No products in the cart.
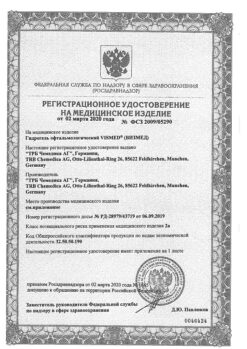
Tizoptan, eye drops 0.3 mg+5 mg/ml 3 ml
€21.90 €18.25
Description
Tisoptan® is a combination medication with bimatoprost and timolol reducing intraocular pressure (IOP) through a synergistic interaction resulting in a significantly more pronounced hypotensive effect compared to the effects of each component alone.
Bimatoprost is a synthetic prostamide with a chemical structure similar to prostaglandin F2α (PGF2α). Bimatoprost has no effect on any of the known types of prostaglandin receptors. The hypotensive effect of bimatoprost is achieved by enhancing the outflow of intraocular fluid through the trabecula and through the uveoscleral pathway of the eye.
Timolol is a non-selective beta-adrenoblocker and has no intrinsic sympathomimetic and membrane-stabilizing activity.
Timolol reduces IOP by reducing the formation of intraocular fluid. The exact mechanism of action is not known; it may be related to inhibition of cyclic adenosine monophosphate (c-AMP) synthesis and is caused by endogenous stimulation of beta-adrenergic receptors.
Pharmacokinetics
Tisoptan®
The systemic absorption of the drug is minimal and does not differ with both combined treatment and instillation of each component of the drug individually.
Two 12-month studies showed no systemic cumulation of either active ingredient.
Bimatoprost
In in vitro studies, bimatoprost has been shown to penetrate the iris and sclera.
When bimatoprost 0.03% solution is instilled 1 drop in both eyes once a day for 2 weeks, the maximum plasma concentration (Cmax) of bimatoprost is reached within 10 minutes after application, and within 1.5 h its plasma concentration decreases to the lower limit of determination (0,025 ng/ml) the mean Cmax and area under the concentration-time curve (AUC0-24h) values of bimatoprost were close on days 7 and 14 of administration, being 0.08 ng/ml and 0.09 ng*h/ml respectively, indicating that the equilibrium concentration of bimatoprost is reached within the first week of use.
Bimatoprost is moderately distributed in the tissues, and the systemic volume of distribution when the equilibrium concentration of the drug is reached is 0.67 L/kg. Bimatoprost is predominantly found in the blood plasma.
The binding of bimatoprost to plasma proteins is approximately 88%. Bimatoprost undergoes oxidation, N-deletylation and glucuronidation with the formation of various metabolites.
Bimatoprost is excreted mainly by the kidneys. About 67% of the drug administered intravenously to healthy volunteers was excreted with the urine, and 25% was excreted through the gastrointestinal tract (GIT). The half-life (T1/2) of bimatoprost, determined after intravenous administration, was approximately 45 minutes; and total clearance was 1.5 L/h/kg.
In elderly patients:
When bimatoprost is used twice daily, the mean (AUC0-24 h) in elderly patients is 0.0634 ng*h/mL, which is significantly higher than this value in healthy young persons – 0.0218 ng*h/mL.
However, this difference has no clinical significance because the systemic exposure of bimatoprost during its topical administration in elderly patients and healthy young adults remains very low. There is no cumulation of bimatoprost in systemic circulation and the safety profile does not differ between elderly patients and young adults.
Timolol
In patients who underwent cataract surgery, after instillation of eye drops as a 0.5% solution, the Cmax of timolol in intraocular fluid after 1 h was 898 ng/ml. Some amount of the drug enters the systemic bloodstream and is metabolized in the liver. T1/2 of timolol is about 4-6 hours.
A portion of timololol that is metabolized in the liver is excreted through the gastrointestinal tract, and another portion and metabolites are excreted by the kidneys. Timolol is slightly bound to plasma proteins.
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
How to take, the dosage
How to take, the dosage
Interaction
Interaction
Special Instructions
Special Instructions
In common with other ophthalmic medications, Tizoptan® may enter the systemic bloodstream. Due to the presence of timolol, a beta-adrenergic component, various types of adverse reactions (cardiovascular, respiratory and other systems) may occur as with systemic beta-blockers. The incidence of adverse reactions is lower when the drug is administered topically than when it is used systemically.
The cardiovascular system
The symptoms of heart failure should be compensated before starting Tizoptan®. Regular monitoring of patients with severe heart failure and determination of heart rate is necessary.
Beta-adrenoblockers may mask symptoms of hypoglycemia, hyperthyroidism, and worsen the course of Prinzmetal angina, severe peripheral and central vascular disorders, and arterial hypotension.
Patients with severe peripheral circulatory disorders (e.g., severe forms of Raynaud’s disease or Raynaud’s syndrome) should use the drug with caution.
Respiratory system
In the use of timolol, there have been reports of respiratory adverse effects, including deaths due to bronchospasm in patients with bronchial asthma and, less frequently, from heart failure.
Other beta-adrenoblockers
Timolol may affect intraocular pressure or potentiate the effects of systemic beta-blockers in patients already receiving a systemic beta-adrenoblocker. Close monitoring of such patients is recommended. Also, the use of two topical beta-adrenoblockers is not recommended.
Anaphylactic reactions
In patients with a history of atopy and severe anaphylactic reactions to various allergens the doses of epinephrine (adrenaline) that are usually used to control anaphylactic reactions may be ineffective with beta-adrenoblockers.
Chorioidal detachment
Cases of chorioidal detachment have been reported with the use of therapy that reduces intraocular fluid flow (e.g., timolol, acetazolamide) after filtration surgery.
Surgical anesthesia
Ophthalmic drugs with beta-blocking effects may suppress the systemic effects of beta-agonists such as adrenaline.
The anesthesiologist should be advised of the patient’s use of timolol.
Liver
In patients with mild liver disease or baseline elevated liver enzyme activity – alanine aminotransferase (ALT), aspartate aminotransferase (ACT) and/or total bilirubin, bimatoprost had no effect on liver function during a study period of more than 24 months. There are no data on adverse reactions due to the effect of timolol on liver function.
The visual system
Patients should be advised of possible eyelash growth, increased eyelid pigmentation, and iris pigmentation before starting treatment, as these side effects have been established in studies of bimatoprost and the bimatoprost+timololol combination.
Some changes may be permanent and may be accompanied by differences between eyes if instillations of the drug were only given in one eye. After discontinuation of the drug
Tizoptan® iris pigmentation may remain permanent. After 12 months of treatment with Tizoptan®, the incidence of iris pigmentation was noted in 0.2% of patients. And after 12 months of treatment with bimatoprost alone in the form of eye drops of 1.5%, no further increase in the incidence of this effect was observed during the therapy duration of 3 years.
The enhancement of iris pigmentation is due to increased production of melanocytes, not simply to an increase in their number. The duration of the development of the effect of increased iris pigmentation is unknown. The change in iris color seen with bimatoprost may be subtle over a period of several months to several years.
The use of the drug has no effect on nevi or iris pigment deposits. Periorbital pigmentation has been reported to be reversible in some patients. There may be a change in refraction (due to discontinuation of myotic therapy in some cases).
The skin
Possible hair growth on areas of skin where the drug was accidentally applied. It is important to use Tizoptan® strictly according to the directions for medical use and to avoid contact of Tizoptan® with the skin.
Auxiliary substances
The excipient benzalkonium chloride in Tizoptan® may irritate the eye mucosa and may cause discoloration of soft contact lenses. Contact lenses shall be removed prior to instillation of the drug; they may be put on 15 minutes after instillation.
Benzalkonium chloride may cause acute keratitis and/or toxic corneal ulcer. In this regard, the patient’s condition should be monitored during frequent or prolonged treatment with Tizoptan® in patients with “dry” eye syndrome and in case of corneal changes.
After opening the bottle one cannot exclude the possibility of microbial contamination of its contents, which may lead to inflammatory lesions of the eyes. The shelf life of the drug after the first opening of the bottle is 28 days. After this time the vial should be thrown away, even if the solution has not been completely used.
It is recommended to write on the carton of the drug the date of opening the vial.
Contraindications
Contraindications
Hepatic and renal disorders (the drug has not been adequately studied in this category of patients).
In patients with risk factors for macular edema (e.g., aphakia, pseudophakia, posterior lens capsule rupture, and intraocular surgery, retinal vein occlusion, inflammatory eye disease and diabetic retinopathy).
In patients with active intraocular inflammation (e.g., uveitis) because inflammation may worsen.
In patients with mild to moderate chronic obstructive pulmonary disease (COPD), and only when the expected benefits exceed the possible risks.
In patients with grade I atrioventricular block due to adverse effects on intracardiac conduction time.
In patients with corneal diseases, because it can induce dry eye syndrome. In patients with diabetes mellitus (unstable course) and impaired glucose tolerance because the beta-adrenoblocker timolol in Tizoptan® may mask the signs of hypoglycemia.
In patients with ocular inflammatory changes, neovascular, inflammatory, closed angle glaucoma, congenital glaucoma or narrow angle glaucoma (no data on efficacy and safety studies).
Side effects
Side effects
The adverse reactions observed in clinical trials of bimatoprost+timololol combination were limited to those previously observed with the active ingredients bimatoprost and timolol separately.
The majority of adverse reactions observed in clinical trials were mild visual reactions, none of which were serious.
In a 12-month clinical trial, the most common adverse reaction was conjunctival hyperemia (mostly mild non-inflammatory in nature), which was seen in approximately 26% of patients and caused 1.5% of patients to discontinue treatment.
The adverse reactions are presented below according to organ and organ system involvement and frequency of occurrence. The frequency of adverse reactions is defined as follows: very common (>1/10), common (>1/100, <1/10); infrequent (>1/1000, <1/100), rare (>1/10000, <1/1000), very rare (<1/10000), frequency unknown (frequency cannot be determined from available data).
The following adverse reactions were observed in a 12-month clinical trial of bimatoprost+timololol combination.
Immune system disorders:
Frequency unknown: hypersensitivity reactions, including signs or symptoms of allergic dermatitis, angioedema, allergic eye reactions.
Mental disorders:
frequency unknown: insomnia, nightmares.
Nervous system disorders:
often: headache, dizziness;
frequency unknown: dysgeusia.
Visual organ disorders:
very common: conjunctival hyperemia;
common: pitting keratitis, corneal erosion, burning sensation, itching in eyes, tingling sensation in eyes, foreign body sensation, dry eyes, redness of eyelids, pain in eyes, photophobia, ocular discharge;
infrequent: iridocyclitis, conjunctival edema, painful eyelids, asthenopia, trichiasis, iris hyperpigmentation, deepening of the eyelid crease, eyelid retraction;
frequency unknown – cystoid macular edema, eye swelling, blurred vision.
Heart disorders
Frequency unknown: bradycardia.
Respiratory system disorders:
common: rhinitis;
infrequent: dyspnea;
frequency unknown: bronchospasm (mainly in patients with existing bronchospastic disease), asthma.
Skin and subcutaneous tissue disorders:
common: eyelid skin pigmentation, hirsutism, periocular skin hyperpigmentation.
General disorders and disorders at the site of administration:
frequency unknown: fatigue.
Like other topically administered ophthalmic drugs, Tizoptan® (bimatoprost + timolol) is absorbed into the systemic bloodstream. Timolol absorption may cause adverse effects similar to those of systemic beta-blocking agents. The number of systemic adverse reactions after topical administration is lower than after systemic administration.
Other adverse reactions that have been observed with each of the components of the drug and are potentially possible during treatment with Tizoptan®:
Bimatoprost
Visual disorders: allergic conjunctivitis, darkening of eyelashes, blepharospasm, retinal hemorrhage, uveitis, periorbital erythema, blurred vision.
Cardiac disorders: increase in blood pressure, Raynaud’s syndrome, coldness of extremities.
General disorders and disorders at the site of administration: asthenia.
Gastrointestinal disorders: nausea.
Laboratory and instrumental data: changes in liver enzyme activity.
Timolol
Visual disorders: blepharospasm, retinal hemorrhage, uveitis.
Vascular disorders: decreased blood pressure.
Respiratory, thoracic and mediastinal system disorders: exacerbation of asthma.
Gastrointestinal disorders: perversion of taste, nausea, diarrhea, dyspepsia, dry oral mucosa, abdominal pain, vomiting.
Immune system disorders: systemic allergic reactions, including Quincke’s edema, urticaria, focal and multiple rashes, rash, anaphylaxis.
Metabolic and nutrition disorders: hypoglycemia.
Mental disorders: insomnia, depression, nightmares, memory loss.
Nervous system disorders: fainting, acute impairment of cerebral circulation, increased symptoms of myasthenia gravis, paresthesia, cerebral ischemia.
Cardiac disorders: atrioventricular block, cardiac arrest, bradycardia, heart failure, congestive heart failure, chest pain, palpitations, edema.
Respiratory system, chest and mediastinum disorders: cough.
Gastrointestinal disorders: perversion of taste, nausea, diarrhea, dyspepsia, dry mouth, abdominal pain, vomiting.
Skin and subcutaneous tissue disorders: alopecia, psoriasis-like rashes or exacerbation of psoriasis, skin rash.
Muscular and connective tissue disorders: muscle pain.
Gender and mammary gland disorders: sexual dysfunction, decreased libido.
General disorders and disorders at the site of administration: asthenia/fatigue.
Indesirable reactions to phosphate-containing eye drops.
Very rare cases of corneal calcification have been reported when co-administered with phosphate-containing eye drops in some patients.
Overdose
Overdose
Pregnancy use
Pregnancy use
Similarities
Similarities
Additional information
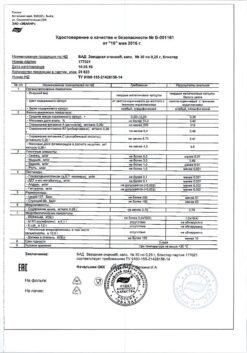
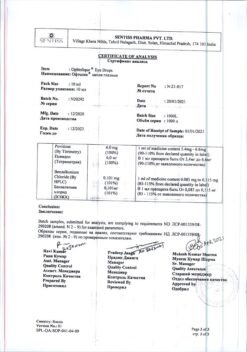
| Shelf life | 2 years. |
|---|---|
| Conditions of storage | Store at temperatures under 25 ° C. Keep out of reach of children. |
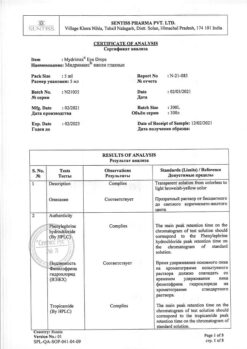
| Manufacturer | Sentiss Pharma Pvt.Ltd, India |
| Medication form | eye drops |
| Brand | Sentiss Pharma Pvt.Ltd |
Related products
Buy Tizoptan, eye drops 0.3 mg+5 mg/ml 3 ml with delivery to USA, UK, Europe and over 120 other countries.