No products in the cart.
Thiapridal, tablets 100 mg 20 pcs
€57.83 €48.19
Description
Tiapridal is neuroleptic, anxiolytic, analgesic.
It selectively blocks central dopamine D2 receptors without affecting D1 receptors.
Pharmacodynamics
It has antipsychotic and anxiolytic effects, including in the treatment of alcohol, opium and nicotine withdrawal. It relieves dyskinesia, promotes mental clarity in elderly patients and has analgesic properties.
Pharmacokinetics
After an intravenous injection of 200 mg Cmax (2.5 mcg/mL) is determined after 30 minutes, after 200 mg oral administration (1.3 mcg/mL) after 1 hour. Bioavailability is 75% (taking immediately before meals increases bioavailability by 20%, Cmax by 40%). Absorption in the elderly is delayed.
Distribution is quick: in 1 hour it is determined in many tissues and organs, passes through BBB and placental barrier, penetrates into breast milk (concentration in milk is half of that in blood plasma). Practically does not bind with plasma proteins, erythrocytes. T1/2 is 2.9 h in women and 3.6 h in men.
It is moderately metabolized: 70% of the dose taken is found unchanged in the urine. Excretion occurs mainly by the kidneys; CL is 330 ml/min. In patients with impaired renal excretory function, the degree of decrease in excretion correlates with the value of Cl creatinine. Daily dose in creatinine Cl less than 20 ml/min should be decreased twice, in creatinine Cl less than 10 ml/min – 4 times.
Indications
Indications
Behavioral disorders (excitement, aggressiveness), especially in patients with alcoholism; pain (intense, intractable); dyskinesia (spontaneous, tardive, Huntington’s chorea).
Pharmacological effect
Pharmacological effect
Tiapridal – antipsychotic, anxiolytic, analgesic.
Selectively blocks central dopamine D2 receptors without affecting D1 receptors.
Pharmacodynamics
Has antipsychotic and anxiolytic effects, incl. in the treatment of alcohol, opium and nicotine withdrawal. Eliminates dyskinesia, promotes clarity of thinking in elderly patients, and has analgesic properties.
Pharmacokinetics
After an intramuscular injection of 200 mg, Cmax (2.5 μg/ml) is determined after 30 minutes, after taking 200 mg orally (1.3 μg/ml) – after 1 hour. Bioavailability – 75% (taken immediately before meals increases bioavailability by 20%, Cmax – by 40%). Absorption is slower in older people.
Distribution is rapid: after 1 hour it is detected in many tissues and organs, passes the BBB and placental barrier, and penetrates into breast milk (the concentration in milk is half that in blood plasma). Practically does not bind to plasma proteins or red blood cells. T1/2 – 2.9 hours in women and 3.6 hours in men.
Moderately metabolized: 70% of the dose taken is found unchanged in the urine. Excretion occurs mainly by the kidneys; Cl is 330 ml/min. In patients with impaired renal excretory function, the degree of decrease in excretion correlates with the creatinine Cl value. The daily dose when creatinine Cl is less than 20 ml/min should be reduced by 2 times, less than 10 ml/min – by 4 times.
Special instructions
Special instructions
Neuroleptic malignant syndrome is characterized by pallor, hyperthermia, muscle rigidity, dysfunction of the peripheral nervous system, and impaired consciousness.
Signs of peripheral nervous system dysfunction, such as increased sweating and blood pressure lability, may precede the onset of hyperthermia and therefore represent early warning signs. Some risk factors, such as dehydration or organic brain damage, although this effect of antipsychotics may be explained by idiosyncrasy, appear to be predisposing.
Tiapride causes a dose-dependent prolongation of the QT interval. This effect is known to increase the risk of serious ventricular arrhythmias, it is enhanced by bradycardia, hypokalemia, and in the case of congenital or acquired long QT interval (combination with drugs that prolong the QT interval).
Hypokalemia should be corrected before starting the drug, and the clinical picture, electrolyte balance and ECG should be monitored. For extrapyramidal syndrome caused by antipsychotics, anticholinergic drugs should be prescribed instead of dopaminergic agonists.
Impact on the ability to drive vehicles and operate machinery: during the treatment period, it is necessary to refrain from engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Tiapride
Composition
Composition
Active ingredient:
111.1 mg tiapride hydrochloride, which corresponds to 100 mg tiapride base;
Excipients:
mannitol,
microcrystalline cellulose,
povidone,
colloidal silicon dioxide,
magnesium stearate.
Pregnancy
Pregnancy
The drug is contraindicated in the first trimester of pregnancy and lactation.
There are no data available regarding the effect of antipsychotics used during pregnancy on the fetal brain (it is preferable not to use tiapride during pregnancy). However, if the drug is still used during pregnancy, it is recommended to limit the dose and duration of treatment if possible.
With prolonged treatment and/or use of high doses and/or in late pregnancy, monitoring of the neurological functions of the newborn is justified.
Breastfeeding
It is unknown whether tiapride passes into breast milk, so breastfeeding is prohibited.
Contraindications
Contraindications
Hypersensitivity, pheochromocytoma (including suspected), pregnancy, breastfeeding.
Side Effects
Side Effects
With long-term use of Tiapridal in high doses, drowsiness, muscle hypotonia, dyskinesia (early – spastic, torticollis, trismus, oculomotor disorders; and late), extrapyramidal symptoms, muscle relaxation, decreased blood pressure, amenorrhea, galactorrhea, hyperprolactinemia, gynecomastia, impotence, frigidity, weight gain, malignant neuroleptic syndrome (unexplained hyperthermia – requires discontinuation of the drug).
Interaction
Interaction
Not recommended combinations
When used together with antiarrhythmic drugs of class 1a (quinidine, hydroquinidine, disopyramide) and class III (amiodarone, sotalol, dofetilide, ibutilide), antiarrhythmic drugs, some neuroleptics (thioridazine, chlorpromazine, levomepromazine, trifluoperazine, cyamemazine, sulpiride, amisulpride, pimozide, haloperidol, droperidol) and other drugs such as bepridil, cisapride, difemanil, erythromycin, mizolastine, vincamine, increase the risk of ventricular arrhythmias, as well as atrial fibrillation.
Alcohol
Alcohol enhances the sedative effect of neuroleptics.
Levodopa
There is a joint antagonism of the action of levodopa and antipsychotics. In patients suffering from Parkinson’s disease, it is recommended to use the minimum effective doses of levodopa and tiapride.
Dopaminergic agonists may cause or worsen psychotic disorders. If treatment with antipsychotics is necessary for a patient suffering from Parkinson’s disease receiving a dopaminergic drug, the dose of the latter should be gradually reduced until discontinuation (abrupt withdrawal can lead to the development of neuroleptic malignant syndrome).
Sparfloxacin, moxifloxacin:
The risk of ventricular arrhythmias, as well as atrial fibrillation, increases. If the combination cannot be avoided, the QT interval should first be checked and ECG monitoring performed.
Combinations requiring caution
Drugs that cause bradycardia (slow calcium channel blockers: diltiazem, verapamil; beta-blockers; clonidine, guanfacine; digitalis preparations, cholinesterase inhibitors: donezepil, rivastigmine, galantamine, pyridostigmine, neostigmine).
Drugs that can cause hypokalemia: potassium-sparing diuretics, laxatives, amphotericin B, glucocorticoids, tetracosactide. The risk of ventricular arrhythmias, as well as atrial fibrillation, increases.
Combinations to Consider
Antihypertensive drugs (all):
Additive effect, increased risk of postural hypotension.
Drugs that depress the central nervous system:
Morphine derivatives (analgesics, antitussives and substitution therapy); barbiturates; benzodiazepines and other anxiolytics; sleeping pills; antidepressants with sedative effects; HI antihistamines with sedative effects; centrally acting antihypertensives; baclofen; thalidomide increases the depression of central nervous system function.
Overdose
Overdose
Symptoms: excessive sedation, drowsiness, depression of consciousness up to coma, arterial hypotension, extrapyramidal symptoms.
Treatment: drug withdrawal, symptomatic and detoxification therapy, monitoring vital body functions (especially cardiac activity – the risk of prolongation of the QT interval) until the symptoms of intoxication completely disappear.
If severe extrapyramidal symptoms appear, anticholinergic treatment is prescribed.
Since tiapride is poorly dialyzable, hemodialysis is not recommended for removal of the substance. There is no known antidote for tiapride.
Storage conditions
Storage conditions
Store out of reach of children, in a dry place, protected from light at a temperature not exceeding 25°C.
Shelf life
Shelf life
5 years.
Manufacturer
Manufacturer
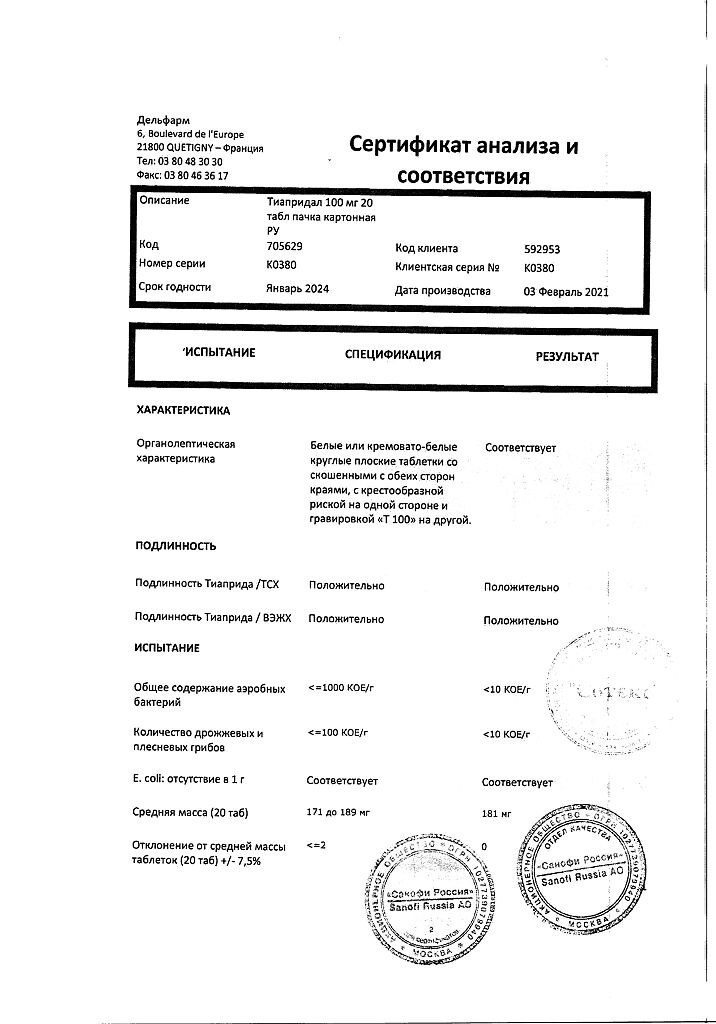
Delpharm Dijon, France
Additional information
| Shelf life | 5 years. |
|---|---|
| Conditions of storage | Store out of the reach of children, dry, protected from light at a temperature not exceeding 25 ° C. |
| Manufacturer | Delpharm Dijon, France |
| Medication form | pills |
| Brand | Delpharm Dijon |
Related products
Buy Thiapridal, tablets 100 mg 20 pcs with delivery to USA, UK, Europe and over 120 other countries.