotic drugs rather than to the characteristics of this patient population.
Concomitant use with furosemide
When furosemide and oral risperidone were taken concomitantly in elderly patients with dementia, there was an increased mortality rate (7.3%, mean age 89 years, range 75-97 years) compared with the risperidone-only group (3.1%, mean age 84 years, range 70-96 years) and the furosemide-alone group (4.1%, mean age 80 years, range 67-90 years old). An increase in mortality when furosemide was used concomitantly with risperidone was observed in 2 of 4 clinical studies. Concomitant use of risperidone with other diuretics (mainly low-dose thiazide diuretics) was not associated with an increase in mortality.
No pathophysiological mechanisms have been established to explain this observation. However, special care should be taken when using the drug in such cases. Before use, the risk/benefit ratio must be carefully assessed. No increased mortality was found in patients taking other diuretics concomitantly with risperidone. Regardless of therapy, dehydration is a common risk factor for mortality and should be carefully monitored in elderly patients with dementia.
An increase in cerebrovascular adverse events (acute and transient cerebrovascular accidents), including deaths, including deaths (mean age 85 years, range 73-97 years) was observed when risperidone was used compared with placebo in elderly patients with dementia. Therefore, risperidone should be used with caution in patients at risk of stroke.
Cerebrovascular adverse events
In placebo-controlled clinical trials, an approximately 3-fold increased risk of cerebrovascular side effects was observed in patients with dementia taking certain atypical antipsychotic drugs. Pooled data from 6 placebo-controlled studies, mainly including elderly patients with dementia (age >65 years), show that cerebrovascular adverse events (serious and non-serious) occurred in 3.3% (33/1009) of patients treated with risperidone and in 1.2% (8/712) of patients treated with placebo. The risk ratio was 2.96 (1.34, 7.50) with a 95% confidence interval. The mechanism by which this risk increases is unknown. An increased risk cannot be excluded with the use of other antipsychotic drugs or in other patient populations. The drug Torendo® Qu-tab® should be used with caution in patients with risk factors for stroke.
The risk of developing cerebrovascular adverse events in patients with mixed or vascular dementia was significantly higher than in patients with dementia due to Alzheimer’s disease. Therefore, risperidone should not be used in patients with any type of dementia other than dementia due to Alzheimer’s disease.
It is necessary to assess the risk/benefit ratio before using Torendo® Qu-tab® in elderly patients with dementia, taking into account the risk factors for stroke in a particular patient. Patients and their caregivers should be advised to immediately report possible manifestations of cerebrovascular disorders (such as sudden weakness or stiffness/numbness in the face, legs, arms, as well as difficulty speaking and blurred vision) to the physician. Necessary treatment measures should be taken immediately, including discontinuation of risperidone.
Torendo® Qu-tab® can only be used for short-term treatment of persistent aggression in patients with moderate to severe Alzheimer’s dementia, as an adjunct to non-pharmacological treatment methods when they are ineffective or of limited effectiveness, and when there is a risk of harm to the patient himself or others.
The patient’s condition and the need for continued risperidone therapy should be continually assessed.
Orthostatic hypotension
Due to the α-adrenergic blocking effect of risperidone, some patients may develop orthostatic hypotension, especially during the initial dose titration period. Cases of clinically significant arterial hypotension have been described with simultaneous use of risperidone with antihypertensive drugs in the post-marketing period. The drug Torendo® Ku-tab® should be used with caution in patients with cardiovascular diseases (for example, chronic heart failure, myocardial infarction, cardiac muscle conduction disorders, dehydration, hypovolemia or cerebrovascular diseases). Appropriate dose adjustment is also necessary. It is recommended to evaluate the possibility of dose reduction in case of arterial hypotension.
Leukopenia, neutropenia and agranulocytosis
Cases of leukopenia, neutropenia and agranulocytosis have been described with the use of antipsychotics, including the use of the drug risperidone. Agranulocytosis was observed very rarely (< 1/10,000 patients) during post-marketing surveillance. Patients with a clinically significant decrease in the leukocyte count or a history of drug-induced leukopenia/neutropenia should be monitored in the first few months after initiation of therapy, and when the first signs of a clinically significant decrease in the leukocyte count appear, in the absence of other causative factors, treatment should be discontinued.
Patients with clinically significant neutropenia should be closely monitored for fever or other symptoms of infection and treatment should be initiated immediately if such symptoms occur. Patients with severe neutropenia (absolute neutrophil count < 1x 109/L) should stop taking Torendo® Qu-tab® until the white blood cell count returns.
Tardive dyskinesia/extrapyramidal symptoms
Therapy with dopamine receptor antagonists can cause tardive dyskinesia, which is characterized by rhythmic involuntary movements, mainly of the tongue and/or facial muscles. The occurrence of extrapyramidal symptoms is a risk factor for the development of tardive dyskinesia. If a patient experiences objective or subjective symptoms indicating tardive dyskinesia, the advisability of discontinuing all antipsychotic drugs, including Torendo® Qu-tab®, should be considered.
Caution should be exercised in patients taking psychostimulants (eg, methylphenidate) and risperidone concomitantly due to the possibility of extrapyramidal symptoms. In these cases, gradual withdrawal of psychostimulants is recommended.
Neuroleptic malignant syndrome (NMS)
When treated with antipsychotic drugs, the development of NMS, characterized by hyperthermia, muscle rigidity, instability of the function of the autonomic nervous system, depression of consciousness and increased activity of creatine phosphokinase in the blood plasma, as well as myoglobinuria (rhabdomyolysis) and acute renal failure, is possible. If a patient experiences objective or subjective symptoms of NMS, all antipsychotic medications, including risperidone, should be immediately discontinued.
Parkinson’s disease and dementia with Lewy bodies
The use of antipsychotic drugs, including Torendo® Qu-tab®, in patients with Parkinson’s disease or dementia with Lewy bodies should be carried out with caution, as both groups of patients have an increased risk of developing NMS and increased sensitivity to antipsychotic drugs (including dullness of pain sensitivity, confusion, postural instability with frequent falls and extrapyramidal symptoms). Parkinson’s disease may worsen when taking risperidone.
Hyperglycemia and diabetes mellitus
Cases of the development of hyperglycemia, diabetes mellitus and aggravation of diabetes mellitus have been described. In some cases, there was an increase in body weight preceding therapy, which can be regarded as a predisposing factor. In very rare cases, the development of ketoacidosis and rarely – diabetic coma were observed. As with any antipsychotic, patients should be monitored for symptoms of hyperglycemia (such as polydipsia, polyuria, polyphagia, and weakness). In patients with diabetes mellitus, blood glucose concentrations should be regularly monitored.
Weight gain
There is a significant increase in body weight. It is necessary to regularly monitor patients’ body weight.
Hyperprolactinemia
Based on the results of in vitro studies, it has been suggested that the growth of mammary tumor cells can be stimulated by prolactin. Although clinical and epidemiological studies have not shown a clear association of hyperprolactinemia with antipsychotic medications, caution should be exercised when using risperidone in patients with a history of this. The drug Torendo® Qu-tab® should be used with caution in patients with existing hyperprolactinemia and in patients with possible prolactin-dependent tumors.
QT prolongation
In very rare cases, prolongation of the QT interval has been observed in the post-marketing period. As with other antipsychotics, caution should be exercised when using Torendo® Qu-tab® in patients with cardiovascular disease, a family history of QT interval prolongation, bradycardia, electrolyte imbalance (hypokalemia, hypomagnesemia), as this may increase the risk of arrhythmogenic effects or when used concomitantly with drugs that prolong the QT interval.
Convulsions
The drug Torendo® Ku-tab® should be used with caution in patients with a history of seizures or in conditions accompanied by a decrease in the threshold of seizure activity.
Priapism
Since risperidone has an α-adrenergic blocking effect, priapism may develop when used.
Dysregulation of body temperature
When using antipsychotic drugs, such an undesirable effect as impaired thermoregulation is described. Caution must be exercised when using the drug Torendo® Qu-tab® in patients who may be exposed to factors that cause an increase in body temperature, such as intense physical activity, dehydration, high ambient temperature, and simultaneous use with drugs that have anticholinergic activity.
Antiemetic effect
In preclinical studies of risperidone, an antiemetic effect was observed. This effect, when occurring in humans, may mask signs and symptoms of overdose of some drugs or diseases such as intestinal obstruction, Reye’s syndrome, and brain tumors.
Impaired kidney and liver function
In patients with impaired renal function, the ability to eliminate the active antipsychotic fraction is lower than in adult patients with normal renal function. In patients with impaired liver function, the concentration of the free fraction of risperidone in the blood plasma increases.
Venous thromboembolism
Cases of venous thromboembolism have been described with the use of antipsychotic drugs. It is necessary to identify all possible risk factors for the development of thromboembolic complications before and during therapy with Torendo® Ku-tab® and take preventive measures.
Intraoperative floppy iris syndrome (ISID)
ISDR was observed during cataract surgery in patients receiving drugs that antagonize alpha1-adrenergic receptors, including the drug Torendo® Qu-tab®. ISDR may increase the risk of visual complications during and after surgery. It is necessary to inform the ophthalmologist in advance about the use of drugs that antagonize alpha1-adrenergic receptors currently or in the past. The potential benefit of discontinuing therapy with drugs that antagonize alpha1-adrenergic receptors before cataract surgery has not been established. It is necessary to assess the benefit/risk ratio of discontinuing antipsychotic therapy.
Children and teenagers
Before using Torendo® Qu-tab® in children or adolescents with mental retardation, it is necessary to carefully assess their condition for the presence of physical or social causes of aggressive behavior, such as pain or inadequate demands of the social environment.
The sedative effect of risperidone should be carefully monitored in this population due to the possible effect on learning ability. Changing the timing of risperidone administration may reduce the effects of sedation on alertness in adolescents and children.
Risperidone use was associated with increases in mean body weight and body mass index. Height changes in longitudinal studies were within expected age-related norms. The effects of long-term use of risperidone on sexual development and growth have not been fully studied.
Due to the possible impact of prolonged hyperprolactinemia on growth and sexual development in children and adolescents, regular clinical assessment of hormonal status should be carried out, including measurement of height, body weight, monitoring of sexual development, menstrual cycle and other possible prolactin-dependent effects.
During risperidone therapy, regular assessment should be carried out to identify extrapyramidal symptoms and other movement disorders.
Active ingredient
Active ingredient
Risperidone
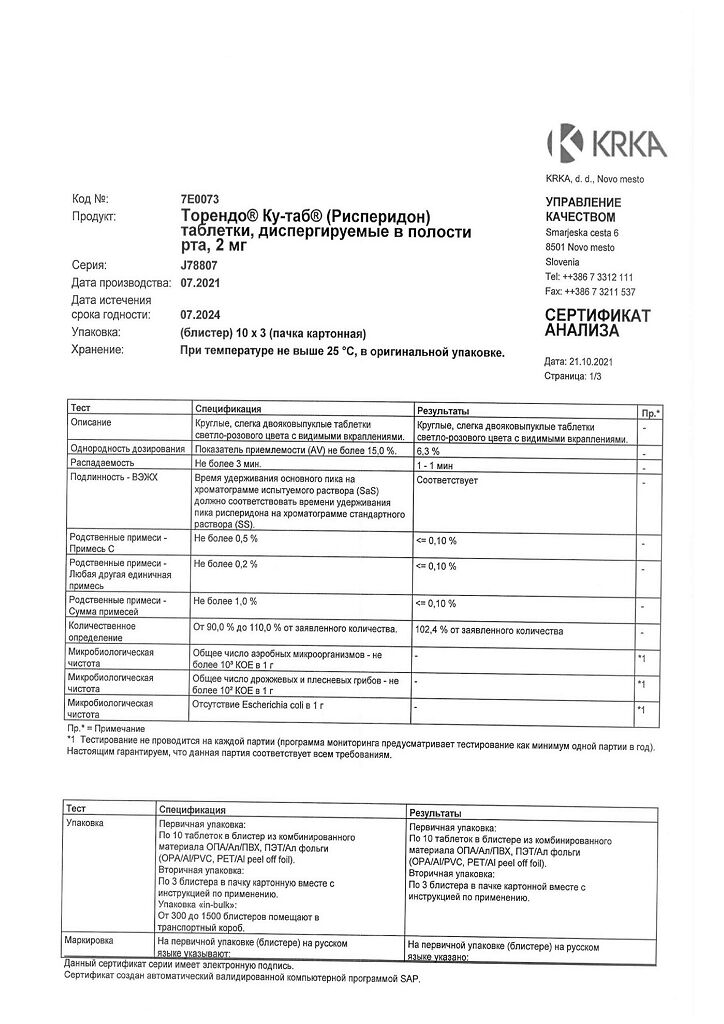
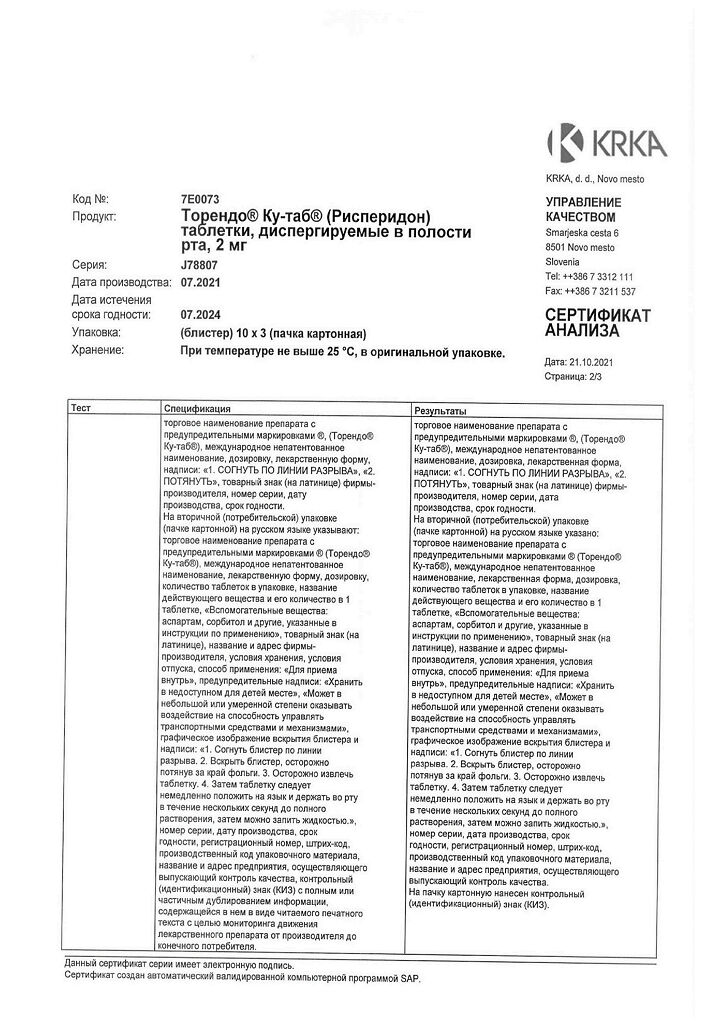
Composition
Composition
1 tablet, dispersible in the oral cavity, 0.5 mg/1 mg/2 mg contains:
Active ingredient:
Risperidone 0.50 mg/1.00 mg/2.00 mg
Excipients: mannitol, butyl methacrylate, dimethylaminoethyl methacrylate and methyl methacrylate copolymer [1:2:1], povidone-K25, microcrystalline cellulose, low-substituted hyprolose, aspartame, crospovidone, red iron oxide dye (E172), mint flavor1, menthol flavor2, calcium silicate, magnesium stearate
1Mint flavor: corn maltodextrin, acacia gum, sorbitol, mint oil, levomenthol.
2Menthol flavoring: corn maltodextrin, flavoring components.
Pregnancy
Pregnancy
Pregnancy
There are no controlled studies of the use of risperidone in pregnant women. In animal studies, risperidone was not teratogenic, but other reproductive toxicities were observed. The potential risk of risperidone in humans is not known.
When antipsychotics (including risperidone) were used during the third trimester of pregnancy, the newborn developed reversible extrapyramidal symptoms and/or withdrawal symptoms that varied in severity and duration. Cases of agitation, hypertension, hypotension, tremor, somnolence, respiratory distress and malnutrition have been reported. Therefore, newborns should be closely monitored.
The use of Torendo® Ku-tab® during pregnancy is possible only if the expected benefit to the mother outweighs the potential risk to the fetus. If it is necessary to discontinue therapy during pregnancy, the drug should be discontinued gradually.
Breastfeeding period
In animal studies, risperidone and 9-hydroxyrisperidone were excreted into breast milk. Risperidone and 9-hydroxyrisperidone have also been demonstrated to pass into human breast milk in small amounts. There is no data on the development of side effects in infants during breastfeeding. Therefore, the issue of breastfeeding should be decided taking into account the possible risk to the child.
Fertility
Like other drugs that are antagonists of dopamine D2 receptors, risperidone increases the concentration of prolactin in the blood plasma. Hyperprolactinemia can suppress the secretion of hypothalamic gonadotropin-releasing hormone, which leads to decreased secretion of pituitary gonadotropin. This, in turn, can cause suppression of reproductive function due to impaired steroidogenesis in the gonads in male and female patients. No significant effects were observed in preclinical studies.
Contraindications
Contraindications
· Hypersensitivity to risperidone or any other components of the drug.
· Phenylketonuria.
· Congenital fructose intolerance.
Side Effects
Side Effects
The most commonly observed adverse reactions (incidence ≥ 5%) were insomnia, anxiety, headache, upper respiratory tract infection, and parkinsonism.
Dose-dependent adverse reactions are parkinsonism and akathisia.
Side effects of risperidone noted in clinical studies of risperidone in oral and extended-release injectable dosage forms, as well as those obtained during post-registration surveillance, are presented with a distribution by frequency and organ system. The frequency of side effects was classified as follows: very common (≥ 1/10 cases), common (≥ 1/100 to < 1/10 cases), uncommon (≥ 1/1000 to < 1/100 cases), rare (≥ 1/10,000 to < 1/1000 cases), very rare (< 1/10,000 cases), frequency unknown (frequency occurrence cannot be estimated based on existing data). Within each frequency group, side effects are presented in order of decreasing importance.
Infectious and parasitic diseases:
often: pneumonia, flu, bronchitis, upper respiratory tract infections, urinary tract infections, sinusitis, ear infections;
uncommon: viral infections, tonsillitis, inflammation of the subcutaneous fat, otitis media, eye infections, localized infections, akarodermatitis, respiratory tract infections, cystitis, onychomycosis;
rarely: lower respiratory tract infections, chronic otitis media, infections, subcutaneous abscess.
Disorders of the blood and lymphatic system:
uncommon: neutropenia, decreased white blood cell count, anemia, thrombocytopenia, decreased hematocrit, decreased eosinophil count, decreased hemoglobin;
rarely: granulocytopenia, agranulocytosis.
Immune system disorders:
uncommon: hypersensitivity reactions to the components of the drug;
rarely: drug hypersensitivity, anaphylactic reaction.
Endocrine system disorders:
often: increased prolactin levels1;
rarely: impaired production of antidiuretic hormone, glucosuria.
Metabolic and nutritional disorders:
often: weight gain, increased appetite, decreased appetite;
uncommon: weight loss, diabetes mellitus3, anorexia, polydipsia, hyperglycemia, increased plasma cholesterol concentrations;
rarely: hypoglycemia, water intoxication, increased insulin, increased concentration of triglycerides in blood plasma;
very rare: diabetic ketoacidosis.
Mental disorders:
very often: insomnia;
often: restlessness, agitation, sleep disturbances, anxiety, depression;
uncommon: confusion, mania, decreased libido, lethargy, nervousness, nightmares;
rarely: anorgasmia, flattening of affect.
Nervous system disorders:
very often: parkinsonism2, headache, drowsiness, sedation;
often: akathisia2, dizziness2, tremor2, dystonia2, lethargy, dyskinesia2;
Uncommon: lack of response to stimuli, loss of consciousness, decreased level of consciousness, syncope, impaired consciousness, stroke, transient ischemic attack, dysarthria, impaired attention, hypersomnia, postural dizziness, imbalance, tardive dyskinesia, speech impairment, impaired coordination, hypoesthesia, taste disorder, taste perversion, convulsions, cerebral ischemia, movement disorder, psychomotor agitation, paresthesia;
rarely: neuroleptic malignant syndrome (NMS), diabetic coma, cerebrovascular disorders, head tremor;
frequency unknown: stuttering.
Visual disorders:
often: blurred vision, conjunctivitis;
uncommon: conjunctival hyperemia, blurred vision, eye discharge, periorbital edema, dry eyes, increased lacrimation, photophobia;
rarely: decreased visual acuity, impaired eye movement, involuntary rotation of the eyeballs, formation of crusts on the edge of the eyelid, glaucoma, intraoperative floppy iris syndrome (IFIS), retinal artery occlusion.
Hearing and labyrinth disorders:
uncommon: vertigo, ear pain, tinnitus.
Cardiac disorders:
often: tachycardia;
uncommon: atrioventricular block, right or left bundle branch block, atrial fibrillation, palpitations, cardiac conduction disturbances, prolongation of the QT interval on the ECG, bradycardia, abnormalities on the ECG;
rarely: sinus arrhythmia, sinus bradycardia;
frequency unknown: first degree atrioventricular block.
Vascular disorders:
often: arterial hypertension;
uncommon: hypotension, orthostatic hypotension, hot flashes;
rarely: pulmonary embolism, deep vein thrombosis.
Disorders of the respiratory system, chest and mediastinal organs:
often: shortness of breath, nosebleeds, cough, nasal congestion, pain in the larynx and pharynx;
uncommon: wheezing, aspiration pneumonia, pulmonary congestion, respiratory distress, moist rales, airway obstruction, dysphonia;
rarely: sleep apnea syndrome, hyperventilation.
Digestive system disorders:
often: vomiting, diarrhea, constipation, nausea, abdominal pain, dyspepsia, dry oral mucosa, abdominal discomfort, hypersalivation, toothache;
uncommon: dysphagia, gastritis, fecal incontinence, fecaloma, gastroenteritis, flatulence;
rarely: intestinal obstruction, pancreatitis, swelling of the lips, swelling of the tongue, cheilitis;
very rare: ileus.
Disorders of the liver and biliary tract:
infrequently: increased activity of transaminases, gamma-glutamyltransferase, liver enzymes (in particular, increased level of alanine aminotransferase activity) in blood plasma;
rarely: jaundice.
Disorders of the skin and subcutaneous tissues:
often: skin rash, erythema;
uncommon: urticaria, skin lesions, loss of skin integrity, itching, acne, acne, skin discoloration, alopecia, seborrheic dermatitis, dry skin, hyperkeratosis, eczema;
rarely: drug rash, dandruff;
very rare: Quincke’s edema.
Musculoskeletal and connective tissue disorders:
often: muscle spasms, musculoskeletal pain, arthralgia, back pain, pain in the extremities, pain in the buttocks;
uncommon: increased activity of creatine phosphokinase in blood plasma, muscle weakness, myalgia, neck pain, swollen joints, poor posture, stiffness in the joints, muscle pain in the chest;
rarely: rhabdomyolysis.
Renal and urinary tract disorders:
often: enuresis, urinary incontinence;
uncommon: urinary retention, dysuria, pollakiuria.
Pregnancy, postpartum and perinatal conditions:
rarely: withdrawal syndrome in newborns.
Disorders of the genital organs and breast:
uncommon: amenorrhea, sexual dysfunction, erectile dysfunction, ejaculation disorder, galactorrhea, gynecomastia, menstrual disorder, vaginal discharge, pain in the breast area, discomfort in the breast area;
rarely: priapism, delayed menstruation, engorgement of the mammary glands, enlarged mammary glands, discharge from the mammary glands.
General disorders and disorders at the injection site:
often: edema, pyrexia, fatigue, peripheral edema, generalized edema, asthenia, chest pain, pain;
uncommon: facial swelling, gait disturbance, poor health, sluggishness, flu-like condition, malaise, thirst, chest discomfort, chills, fever, discomfort;
rarely: hypothermia, decreased body temperature, withdrawal syndrome, cold extremities, induration.
Injuries, intoxications and complications of manipulation:
often: falling;
uncommon: pain during procedures.
1– hyperprolactinemia in some cases can lead to gynecomastia, menstrual irregularities, amenorrhea and galactorrhea.
2- extrapyramidal disorders may manifest as parkinsonism (hypersalivation, musculoskeletal stiffness, parkinsonism, drooling, cogwheel rigidity, bradykinesia, hypokinesia, mask-like face, muscle tension, akinesia, nuchal rigidity, muscle rigidity, parkinsonian gait, abnormalities glabellar reflex, parkinsonian rest tremor), akathisia (akathisia, restlessness, hyperkinesia and restless legs syndrome), tremor, dyskinesia (dyskinesia, muscle twitching, choreoathetosis, athetosis and myoclonus), dystonia.
The term dystonia includes dystonia, muscle spasms, muscle hypertonia, torticollis, involuntary muscle contractions, muscle contracture, blepharospasm, eye movements, tongue paralysis, facial spasm, laryngospasm, myotonia, opisthotonus, oropharyngeal spasm, pleurototonus, tongue spasm, and trismus. Tremors include tremor and parkinsonian resting tremor. It should also be noted that there is a wider range of symptoms that are not always of extrapyramidal origin. Insomnia includes sleep disorder and intrasomnia disorder. Seizures include a grand mal seizure. Menstrual disorders include irregular menstruation, oligomenorrhea. Edema includes generalized edema, peripheral edema, and mild edema.
3- In placebo-controlled studies, diabetes mellitus occurred in 0.18% of patients receiving risperidone compared with 0.11% of patients in the placebo group. In all clinical studies, the overall incidence of diabetes mellitus in patients taking risperidone was 0.43%.
Undesirable effects when using paliperidone
Paliperidone is an active metabolite of risperidone, therefore the adverse reaction profiles of risperidone and paliperidone are interrelated. In addition to the above, the following adverse reactions have been reported with the use of paliperidone, which may also occur with the use of risperidone:
From the cardiovascular system: postural orthostatic tachycardia syndrome.
Class effects
As with other antipsychotic drugs, very rare cases of QT prolongation have been observed during post-marketing surveillance. Other cardiovascular class effects observed with antipsychotic drugs that prolong the QT interval include ventricular arrhythmias, ventricular fibrillation, ventricular tachycardia, sudden death, cardiac arrest, and torsade de pointes (TdP).
Venous thromboembolism
Cases of venous thromboembolism, including pulmonary embolism and cases of deep vein thrombosis, have been observed with the use of antipsychotic drugs (frequency unknown).
Weight gain
In placebo-controlled studies in patients with schizophrenia, weight gain of at least 7% after 6 to 8 weeks was observed in 18% of patients taking risperidone and 9% of patients taking placebo. In placebo-controlled clinical trials in patients with manic episodes, the incidence of weight gain of 7% or more after 3 weeks of treatment was comparable in the risperidone group (2.5%) and placebo group (2.4%), and slightly higher in the active control group (3.5%).
In long-term clinical studies, children with conduct disorders increased body weight by an average of 7.3 kg after 12 months of therapy. The expected increase in body weight in children 5-12 years old with normal development is 3-5 kg per year, from 12-16 years old – 3-5 kg per year for girls and about 5 kg per year for boys.
Special patient groups
Side effects that were reported with greater frequency in elderly patients with dementia and in children than in adult patients are described below.
Elderly patients with dementia
Transient ischemic attacks and stroke were observed in clinical studies with an incidence of 1.4% and 1.5%, respectively, in elderly patients with dementia. In addition, the following adverse effects have been reported in elderly patients with dementia at an incidence of ≥ 5% and at an incidence at least 2 times higher than in other patient populations: urinary tract infections, peripheral edema, lethargy and cough.
Children
The following adverse effects were reported in children (5 to 17 years of age) with an incidence of ≥ 5% and an incidence of at least 2 times that in other patient populations during clinical trials: drowsiness/sedation, fatigue, headache, increased appetite, vomiting, upper respiratory tract infection, nasal congestion, abdominal pain, dizziness, cough, pyrexia, tremor, diarrhea, enuresis.
Interaction
Interaction
Interactions related to the pharmacodynamics of the drug
Drugs that prolong the QT interval
As with other antipsychotic drugs, caution should be exercised when using Torendo® Qu-tab® simultaneously with drugs that prolong the QT interval, for example, with antiarrhythmic drugs (quinidine, disopyramide, procainamide, propafenone, amiodarone, sotalol, etc.), tricyclic antidepressants (amitriptyline, etc.), tetracyclic antidepressants (maprotiline). etc.), some antihistamines, other antipsychotics, some antimalarials (quinine, mefloquine, etc.), drugs that cause electrolyte imbalance (hypokalemia, hypomagnesemia), bradycardia or inhibit the hepatic metabolism of risperidone. This list is not exhaustive.
Centrally acting drugs and alcohol
The drug Torendo® Ku-tab® should be used with caution in combination with other drugs and substances of central action, especially alcohol, opiates, antihistamines and benzodiazepines due to the increased risk of sedation.
Levodopa and dopamine receptor agonists
The drug Torendo® Qu-tab® may reduce the effectiveness of levodopa and other dopamine receptor agonists. If this combination is necessary, especially in end-stage Parkinson’s disease, the lowest effective dose of each drug should be prescribed.
Antihypertensive drugs
When risperidone was used concomitantly with antihypertensive drugs in the post-registration period, clinically significant arterial hypotension was observed.
Paliperidone
It is not recommended to use Torendo® Qu-tab® and paliperidone simultaneously, since paliperidone is an active metabolite of risperidone. Concomitant use of a combination of risperidone and paliperidone may lead to increased concentrations of the active antipsychotic fraction.
Interactions related to drug pharmacokinetics
Eating does not affect the absorption of risperidone.
Risperidone is primarily metabolized by the CYP2D6 isoenzyme and to a lesser extent by the CYP3A4 isoenzyme. Risperidone and its active metabolite 9-hydroxyrisperidone are substrates of P-glycoprotein (P-gp). Drugs that affect the activity of the CYP2D6 isoenzyme and drugs that significantly inhibit or induce the activity of the CYP3A4 isoenzyme and/or P-gp may affect the pharmacokinetics of the active antipsychotic fraction of risperidone.
Potent inhibitors of the CYP2D6 isoenzyme
With simultaneous use of risperidone and potent inhibitors of the CYP2D6 isoenzyme, the plasma concentration of risperidone and, to a lesser extent, the active antipsychotic fraction may increase. Higher doses of a strong CYP2D6 inhibitor may increase the concentration of the active antipsychotic fraction of risperidone (eg, paroxetine, see below). It is expected that other CYP2D6 inhibitors, such as quinidine, may have a similar effect on risperidone plasma concentrations. When initiating or discontinuing therapy with a combination of risperidone and paroxetine, quinidine or another strong inhibitor of the CYP2D6 isoenzyme, especially at higher doses, the dose of Torendo® Qu-tab® should be adjusted.
CYP3A4 and/or P-gp inhibitors
The simultaneous use of Torendo® Qu-tab® and potent inhibitors of the CYP3A4 isoenzyme and/or P-gp can significantly increase the concentration of the active antipsychotic fraction of risperidone in the blood plasma. When initiating or discontinuing therapy with a combination of risperidone and itraconazole or another strong inhibitor of the CYP3A4 isoenzyme and/or P-gp, the dose of Torendo® Qu-tab® should be adjusted.
Inducers of the isoenzyme CYP3A4 and/or P-gp
Concomitant use of Torendo® Qu-tab® with a powerful inducer of the CYP3A4 isoenzyme and/or P-gp may reduce the concentration of the active antipsychotic fraction of risperidone in the blood plasma. When initiating or discontinuing therapy with a combination of risperidone and carbamazepine or another strong inducer of the isoenzyme CYP3A4 and/or P-gp, the dose of Torendo® Qu-tab® should be adjusted. The effects of CYP3A4 inducers occur over time, so it may take up to 2 weeks to achieve maximum effect after starting treatment. Accordingly, when discontinuing an inducer of the CYP3A4 isoenzyme, it may take up to 2 weeks until the effect disappears.
Drugs that bind tightly to plasma proteins
With the simultaneous use of the drug Torendo® Ku-tab® with drugs that are highly bound to blood plasma proteins, there is no clinically significant displacement of the drug from the complex with blood plasma proteins.
When using concomitant treatment, you should refer to the instructions for use of the corresponding drug and, if necessary, adjust the dosage of the drugs taken.
Psychostimulants
When psychostimulants (eg, methylphenidate) and risperidone are used concomitantly, changing the order of administration of one or both drugs may lead to extrapyramidal symptoms (see section “Special Instructions”).
Children
Drug interaction studies were conducted only in adult patients. The relevance of these studies in children is unknown.
The simultaneous use of psychostimulants (for example, methylphenidate) and the drug Torendo® Qu-tab® in children does not change the pharmacokinetic parameters and effectiveness of risperidone.
Effect of other drugs on the pharmacokinetics of risperidone
Antibacterial drugs
Erythromycin, a moderate inhibitor of CYP3A4 and P-gp, does not affect the pharmacokinetics of risperidone and the active antipsychotic fraction.
Rifampicin, a powerful inducer of the CYP3A4 and P-gp isoenzymes, causes a decrease in the concentration of the active antipsychotic fraction in the blood plasma.
Anticholinesterase drugs
Donepezil and galantamine, which are substrates of the CYP2D6 and CYP3A4 isoenzymes, do not have a clinically significant effect on the pharmacokinetics of neticurisperidone and the active antipsychotic fraction.
Antiepileptic drugs
Carbamazepine, a potent inducer of the CYP3A4 and P-gp isoenzymes, reduces the concentration of the active antipsychotic fraction of risperidone in the blood plasma. Similar effects were observed with the use of phenytoin and phenobarbital, which are also inducers of the CYP3A4 isoenzyme and P-gp.
Topiramate moderately reduces the bioavailability of risperidone, but not the active antipsychotic fraction. This interaction is not considered clinically significant.
Antifungal drugs
Itraconazole, a potent CYP3A4 and P-gp inhibitor, at a dose of 200 mg/day increases the plasma concentration of the active antipsychotic fraction by approximately 70% when using risperidone at a dose of 2 to 8 mg/day.
Ketoconazole, a potent inhibitor of the CYP3A4 and P-gp isoenzyme, at a dose of 200 mg/day increases the concentration of risperidone in the blood plasma and reduces the concentration of 9-hydroxyrisperidone in the blood plasma.
Neuroleptics
Phenothiazines may increase plasma concentrations of risperidone, but not the active antipsychotic fraction.
Antiviral drugs
Protease inhibitors: No formal study data available. Because ritonavir is a strong inhibitor of CYP3A4 and a weak inhibitor of CYP2D6, ritonavir and ritonavir-boosted protease inhibitors may lead to increased concentrations of the active antipsychotic fraction of risperidone.
Beta blockers
Some beta-blockers may increase plasma concentrations of risperidone, but not the active antipsychotic fraction.
Calcium channel blockers
Verapamil, a moderate inhibitor of the CYP3A4 isoenzyme and P-gp, increases the concentration of risperidone and the active antipsychotic fraction in the blood plasma.
Drugs for the treatment of diseases of the gastrointestinal tract
H2 receptor antagonists: cimetidine and ranitidine, which are weak inhibitors of the CYP2D6 and CYP3A4 isoenzymes, increase the bioavailability of risperidone, but minimally affect the concentration of the active antipsychotic fraction in the blood plasma.
Serotonin reuptake inhibitors and tricyclic antidepressants
Fluoxetine, a potent inhibitor of the CYP2D6 isoenzyme, increases the concentration of risperidone in the blood plasma, but has a lesser effect on the concentration of the active antipsychotic fraction.
Paroxetine, a potent inhibitor of the CYP2D6 isoenzyme, increases the concentration of risperidone in the blood plasma, but in doses up to 20 mg/day it has a lesser effect on the concentration of the active antipsychotic fraction. However, higher doses of paroxetine may increase the concentration of the active antipsychotic fraction of risperidone.
Tricyclic antidepressants can increase the concentration of risperidone in the blood plasma, but do not affect the concentration of the active antipsychotic fraction. Amitriptyline does not affect the pharmacokinetics of risperidone or the active antipsychotic fraction.
Sertraline is a weak inhibitor of the CYP2D6 isoenzyme, and fluvoxamine is a weak inhibitor of the CYP3A4 isoenzyme. At doses up to 100 mg/day, sertraline and fluvoxamine do not have a clinically significant effect on the concentration of the active antipsychotic fraction of risperidone. However, the use of sertraline or fluvoxamine in doses above 100 mg/day may lead to an increase in the concentration of the active antipsychotic fraction of risperidone.
Effect of risperidone on the pharmacokinetics of other drugs
Antiepileptic drugs
Risperidone does not have a clinically significant effect on the pharmacokinetics of valproic acid or topiramate.
Neuroleptics
Aripiprazole, a substrate of CYP2D6 and CYP3A4 isoenzymes: Risperidone has no effect on the pharmacokinetics of aripiprazole and its active metabolite, dehydroaripiprazole.
Cardiac glycosides
Risperidone does not have a clinically significant effect on the pharmacokinetics of digoxin. The use of therapeutic doses of digoxin in combination with risperidone at a dose of 0.25 mg 2 times a day did not lead to changes in exposure and did not require dosage adjustment.
Lithium preparations
Risperidone does not have a clinically significant effect on the pharmacokinetics of lithium preparations.
Concomitant use with furosemide
See the Precautions section for information regarding increased mortality in elderly patients with dementia receiving furosemide concomitantly.
Overdose
Overdose
Symptoms: drowsiness, sedation, depression of consciousness, tachycardia, arterial hypotension, extrapyramidal disorders, in rare cases, prolongation of the QT interval and convulsions. In case of overdose in patients taking risperidone and paroxetine simultaneously, the development of polymorphic ventricular tachycardia of the “pirouette” type has been described.
In case of acute overdose, it is necessary to consider the possibility of overdose from taking several drugs.
Treatment: ensure a clear airway for adequate oxygenation and ventilation. Gastric lavage (after intubation, if the patient is unconscious), as well as the use of activated charcoal and laxatives, should only be done if risperidone was taken no more than 1 hour ago.
To timely diagnose a possible heart rhythm disorder, it is necessary to begin ECG monitoring as soon as possible. There is no specific antidote; appropriate symptomatic therapy must be carried out. When blood pressure decreases and vascular collapse, intravenous administration of infusion solutions and/or sympathomimetic drugs is recommended. If acute extrapyramidal symptoms develop, anticholinergic drugs should be prescribed. Careful medical observation and ECG monitoring are carried out until the symptoms of intoxication completely disappear.
Clinical pharmacology
Clinical pharmacology
Pharmacodynamics
Risperidone is a selective monoaminergic antagonist with high affinity for serotonin 5-HT2 and dopamine D2 receptors. Risperidone also binds to alpha1-adrenergic receptors and, to a lesser extent, to H1-histamine and alpha2-adrenergic receptors.
It has a weak affinity for 5-HT1A-, 5-HT1C-, 5-HT1D-serotonergic, D1-dopaminergic receptors and haloperidol-sensitive sigma receptor binding sites, and insignificant affinity for 5-HT1B and 5-HT3 receptors. Does not have the ability to interact with m-cholinergic and beta1-, beta2-adrenergic receptors.
Risperidone reduces the productive symptoms of schizophrenia, causes less suppression of motor activity and induces catalepsy to a lesser extent than classical antipsychotics. Balanced central antagonism to serotonin and dopamine reduces the likelihood of developing extrapyramidal disorders and expands the therapeutic effect of the drug to cover negative and affective symptoms of schizophrenia.
Pharmacokinetics
Suction
Risperidone is completely absorbed after oral administration, reaching maximum plasma concentrations after 1-2 hours. The absolute bioavailability of risperidone after oral administration is 70%. The relative bioavailability after oral administration of risperidone in tablet form is 94% when compared with risperidone in solution form. Eating does not affect the absorption of the drug, so risperidone can be used regardless of the time of meal. The equilibrium concentration of risperidone in the body is achieved within 1 day in most patients. The equilibrium concentration of 9-hydroxyrisperidone is achieved within 4-5 days.
Distribution
Risperidone is rapidly distributed in the body. The volume of distribution is 1-2 l/kg. In blood plasma, risperidone binds to albumin and alpha1-acid glycoprotein. Risperidone is 90% bound to plasma proteins, 9-hydroxyrisperidone is 77% bound.
Metabolism and excretion
Risperidone is metabolized in the liver with the participation of the CYP2D6 isoenzyme. The main metabolite is 9-hydroxyrisperidone, which has similar pharmacological activity to risperidone. Risperidone and 9-hydroxyrisperidone constitute the active antipsychotic fraction. The CYP2D6 isoenzyme is subject to genetic polymorphism. In patients who are extensive metabolizers of CYP2D6, risperidone is rapidly converted to 9-hydroxyrisperidone, while in patients who are poor metabolizers of CYP2D6, this process occurs much more slowly. Although extensive metabolizers have lower risperidone concentrations and higher 9-hydroxyrisperidone concentrations than poor metabolizers, the pharmacokinetics of the active antipsychotic fraction after single or multiple doses are similar in the two patient groups.
Another pathway of risperidone metabolism is N-dealkylation. In vitro studies on human liver microsomes showed that risperidone at clinically significant concentrations does not significantly inhibit the metabolism of drugs biotransformed by isoenzymes of the cytochrome P450 system, including CYP1A2, CYP2A6, CYP2C8/9/10, CYP2D6, CYP2E1, CYP3A4 and CYP3A5. A week after starting to take risperidone, 70% of the dose is excreted by the kidneys (while the excretion of risperidone and 9-hydroxyrisperidone by the kidneys is 35-45% of the dose taken, the rest is inactive metabolites) and 14% through the intestines. After oral administration in patients with psychosis, the half-life (T1/2) of risperidone is about 3 hours, T1/2 of 9-hydroxyrisperidone and the active antipsychotic fraction is 24 hours.
Linearity
The concentration of risperidone in blood plasma is directly proportional to the dose taken in the therapeutic dose range.
Pharmacokinetics in certain groups of patients
Elderly patients, patients with impaired liver and kidney function
After a single dose of risperidone in elderly patients, the concentration of the active antipsychotic fraction in the blood plasma increased by an average of 43%, T1/2 – by 38%, and clearance decreased by 30%.
In patients with renal failure, an increase in plasma concentration and a decrease in clearance of the active antipsychotic fraction by an average of 60% were observed. In patients with liver failure, plasma risperidone concentrations did not change, but the average concentration of the free fraction of risperidone increased by 35%.
Children
The pharmacokinetics of risperidone, 9-hydroxyrisperidone and the active antipsychotic fraction in children is comparable to that in adult patients.
Gender, race, smoking
Population pharmacokinetic analysis did not reveal obvious effects of gender, race, or smoking on the pharmacokinetics of neticurisperidone and the active antipsychotic fraction.
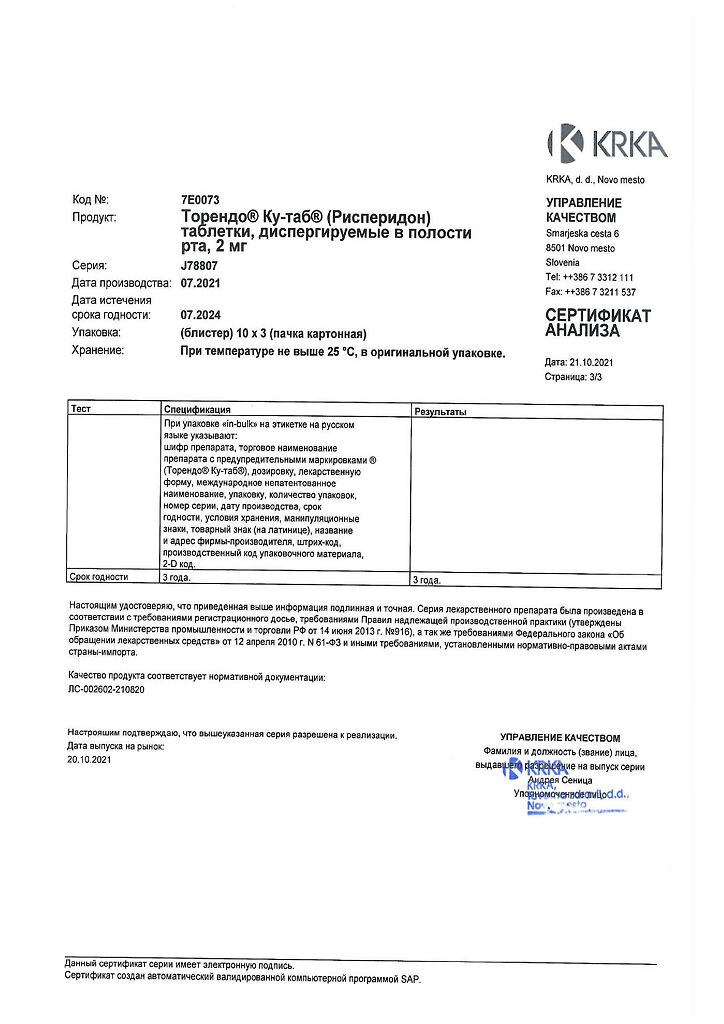
Storage conditions
Storage conditions
At a temperature not exceeding 25 ºС, in the original packaging.
Keep out of the reach of children.
Shelf life
Shelf life
3 years.
Do not use the drug after the expiration date.
Manufacturer
Manufacturer
KRKA dd Novo Mesto, Slovenia
Additional information
| Shelf life | 3 years. Do not use the drug after the expiration date. |
|---|---|
| Conditions of storage | At the temperature not more than 25 ºС, in the original package. Keep out of reach of children. |
| Manufacturer | KRKA dd Novo mesto, Slovenia |
| Medication form | Oral dispersible tablets |
| Brand | KRKA dd Novo mesto |
Other forms…
Related products
Buy Torendo Ku-tab, 2 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.