No products in the cart.
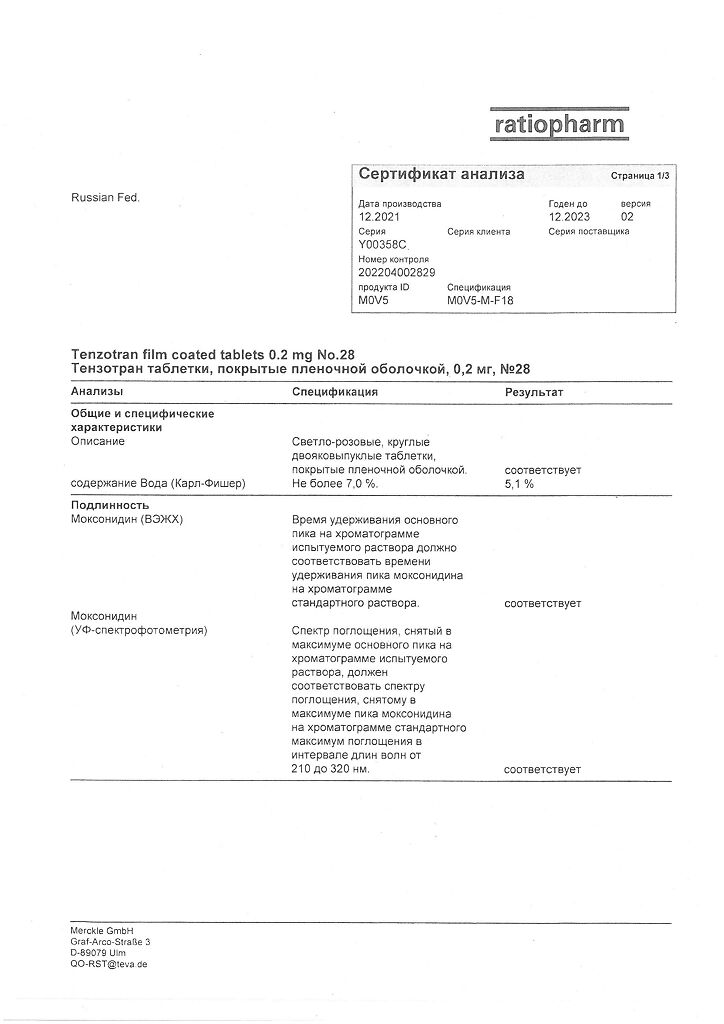
Tenzotran, 0.2 mg 28 pcs.
€11.01 €9.17
Description
Tenzotran is a hypotensive agent of central action. < br>
A selective agonist of imidazoline receptors responsible for reflex control of the sympathetic nervous system (localized in the ventero-lateral part of the medulla oblongata). < br>
It has low affinity with central alpha2-adrenoreceptors, due to interaction with which the sedative effect and dryness of the oral mucosa are mediated. < br>
Moxonidine improves insulin sensitivity index by 21% compared to placebo in obese patients and insulin-resistant patients with moderate arterial hypertension. < br>
Impact on hemodynamics: decrease of systolic and diastolic blood pressure (BP) with single and prolonged use of moxonidine is associated with decrease of sympathetic pressor action on peripheral vessels and decrease of total peripheral vascular resistance, whereas cardiac output and heart rate (HR) do not change significantly.
Indications
Indications
Arterial hypertension.
Pharmacological effect
Pharmacological effect
Tenzotran is a centrally acting antihypertensive drug.
Selective agonist of imidazoline receptors responsible for reflex control of the sympathetic nervous system (localized in the venterolateral medulla oblongata).
It has low affinity for central alpha2-adrenergic receptors, due to interaction with which sedation and dryness of the oral mucosa are mediated.
Moxonidine improves insulin sensitivity index by 21% compared with placebo in obese and insulin-resistant patients with moderate hypertension.
Effect on hemodynamics: a decrease in systolic and diastolic blood pressure (BP) with single and long-term use of moxonidine is associated with a decrease in the pressor effect of the sympathetic system on peripheral vessels, a decrease in total peripheral vascular resistance, while cardiac output and heart rate (HR) do not change significantly.
Special instructions
Special instructions
If it is necessary to cancel simultaneously taken beta-blockers and Tenzotran, first cancel the beta-blockers and, only after a few days, Tenzotran.
It is not recommended to prescribe tricyclic antidepressants simultaneously with Tenzotran.
During treatment, regular monitoring of blood pressure, heart rate and ECG is necessary.
Moxonidine can be prescribed with thiazide diuretics, angiotensin-converting enzyme (ACE) inhibitors and slow calcium channel blockers.
Tenzotran should be stopped gradually.
Patients with rare hereditary conditions of galactose intolerance, lactase deficiency or glucose-galactose malabsorption should not take this drug.
Active ingredient
Active ingredient
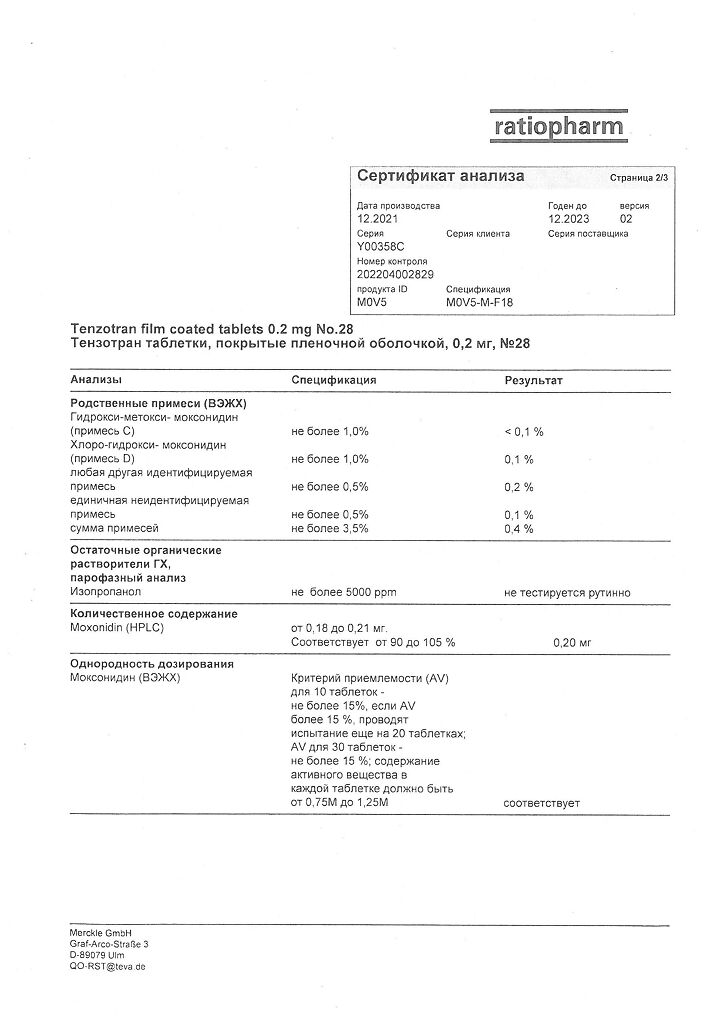
Moxonidine
Composition
Composition
Film-coated tablets.
1 tablet contains:
active substance:
moxonidine 0.2 mg;
excipients:
lactose monohydrate,
povidone – K25,
crospovidone,
magnesium stearate,
Opadry Y-1-7000,
red iron oxide dye.
Pregnancy
Pregnancy
There is no clinical evidence of a negative effect on pregnancy.
However, Tenzotran should be prescribed to pregnant women only if the potential benefit to the mother outweighs the possible risk to the fetus.
Moxonidine passes into breast milk; women are advised to stop breastfeeding or discontinue the drug during treatment.
Contraindications
Contraindications
Hypersensitivity to moxonidine and other components of the drug, sick sinus syndrome, sinoatrial and atrioventricular block II and III degrees, severe bradycardia (heart rate less than 50 beats/min.), chronic heart failure III and IV functional class according to the NYHA classification, history of angioedema, unstable angina, severe liver failure (more than 9 points on the Child-Pugh scale), chronic renal failure (creatinine clearance less than 30 ml/min., creatinine more than 160 µmol/l), age under 18 years (efficacy and safety have not been established), lactation period; galactose intolerance, lactase deficiency or glucose-galactose malabsorption syndrome.
With caution: Parkinson’s disease (severe form), epilepsy, glaucoma, depression, intermittent claudication, Raynaud’s disease, first degree atrioventricular block, chronic renal failure (creatinine clearance more than 30, but less than 60 ml/min.), severe cerebrovascular disorders, after myocardial infarction, chronic heart failure I and II functional class, liver dysfunction, hemodialysis, pregnancy.
Side Effects
Side Effects
Especially at the beginning of therapy, the most common adverse reactions were: dry mouth, headache, asthenia and drowsiness.
The intensity of their manifestation and frequency decrease with repeated use. Frequency of development: very common (more than 1/10), often (more than 1/100, less than 1/10), sometimes (more than 1/1000 and less than 1/100), very rare (less than 1/1000, including individual reports).
From the cardiovascular system: often – vasodilation; sometimes – a pronounced decrease in blood pressure, orthostatic hypotension, paresthesia, Raynaud’s syndrome, peripheral circulation disorders;
From the central nervous system: often – increased fatigue, drowsiness, headache, dizziness; sometimes – insomnia, asthenia;
From the digestive tract: dryness of the oral mucosa; often – nausea, constipation and other gastrointestinal dysfunction; very rarely – hepatitis, cholestasis;
From the skin and skin: sometimes – allergic reactions;
From the genitourinary system: sometimes – urinary retention or incontinence, impotence, decreased libido;
On the part of the organ of vision: sometimes – dry eyes, causing itching or a burning sensation;
Other: sometimes – edema of various localizations, weakness in the legs, angioedema, fainting, fluid retention, anorexia, pain in the parotid glands, gynecomastia.
Interaction
Interaction
Moxonidine can be prescribed with thiazide diuretics, slow calcium channel blockers and other antihypertensive drugs.
The combined use of moxonidine with these and other antihypertensive drugs leads to an additive effect and enhanced hypotensive effect.
When prescribing moxonidine with hydrochlorothiazide, glibenclamide (glyburide) or digoxin, there is no pharmacokinetic interaction.
Tricyclic antidepressants may reduce the effectiveness of centrally acting antihypertensive agents; therefore, it is not recommended to prescribe tricyclic antidepressants simultaneously with moxonidine.
Moxonidine moderately enhances decreased cognitive performance in patients taking lorazepam.
Prescribing moxonidine together with benzodiazepines may be accompanied by an increase in the sedative effect of the latter.
Moxonidine may potentiate the effect of ethanol when used together.
When moxonidine is prescribed together with moclobemide, there is no pharmacodynamic interaction.
Overdose
Overdose
There have been reports of several cases of non-fatal overdose when doses up to 19.6 mg were used per dose.
Symptoms: headache, sedation, drowsiness, marked decrease in blood pressure, dizziness, asthenia, bradycardia, dry oral mucosa, vomiting and stomach pain, increased fatigue. Potentially also possible: short-term increase in blood pressure, tachycardia, hyperglycemia.
Treatment: there is no specific antidote. Gastric lavage, taking activated charcoal and laxatives, symptomatic therapy.
In the case of a pronounced decrease in blood pressure, it is recommended to restore circulating blood volume by administering fluids and administering dopamine. Bradycardia can be relieved with atropine.
Alpha-adrenergic antagonists may reduce or eliminate transient hypertension following moxonidine overdose.
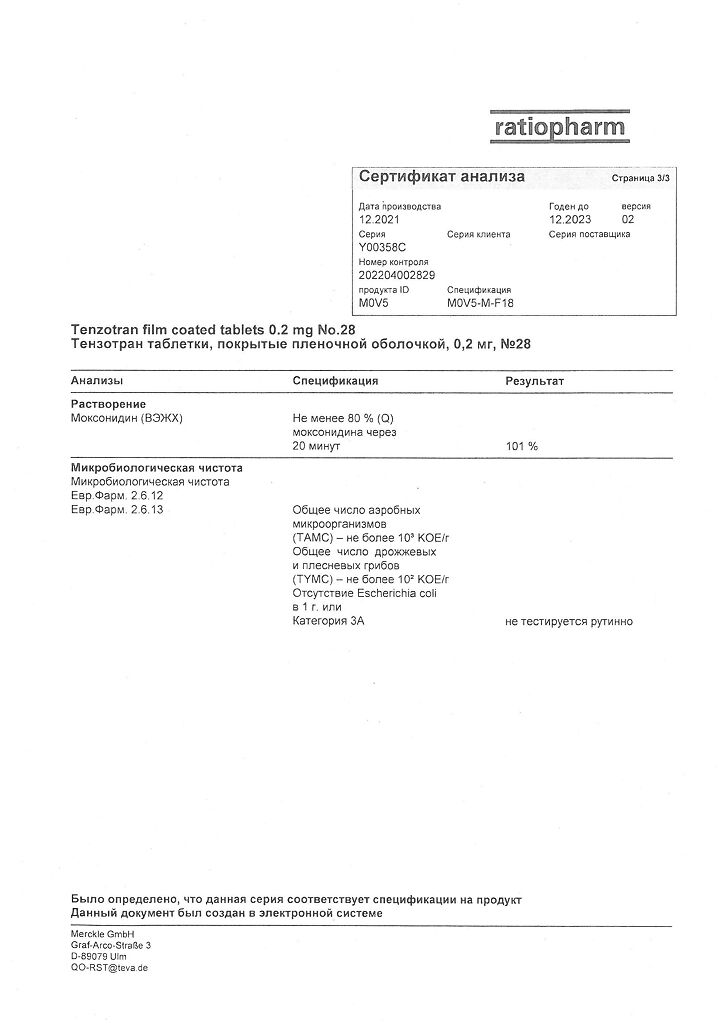
Storage conditions
Storage conditions
At a temperature not exceeding 30 °C
Shelf life
Shelf life
2 years
Manufacturer
Manufacturer
Merkle GmbH, Germany
Additional information
| Shelf life | 2 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 30 °C |
| Manufacturer | Merkle GmbH, Germany |
| Medication form | pills |
| Brand | Merkle GmbH |
Related products
Buy Tenzotran, 0.2 mg 28 pcs. with delivery to USA, UK, Europe and over 120 other countries.