No products in the cart.
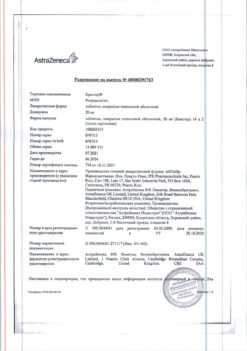
Telmista N, tablets 12.5mg+40 mg 84 pcs
€26.29 €21.91
Description
Pharmacotherapeutic group
Hypertensive combined (angiotensin II receptor antagonist + diuretic)/p> ATH code
C09DA07
Pharmacodynamics:
The drug Telmista® H is a combination of telmisartan (ARA II) and hydrochlorothiazide, a thiazide diuretic. Simultaneous use of these components leads to a more pronounced antihypertensive effect than the use of each of them separately.
The administration of Telmist® N once daily leads to a significant gradual decrease in blood pressure (BP).
Telmisartan
Telmisartan is a specific ARA II (AT1 subtype) effective when taken orally. It has high affinity for the AT1 subtype of angiotensin II receptors through which the action of angiotensin II is realized. It displaces angiotensin II from binding to the receptor without exhibiting agonist properties against this receptor. Telmisartan binds only to the AT1 subtype of angiotensin II receptor. The binding is long-lasting. It has no affinity for other receptors, including AT2 receptors and other less studied angiotensin receptors. The functional significance of these receptors as well as the effect of their possible overstimulation by angiotensin II, the concentration of which increases with telmisartan administration, has not been studied.
Telmisartan reduces plasma aldosterone concentrations does not inhibit plasma renin and does not block ion channels.
Telmisartan does not inhibit angiotensin-converting enzyme (ACE) (kininase II), an enzyme that also degrades bradykinin. Therefore, an increase in bradykinin-induced side effects is not expected.
In patients with arterial hypertension, telmisartan at a dose of 80 mg completely blocks the hypertensive effects of angiotensin II. The onset of antihypertensive action is noted within 3 hours after the first oral administration of telmisartan. The action of the drug persists for 24 hours and remains significant up to 48 hours.
A pronounced antihypertensive effect usually develops 4 weeks after regular use.
In patients with arterial hypertension, telmisartan reduces systolic and diastolic BP without affecting heart rate (HR).
In case of abrupt telmisartan withdrawal, BP gradually returns to baseline levels without development of “withdrawal” syndrome.
The study with telmisartan evaluated cardiovascular mortality of nonfatal myocardial infarction nonfatal stroke or hospitalization due to chronic heart failure (CHF). Cardiovascular morbidity and mortality in patients at high cardiovascular risk (with coronary artery disease stroke, peripheral artery disease or diabetes mellitus with concomitant target organ damage such as retinopathy left ventricular hypertrophy macro- or microalbuminuria in the history) over 55 years old have been shown to decrease.
Hydrochlorothiazide
Hydrochlorothiazide is a thiazide diuretic. Thiazide diuretics affect electrolyte reabsorption in the renal tubules directly by increasing sodium and chloride ion excretion (approximately equivalent amounts). Diuretic action of hydrochlorothiazide leads to decreased circulating blood volume (RBC), increased plasma renin activity, increased secretion of aldosterone with subsequent increase of urinary potassium and hydrocarbonate content and as a consequence reduction of plasma potassium content.
In concomitant administration with telmisartan there is a tendency to stop potassium loss caused by these diuretics presumably due to blockade of renin-angiotensin-aldosterone system (RAAS).
After oral administration, diuresis increases after 2 hours and the maximum effect is observed after about 4 hours. The diuretic effect of the drug lasts for about 6-12 hours.
Long-term use of hydrochlorothiazide reduces the risk of cardiovascular complications and mortality.
The maximal antihypertensive effect of the drug Telmist® N is usually achieved 4-8 weeks after the start of treatment.
Pharmacokinetics:
The concomitant use of telmisartan and hydrochlorothiazide has no effect on the pharmacokinetics of either component of the drug.
Telmisartan
It is rapidly absorbed from the gastrointestinal tract (GIT) when taken orally. Bioavailability is approximately 50%. Peak plasma concentrations occur approximately 05-15 hours later.
When taken concomitantly with food, the decrease in the area under the curve “concentration-time” (AUC) ranges from 6% (when taking a dose of 40 mg) to 19% (when taking a dose of 160 mg). In 3 hours after oral administration, plasma concentrations level off regardless of food intake. There is a difference in plasma concentrations of telmisartan in men and women.
The maximum plasma concentration (Cmax) and AUC are approximately 3 and 2 times higher in women compared to men, respectively, with no significant effect on efficacy. However, no enhancement of the antihypertensive effect is observed in women.
The binding to plasma proteins is significant (more than 995%) mainly with albumin and alpha1-acid glycoprotein. The volume of distribution is approximately 500 liters.
Telmisartan is metabolized by conjugation with glucuronic acid. Metabolites are pharmacologically inactive.
The elimination half-life (T1/2) is more than 20 hours. Excretion through the intestine unchanged kidney excretion is less than 2%. Total plasma clearance is high (about 900 ml/min).
Elderly patients
The pharmacokinetics of telmisartan in elderly patients does not differ from that in younger patients.
Dose adjustment is not required.
Patients with renal impairment
Telmisartan dose adjustment is not required in patients with renal impairment including those on hemodialysis.
Telmisartan is not eliminated by hemodialysis.
Patients with hepatic impairment
Pharmacokinetic studies in patients with hepatic impairment have shown increased absolute bioavailability of telmisartan to nearly 100%. In patients with hepatic insufficiency the T1/2 is not changed (see section “Dosage and administration”).
Hydrochlorothiazide
After oral administration of the drug Telmista® N the Cmax of hydrochlorothiazide in blood plasma is reached within 1-3 hours. Absolute bioavailability based on total renal excretion is about 60%. 64% of hydrochlorothiazide is bound by blood plasma proteins and the volume of distribution is 08±03 l/kg.
Hydrochlorothiazide is not metabolized in the body and is excreted by the kidneys almost unchanged. About 60% of the dose taken orally is eliminated within 48 hours. Renal clearance is about 250-300 ml/min. The T1/2 of hydrochlorothiazide is 10-15 hours. There is a difference in plasma concentrations in men and women.
In women the plasma concentration of telmisartan is 2-3 times higher than in men also in women there is a tendency to clinically insignificant increase in plasma concentration of hydrochlorothiazide.
Patients with renal impairment
In patients with impaired renal function the excretion rate of hydrochlorothiazide is reduced.
Studies conducted in patients with a creatinine clearance (CK) of 90 ml/min have shown that the T1/2 of hydrochlorothiazide is prolonged. In patients with decreased renal function, the T1/2 is about 34 hours.
Indications
Indications
Arterial hypertension (in case of ineffectiveness of telmisartan or hydrochlorothiazide in monotherapy).
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group
Combination antihypertensive drug (angiotensin II receptor antagonist + diuretic)
ATX code
C09DA07
Pharmacodynamics:
The drug Telmista® N is a combination of telmisartan (ARA II) and hydrochlorothiazide, a thiazide diuretic. The simultaneous use of these components leads to a more pronounced antihypertensive effect than the use of each of them separately.
Taking Telmista® N once a day leads to a significant gradual decrease in blood pressure (BP).
Telmisartan
Telmisartan is a specific ARA II (subtype AT1) effective when taken orally. It has a high affinity for the AT1 receptor subtype of angiotensin II through which the action of angiotensin II is realized. Displaces angiotensin II from its connection with the receptor without exhibiting agonist properties in relation to this receptor. Telmisartan binds only to the AT1 receptor subtype of angiotensin II. The connection is long-term. It has no affinity for other receptors, including AT2 receptors and other less studied angiotensin receptors. The functional significance of these receptors, as well as the effect of their possible excessive stimulation by angiotensin II, the concentration of which increases with the use of telmisartan, have not been studied.
Telmisartan reduces the concentration of aldosterone in the blood plasma, does not inhibit renin in the blood plasma and does not block ion channels.
Telmisartan does not inhibit angiotensin-converting enzyme (ACE) (kininase II), an enzyme that also destroys bradykinin. Therefore, an increase in the side effects caused by bradykinin is not expected.
In patients with arterial hypertension, telmisartan at a dose of 80 mg completely blocks the hypertensive effect of angiotensin II. The onset of antihypertensive action is observed within 3 hours after the first oral administration of telmisartan. The effect of the drug lasts for 24 hours and remains significant for up to 48 hours.
A pronounced antihypertensive effect usually develops 4 weeks after regular use of the drug.
In patients with arterial hypertension, telmisartan reduces systolic and diastolic blood pressure without affecting heart rate (HR).
In case of abrupt withdrawal of telmisartan, blood pressure gradually returns to its original level without the development of withdrawal syndrome.
The telmisargan study assessed the incidence of cardiovascular mortality, nonfatal myocardial infarction, nonfatal stroke, or hospitalization due to chronic heart failure (CHF). A reduction in cardiovascular morbidity and mortality has been proven in patients at high cardiovascular risk (with coronary artery disease, stroke, peripheral artery disease, or diabetes mellitus with concomitant target organ damage such as retinopathy, left ventricular hypertrophy, macro- or microalbuminuria in history) over the age of 55 years.
Hydrochlorothiazide
Hydrochlorothiazide is a thiazide diuretic. Thiazide diuretics affect the reabsorption of electrolytes in the renal tubules by directly increasing the excretion of sodium and chloride ions (in approximately equivalent quantities). The diuretic effect of hydrochlorothiazide leads to a decrease in circulating blood volume (CBV), an increase in plasma renin activity, an increase in the secretion of aldosterone, followed by an increase in the content of potassium and bicarbonates in the urine and, as a consequence, a decrease in the potassium content in the blood plasma.
When taken concomitantly with telmisartan, there is a tendency to stop the loss of potassium caused by these diuretics, presumably due to blockade of the renin-angiotensin-aldosterone system (RAAS).
After oral administration, diuresis increases after 2 hours and the maximum effect is observed after approximately 4 hours. The diuretic effect of the drug lasts for approximately 6-12 hours.
Long-term use of hydrochlorothiazide reduces the risk of complications of cardiovascular diseases and mortality from them.
The maximum antihypertensive effect of Telmista® N is usually achieved 4-8 weeks after the start of treatment.
Pharmacokinetics:
The simultaneous use of telmisartan and hydrochlorothiazide does not affect the pharmacokinetics of each of the components of the drug.
Telmisartan
When taken orally, it is quickly absorbed from the gastrointestinal tract (GIT). Bioavailability is approximately 50%. Peak concentrations in blood plasma occur approximately after 05-15 hours.
When taken concomitantly with food, the reduction in area under the concentration-time curve (AUC) ranges from 6% (with a 40 mg dose) to 19% (with a 160 mg dose). 3 hours after oral administration, the concentration in the blood plasma levels off regardless of food intake. There is a difference in plasma concentrations of telmisartan in men and women.
The maximum plasma concentration (Cmax) and AUC are approximately 3 and 2 times higher, respectively, in women compared to men, without a significant effect on efficacy. However, an increase in the antihypertensive effect is not observed in women.
The binding to plasma proteins is significant (more than 995%), mainly with albumin and alpha1-acid glycoprotein. Distribution volume approx. 500 l.
Telmisartan is metabolized by conjugation with glucuronic acid. Metabolites are pharmacologically inactive.
The half-life (T1/2) is more than 20 hours. Excreted unchanged through the intestines, excretion by the kidneys is less than 2%. The total plasma clearance is high (about 900 ml/min).
Elderly patients
The pharmacokinetics of telmisartan in elderly patients does not differ from the pharmacokinetics in young patients.
No dose adjustment is required.
Patients with renal failure
No dose adjustment of telmisartan is required in patients with renal failure, including patients on hemodialysis.
Telmisartan is not removed by hemodialysis.
Patients with liver failure
Pharmacokinetic studies in patients with liver failure showed an increase in the absolute bioavailability of telmisartan to almost 100%. In case of liver failure, T1/2 does not change (see section “Method of administration and dosage”).
Hydrochlorothiazide
After oral administration of the drug Telmista® N, Cmax of hydrochlorothiazide in the blood plasma is achieved within 1-3 hours. Absolute bioavailability based on total renal excretion is approximately 60%. 64% of hydrochlorothiazide is bound by blood plasma proteins and the volume of distribution is 08±03 l/kg.
Hydrochlorothiazide is not metabolized in the body and is excreted by the kidneys almost unchanged. About 60% of the dose taken orally is eliminated within 48 hours. Renal clearance is about 250-300 ml/min. T1/2 of hydrochlorothiazide is 10-15 hours. There is a difference in plasma concentrations between men and women.
In women, the concentration of telmisartan in the blood plasma is 2-3 times higher than in men; also in women there is a tendency to a clinically insignificant increase in the concentration of hydrochlorothiazide in the blood plasma.
Patients with renal failure
In patients with impaired renal function, the rate of elimination of hydrochlorothiazide is reduced.
Studies conducted in patients with creatinine clearance (CC) 90 ml/min showed that T1/2 of hydrochlorothiazide is prolonged. In patients with reduced renal function, T1/2 is about 34 hours.
Special instructions
Special instructions
· Bilateral renal artery stenosis or stenosis of the artery of a single kidney (see section “Special instructions”).
· Impaired liver function or progressive liver disease (class A and B according to the Child-Pugh classification) (see section “Special instructions”).
· Decrease in blood volume due to previous diuretic therapy, restriction of salt intake, diarrhea or vomiting.
· Hyperkalemia.
· Condition after kidney transplantation (no experience of use).
· Chronic heart failure III-IV functional class (FC) according to the New York Heart Association (NYHA) classification.
· Hypercalcemia.
· Hypercholesterolemia.
· Hypertriglyceridemia.
· Hypokalemia.
· Hyponatremia.
· Concomitant use of drugs that can cause polymorphic ventricular tachycardia of the “pirouette” type or increase the duration of the QT interval on the ECG.
· Simultaneous use of lithium preparations, drugs that can cause hypokalemia, cardiac glycosides.
· Hyperparathyroidism.
· Old age.
· Coronary heart disease (CHD).
· Progressive liver diseases (risk of developing hepatic coma).
· Stenosis of the aortic and/or mitral valve.
· Idiopathic hypertrophic subaortic stenosis.
· Hypertrophic obstructive cardiomyopathy (HOCM).
· Diabetes mellitus.
· Primary hyperaldosteronism.
· Gout, hyperuricemia.
· Systemic lupus erythematosus.
· History of an allergic reaction to penicillin.
· History of non-melanoma skin cancer (NMSC) (see section “Special instructions”).
· Use in patients of the Negroid race.
· Experience in patients with renal failure (creatinine clearance more than 30 ml/min) is limited, but does not confirm the development of side effects from the kidneys, and dose adjustment is not required.
Contraindicated in persons under 18 years of age as efficacy and safety have not been established.
Renal dysfunction
The limited experience with the use of the combination of hydrochlorothiazide + telmisartan in patients with mild or moderate renal impairment does not require a change in the dose of the drug in these cases. In such patients, renal function should be monitored (for use with CC less than 30 ml/min, see section “Contraindications”).
Liver dysfunction
In patients with mild to moderate liver dysfunction (class A and B according to the Child-Pugh classification), the daily dose of Telmista® H should not exceed the dose of hydrochlorothiazide 12.5 mg and telmisartan 40 mg per day (see section “Pharmacological properties. Pharmacokinetics”).
Elderly patients
The dosage regimen does not require changes.
The use of Telmista® N in patients with acute myocardial infarction is not recommended due to insufficient experience in clinical use.
The drug Telmista® N should not be used to relieve a hypertensive crisis.
Hydrochlorothiazide
Renal dysfunction
In patients with impaired renal function, hydrochlorothiazide may cause azotemia. In case of renal failure, accumulation of hydrochlorothiazide is possible.
In patients with reduced renal function, periodic monitoring of CK is necessary. If renal dysfunction progresses and/or oliguria (anuria) occurs, hydrochlorothiazide should be discontinued.
Liver dysfunction
When using thiazide diuretics in patients with impaired liver function, hepatic encephalopathy may develop. In patients with severe liver failure or hepatic encephalopathy, the use of thiazides is contraindicated. In patients with mild to moderate hepatic impairment and/or progressive liver disease, hydrochlorothiazide should be used with caution, since even a slight change in fluid and electrolyte balance and the accumulation of ammonium in the blood serum can cause hepatic coma. If symptoms of encephalopathy occur, diuretics should be discontinued immediately.
Water-electrolyte balance and metabolic disorders
Thiazide diuretics (including hydrochlorothiazide) can cause a decrease in blood volume (hypovolemia) and disturbances in water and electrolyte balance (including hypokalemia, hyponatremia, hypochloremic alkalosis).
Clinical symptoms of water and electrolyte imbalance are dryness of the oral mucosa, thirst, weakness, lethargy, fatigue, drowsiness, anxiety, muscle pain or cramps, muscle weakness, marked decrease in blood pressure, oliguria, tachycardia, arrhythmia and gastrointestinal disorders (such as nausea and vomiting). In patients receiving hydrochlorothiazide therapy (especially with long-term course treatment), clinical symptoms of water-electrolyte imbalance should be identified and the content of electrolytes in the blood plasma should be regularly monitored.
Sodium
All diuretics can cause hyponatremia, sometimes leading to severe complications. Hyponatremia and hypovolemia can lead to dehydration and orthostatic hypotension. A concomitant decrease in plasma chlorine content can lead to secondary compensatory metabolic alkalosis, but the frequency and severity of this effect are insignificant. It is recommended to determine the sodium content in the blood plasma before starting treatment and regularly monitor this indicator while taking hydrochlorothiazide.
Potassium
When using thiazide and thiazide-like diuretics, there is a risk of a sharp decrease in the potassium content in the blood plasma and the development of hypokalemia (potassium content in the blood plasma less than 3.4 mmol/l). Hypokalemia increases the risk of developing heart rhythm disturbances (including severe arrhythmias) and enhances the toxic effect of cardiac glycosides. In addition, hypokalemia (as well as bradycardia) is a condition that contributes to the development of polymorphic ventricular tachycardia of the “pirouette” type, which can be fatal.
Hypokalemia poses the greatest danger to the following groups of patients: elderly people, patients simultaneously receiving therapy with antiarrhythmic and non-antiarrhythmic drugs that can cause polymorphic ventricular tachycardia of the “pirouette” type or increase the duration of the QT interval on the ECG, patients with impaired liver function, coronary artery disease, and heart failure. In addition, patients with an increased QT interval are at increased risk. It does not matter whether this increase is caused by congenital causes or the effect of drugs.
In all the cases described above, it is necessary to avoid the risk of developing hypokalemia and regularly monitor the potassium content in the blood plasma. The first determination of potassium content in blood plasma should be carried out within the first week from the start of treatment. If hypokalemia occurs, appropriate treatment should be prescribed. Hypokalemia can be corrected by using potassium-containing medications or eating foods rich in potassium (dried fruits, fruits, vegetables).
Calcium
Thiazide diuretics may reduce the excretion of calcium ions by the kidneys, leading to a slight and temporary increase in plasma calcium levels. In some patients, with long-term use of thiazide diuretics, pathological changes in the parathyroid glands with hypercalcemia and hyperphosphatemia were observed, but without the typical complications of hyperparathyroidism (nephrolithiasis, decreased bone mineral density, peptic ulcer). Severe hypercalcemia may be a manifestation of previously undiagnosed hyperparathyroidism.
Because of their effect on calcium metabolism, thiazides may interfere with laboratory parameters of parathyroid function. Thiazide diuretics (including hydrochlorothiazide) should be discontinued before testing parathyroid function.
Magnesium
Thiazides have been found to increase the excretion of magnesium ions by the kidneys, which can lead to hypomagnesemia. The clinical significance of hypomagnesemia remains unclear.
Glucose
Treatment with thiazide diuretics may impair glucose tolerance. When using hydrochlorothiazide in patients with manifest or latent diabetes mellitus, it is necessary to regularly monitor the concentration of glucose in the blood. Dosage adjustment of hypoglycemic medications may be required.
Uric acid
In patients with gout, the frequency of attacks may increase or the course of gout may worsen. Careful monitoring of patients with gout and impaired uric acid metabolism (hyperuricemia) is necessary.
Lipids
When using hydrochlorothiazide, the concentration of cholesterol and triglycerides in the blood plasma may increase.
Acute myopia/secondary angle-closure glaucoma
Hydrochlorothiazide can cause an idiosyncratic reaction leading to the development of acute myopia and an acute attack of secondary angle-closure glaucoma. Symptoms include: sudden loss of vision or eye pain, usually occurring within hours to weeks of starting hydrochlorothiazide therapy. If left untreated, acute angle-closure glaucoma can lead to irreversible vision loss. If symptoms appear, you should stop taking hydrochlorothiazide as soon as possible. If intraocular pressure remains uncontrolled, emergency medical treatment or surgery may be required. Risk factors for the development of acute angle-closure glaucoma are: a history of an allergic reaction to sulfonamides or penicillin.
Immune system disorders
There are reports that thiazide diuretics (including hydrochlorothiazide) may cause exacerbation or progression of systemic lupus erythematosus, as well as lupus-like reactions.
In patients receiving thiazide diuretics, hypersensitivity reactions may occur even in the absence of a history of allergic reactions or bronchial asthma.
Photosensitivity
There is information about cases of the development of photosensitivity reactions when taking thiazide diuretics. If photosensitivity occurs while taking hydrochlorothiazide, treatment should be discontinued. If continued use of the diuretic is necessary, the skin should be protected from exposure to sunlight or artificial ultraviolet (UV) rays.
NMRK
Two pharmacoepidemiological studies using data from the Danish National Cancer Registry demonstrated an association between hydrochlorothiazide use and an increased risk of NMSC basal cell carcinoma and squamous cell carcinoma. The risk of developing NMSC increased with increasing total (cumulative) dose of hydrochlorothiazide. A possible mechanism for the development of NMSC is the photosensitizing effect of hydrochlorothiazide.
Patients taking hydrochlorothiazide as monotherapy or in combination with other drugs should be aware of the risk of developing NMSC. It is recommended that such patients undergo regular skin examination to identify any new suspicious lesions as well as changes in existing skin lesions.
Any suspicious skin changes should be reported to your doctor immediately. Suspicious areas of skin should be examined by a specialist. To clarify the diagnosis, histological examination of skin biopsies may be required.
To minimize the risk of developing NMSC, patients should be advised to follow preventive measures, such as limiting exposure to sunlight and UV rays, and using appropriate protective equipment.
In patients with a history of NMSC, it is recommended to reconsider the use of hydrochlorothiazide.
Alcohol
During the treatment period, it is not recommended to drink alcoholic beverages, since ethanol enhances the antihypertensive effect of thiazide diuretics.
Athletes
Hydrochlorothiazide may give a positive result during doping control in athletes.
Other
In patients with severe atherosclerosis of the cerebral and coronary arteries, hydrochlorothiazide should be used with extreme caution.
Thiazide diuretics can reduce the amount of iodine bound to plasma proteins without causing signs of thyroid dysfunction.
Telmisartan
Liver failure
Telmisartan should not be used in patients with cholestasis, biliary obstruction or severe hepatic impairment (Child-Pugh class C). since telmisartan is excreted mainly in bile. It is assumed that in such patients the hepatic clearance of telmisartan is reduced.
Renovascular hypertension
When treated with drugs that act on the RAAS, the risk of severe arterial hypotension and renal failure increases in patients with bilateral renal artery stenosis or stenosis of the artery of a solitary kidney.
Double blockade of the RAAS
Data on the simultaneous use of ACE inhibitors with ARB II or drugs containing aliskiren confirm an increased risk of a sharp decrease in blood pressure, the development of hyperkalemia and impaired renal function (including acute renal failure).
Concomitant use of ARB II, including telmisartan, with drugs containing aliskiren is contraindicated in patients with diabetes mellitus and/or with moderate or severe renal impairment (GFR less than 60 ml/min/1.73 m2 body surface area) and is not recommended in other patients.
Concomitant use of II receptor antagonists, including telmisartan, with ACE inhibitors is contraindicated in patients with diabetic nephropathy and is not recommended in other patients.
If it is necessary to carry out double blockade of the RAAS, each case should be considered individually and carefully monitor renal function, fluid and electrolyte balance and blood pressure levels.
Other diseases characterized by stimulation of the RAAS
In patients whose vascular tone and renal function depend primarily on the activity of the RAAS (for example, patients with CHF or kidney disease, including renal artery stenosis), the use of drugs acting on this system, such as telmisartan, has been associated with the occurrence of acute arterial hypotension, hyperazotemia, oliguria, or rarely with acute renal failure.
Primary hyperaldosteronism
Patients with primary hyperaldosteronism generally do not respond to treatment with antihypertensive drugs that act by inhibiting the RAAS. In this regard, the use of telmisartan in these cases is not recommended.
Kidney failure and kidney transplantation
There is no clinical experience with the use of telmisartan in patients who have recently undergone kidney transplantation.
Decrease in BCC
In patients with a decrease in blood volume and/or sodium content in the blood plasma due to previous diuretic therapy, restriction of salt intake, diarrhea or vomiting, symptomatic arterial hypotension may occur, especially after the first dose of telmisartan.
Aortic and mitral valve stenosis, HOCM
As with the use of other vasodilators, caution should be exercised when prescribing the drug to patients with aortic or mitral valve stenosis or HOCM.
Hyperkalemia
Telmisartan may cause hyperkalemia due to antagonism of angiotensin II receptors (AT1 subtype). For elderly patients, patients with renal failure, patients with diabetes mellitus and also with arterial hypertension and coronary artery disease, patients receiving concomitant therapy with drugs that can cause an increase in potassium levels, and/or patients with concomitant disease, hyperkalemia can be fatal. Before considering the possibility of concomitant use of drugs acting on the RAAS, it is necessary to assess the benefit-risk ratio. The main risk factors to consider are:
· diabetes mellitus, renal failure, heart failure, old age (patients over 70 years old);
· combination with one or more drugs acting on the RAAS and/or nutritional supplements containing potassium. Medicines that can cause hyperkalemia are potassium-sparing diuretics, ACE inhibitors, ARB II, NSAIDs, including selective COX-2 inhibitors, heparin, immunosuppressants (cyclosporine or tacrolimus), trimethoprim, and salt substitutes containing potassium;
· concomitant diseases or conditions, especially dehydration, acute heart failure, metabolic acidosis, impaired renal function, acute renal failure (for example, in infectious diseases), cytolysis syndrome (for example, acute limb ischemia, rhabdomyolysis, major trauma).
Active ingredient
Active ingredient
Hydrochlorothiazide, Telmisartan
Composition
Composition
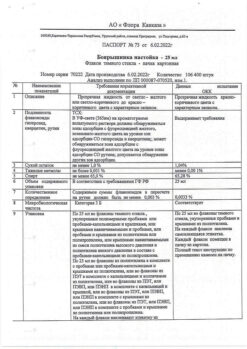
Active ingredients:
Hydrochlorothiazide 12.50 mg/12.50 mg/25.00 mg
Telmisartan 40.00 mg/80.00 mg/80.00 mg
Excipients:
Meglumine, sodium hydroxide, povidone-K30, lactose monohydrate, sorbitol, magnesium stearate, mannitol, mannitol DC, yellow iron oxide dye (E172) (for 25 mg + 80 mg tablets), red iron oxide dye (E172) (for 12.5 mg + 40 mg and 12.5 mg + 80 mg tablets), hyprolose, colloidal silicon dioxide, sodium stearyl fumarate
Pregnancy
Pregnancy
The use of Telmista® H during pregnancy is contraindicated.
Hydrochlorothiazide
Experience with the use of hydrochlorothiazide during pregnancy, especially in the first trimester, is limited.
Hydrochlorothiazide penetrates the placental barrier. Given the mechanism of pharmacological action of hydrochlorothiazide, it is assumed that its use in the second and third trimesters of pregnancy may disrupt fetoplacental perfusion and cause changes in the embryo and fetus such as jaundice, water-electrolyte imbalance and thrombocytopenia.
Hydrochlorothiazide should not be used for edema in pregnancy, hypertension in pregnancy or pre-eclampsia, as there is a risk of decreased plasma volume and decreased placental perfusion, and there is no beneficial effect in these clinical situations.
Hydrochlorothiazide should not be used to treat essential hypertension in pregnancy, except in rare situations where other treatments cannot be used.
Telmisartan
The use of ARA II in the first trimester of pregnancy is not recommended; these drugs should not be prescribed during pregnancy. If pregnancy is diagnosed, the drug should be stopped immediately. If necessary, alternative therapy should be prescribed (other classes of antihypertensive drugs approved for use during pregnancy).
The use of ARA II in the second and third trimesters of pregnancy is contraindicated. In preclinical studies studying the use of telmisartan, a teratogenic effect was not noted, but fetotoxicity was established. It is known that exposure to ARA II in the second and third trimesters of pregnancy causes fetotoxicity in humans (decreased renal function, oligohydramnios, delayed ossification of the skull bones), as well as neonatal toxicity (renal failure, arterial hypotension, hyperkalemia). Patients planning pregnancy should be prescribed alternative therapy with a proven safety profile for use in pregnant women. If treatment with ARA II occurred in the second trimester of pregnancy, ultrasound examination of the fetal kidneys and skull bones is recommended.
Newborns whose mothers received ARA II should be closely monitored for hypotension.
Therapy with Telmista® H is contraindicated during breastfeeding.
In animal studies, no effect of telmisartan and hydrochlorothiazide on fertility was observed.
No studies have been conducted to study the effect on human fertility.
Contraindications
Contraindications
· Hypersensitivity to the active substances or auxiliary components of the drug, or other sulfonamide derivatives.
· Pregnancy.
· Breastfeeding period.
· Obstructive diseases of the biliary tract.
· Severe liver dysfunction (class C according to the Child-Pugh classification).
· Severe renal dysfunction (creatinine clearance less than 30 ml/min).
· Refractory hypokalemia, hypercalcemia.
· Concomitant use with aliskiren and drugs containing aliskiren in patients with diabetes mellitus and/or moderate or severe renal impairment (glomerular filtration rate [GFR] less than 60 ml/min/1.73 m2 body surface area).
· Concomitant use with ACE inhibitors in patients with diabetic nephropathy.
· Fructose or lactose intolerance, lactase deficiency, glucose-galactose malabsorption syndrome, since the drug Telmista® H contains lactose and sorbitol.
· Children under 18 years of age (efficacy and safety have not been established).
Interaction
Interaction
Hydrochlorothiazide
Not recommended drug combinations
Lithium preparations
With the simultaneous use of hydrochlorothiazide and lithium preparations, the renal clearance of lithium is reduced, which can lead to an increase in the concentration of lithium in the blood plasma and an increase in its toxicity. If concomitant use of hydrochlorothiazide is necessary, the dose of lithium preparations should be carefully selected, the concentration of lithium in the blood plasma should be regularly monitored and the dose of the drug should be adjusted accordingly.
Combinations of drugs requiring special attention
Drugs that can cause polymorphic ventricular tachycardia of the “pirouette” type
Hydrochlorothiazide should be used with extreme caution concomitantly with drugs such as:
antiarrhythmic drugs of class IA (quinidine, hydroquinidine, disopyramide, procainamide) and class IC (flecainide);
class III antiarrhythmic drugs (dofetilide, ibutilide, bretylium tosylate), sotalol, dronedarone, amiodarone;
other (non-antiarrhythmic) medicines such as:
– neuroleptics: phenothiazines (chlorpromazine, cyamemazine, levomepromazine, thioridazine, trifluoperazine, fluphenazine), benzamides (amisulpride, sultopride, sulpiride, tiapride), butyrophenones (droperidol, haloperidol), pimozide, sertindole;
– antidepressants: tricyclic antidepressants, selective serotonin reuptake inhibitors (SSRIs) (citalopram, escitalopram);
– antibacterial agents: fluoroquinolones (levofloxacin, moxifloxacin, sparfloxacin, ciprofloxacin), macrolides (erythromycin for intravenous administration, azithromycin, clarithromycin, roxithromycin, spiramycin), co-trimoxazole;
– antifungals: azoles (voriconazole, itraconazole, ketoconazole, fluconazole);
– antimalarials (quinine, chloroquine, mefloquine, halofantrine, lumefantrine);
– antiprotozoal drugs (pentamidine for parenteral administration);
– antianginal drugs (ranolazine, bepridil);
– antitumor agents (vandetanib, arsenic trioxide, oxaliplatin, tacrolimus);
– antiemetics (domperidone, ondansetron);
– drugs affecting gastrointestinal motility (cisapride);
– antihistamines (astemizole, terfenadine, mizolastine);
– other medicines (anagrelide, vasopressin, difemanil methyl sulfate, ketanserin, probucol, propofol, sevoflurane, terlipressin, terodiline, cilostazol).
Due to the increased risk of ventricular arrhythmias, especially polymorphic ventricular tachycardia of the “pirouette” type (risk factor – hypokalemia), the potassium content in the blood plasma should be determined and, if necessary, adjusted before starting combination therapy with hydrochlorothiazide with the above drugs. It is necessary to monitor the patient’s clinical condition, blood plasma electrolyte levels and ECG parameters. In patients with hypokalemia, it is necessary to use drugs that do not cause polymorphic ventricular tachycardia of the “pirouette” type.
Medicines that can prolong the QT interval
The simultaneous use of hydrochlorothiazide with drugs that can prolong the QT interval should be based on a careful assessment for each patient of the expected benefit versus the potential risk (possible increased risk of developing torsade de pointes (TdP). When using such combinations, it is necessary to regularly record an ECG (to detect prolongation of the QT interval), as well as monitor potassium levels in the blood plasma.
Drugs that can cause hypokalemia: amphotericin B (when administered intravenously), gluco- and mineralocorticosteroids (when used systemically), tetracosactide (adrenocorticotropic hormone [ACTH]), glycyrrhizic acid (carbenoxolone, preparations containing licorice root), laxatives that stimulate intestinal motility
Increased risk of hypokalemia when used simultaneously with hydrochlorothiazide (additive effect). Regular monitoring of the potassium content in the blood plasma is necessary, and, if necessary, its correction. During therapy with hydrochlorothiazide, it is recommended to use laxatives that do not stimulate intestinal motility.
Cardiac glycosides
Hypokalemia and hypomagnesemia caused by the action of thiazide diuretics increase the toxicity of cardiac glycosides. When using hydrochlorothiazide and cardiac glycosides simultaneously, you should regularly monitor the potassium content in the blood plasma, ECG readings and, if necessary, adjust therapy.
Drug combinations requiring attention
Other antihypertensive drugs
Potentiation of the antihypertensive effect of hydrochlorothiazide (additive effect). It may be necessary to adjust the dose of concomitantly prescribed antihypertensive drugs.
Ethanol, barbiturates, antipsychotics (neuroleptics), antidepressants, anxiolytics, narcotic analgesics and general anesthesia
It is possible to enhance the antihypertensive effect of hydrochlorothiazide and potentiate orthostatic hypotension (additive effect).
Non-depolarizing muscle relaxants (eg, tubocurarine)
The effect of non-depolarizing muscle relaxants may be enhanced.
Adrenergic agonists (pressor amines)
Hydrochlorothiazide may reduce the effect of adrenergic agonists such as epinephrine (adrenaline) and norepinephrine (norepinephrine).
Nonsteroidal anti-inflammatory drugs (NSAIDs), including selective cyclooxygenase-2 (COX-2) inhibitors and high doses of acetylsalicylic acid (≥ 3 g/day)
NSAIDs may reduce the diuretic and antihypertensive effects of hydrochlorothiazide. With simultaneous use, there is a risk of developing acute renal failure due to a decrease in GFR. Hydrochlorothiazide may enhance the toxic effects of high doses of salicylates on the central nervous system.
Oral hypoglycemic agents and insulin
Thiazide diuretics affect glucose tolerance (hyperglycemia may develop) and reduce the effectiveness of hypoglycemic agents (dose adjustment of hypoglycemic agents may be required).
Hydrochlorothiazide and metformin should be used concomitantly with caution due to the risk of lactic acidosis due to renal impairment caused by hydrochlorothiazide.
Beta blockers, diazoxide
Concomitant use of thiazide diuretics (including hydrochlorothiazide) with beta-blockers or diazoxide may increase the risk of hyperglycemia.
Medicines used to treat gout (probenecid, sulfinpyrazone, allopurinol)
Dose adjustment of uricosuric drugs may be required as hydrochlorothiazide increases serum uric acid concentrations. Thiazide diuretics may increase the incidence of hypersensitivity reactions to allopurinol.
Amantadine
Thiazide diuretics (including hydrochlorothiazide) may reduce the clearance of amantadine, lead to increased plasma concentrations of amantadine and increase the risk of adverse effects.
Anticholinergic drugs (cholinergic blockers)
Anticholinergic drugs (eg, atropine, biperiden) increase the bioavailability of thiazide diuretics by reducing gastrointestinal motility and the rate of gastric emptying.
Cytotoxic (antitumor) drugs
Thiazide diuretics reduce the renal excretion of cytotoxic drugs (for example, cyclophosphamide and methotrexate) and potentiate their myelosuppressive effects.
Methyldopa
Cases of hemolytic anemia have been described with the simultaneous use of hydrochlorothiazide and methyldopa
Antiepileptic drugs (carbamazepine, oxcarbazepine, topiramate)
Risk of developing symptomatic hyponatremia. When using hydrochlorothiazide and carbamazepine simultaneously, it is necessary to monitor the patient’s condition and monitor the sodium level in the blood serum. When using hydrochlorothiazide and topiramate simultaneously, the level of topiramate in the blood serum should also be monitored, and if necessary, prescribe potassium supplements or adjust the dose of topiramate.
SSRIs
When used simultaneously with thiazide diuretics, hyponatremia may be potentiated. Monitoring of sodium levels in blood plasma is necessary.
Cyclosporine
With simultaneous use of thiazide diuretics and cyclosporine, the risk of developing hyperuricemia and exacerbation of gout increases.
Oral anticoagulants
Thiazide diuretics may reduce the effect of oral anticoagulants.
Iodinated contrast agents
Dehydration while taking thiazide diuretics increases the risk of developing acute renal failure, especially when using high doses of iodinated contrast agents. Before using iodinated contrast agents, it is necessary to compensate for fluid loss.
Calcium preparations
With simultaneous use, it is possible to increase the calcium content in the blood plasma and develop hypercalcemia due to a decrease in the excretion of calcium ions by the kidneys. If simultaneous administration of calcium-containing drugs is necessary, the calcium level in the blood plasma should be monitored and the dose of calcium supplements should be adjusted.
Anion exchange resins (cholestyramine and colestipol)
Anion exchange resins reduce the absorption of hydrochlorothiazide. Single doses of cholestyramine and colestipol reduce the absorption of hydrochlorothiazide in the gastrointestinal tract by 85% and 43%, respectively.
Telmisartan
With simultaneous use of telmisartan with:
· other antihypertensive drugs may enhance the antihypertensive effect. In one study, with the combined use of telmisartan and ramipril, an increase in AUC0-24 and Cmax of ramipril and ramiprilat in blood plasma was observed by 2.5 times. The clinical significance of this interaction has not been established.
In the analysis of adverse events leading to discontinuation of treatment and the analysis of serious adverse events obtained during the clinical trial, it was found that cough and angioedema were observed more often during therapy with ramipril, while arterial hypotension occurred more often during therapy with telmisartan. Cases of hyperkalemia, renal failure, arterial hypotension and syncope were observed significantly more often with simultaneous use of telmisartan and ramipril;
· with lithium preparations, a reversible increase in the lithium content in the blood plasma was observed, accompanied by toxic effects when taking ACE inhibitors. In rare cases, such changes have been reported with the administration of ARA II, in particular telmisartan. When using lithium preparations and ARA II simultaneously, it is recommended to determine the lithium content in the blood plasma;
· NSAIDs, including acetylsalicylic acid in doses used as an anti-inflammatory agent, cyclooxygenase-2 (COX-2) inhibitors and non-selective NSAIDs, can cause the development of acute renal failure in patients with reduced blood volume. Drugs that affect the renin-angiotensin-aldosterone system (RAAS) may have a synergistic effect. In patients simultaneously using NSAIDs and telmisartan, blood volume should be compensated and renal function monitored at the beginning of treatment.
A decrease in the effect of antihypertensive agents, such as telmisartan, through inhibition of the vasodilatory effect of prostaglandins has been observed during concomitant treatment with NSAIDs. When telmisartan was used simultaneously with ibuprofen or paracetamol, no clinically significant effect was observed;
Digoxin, warfarin, hydrochlorothiazide, glibenclamide, simvastatin and amlodipine have not revealed any clinically significant interactions. There was an increase in the average concentration of digoxin in the blood plasma by an average of 20% (in one case by 39%). With the simultaneous use of telmisartan and digoxin, it is advisable to periodically determine the concentration of digoxin in the blood plasma;
· aliskiren, aliskiren-containing drugs, clinical data have shown that double blockade of the RAAS through the simultaneous use of ACE inhibitors, ARA II and aliskiren is associated with a high incidence of side effects, such as arterial hypotension, hyperkalemia, decreased renal function (including acute renal failure) compared with the use of a single RAAS activity blocker. The simultaneous use of ARA II with drugs containing aliskiren is contraindicated in patients with diabetes mellitus and/or with moderate or severe renal impairment (GFR less than 60 ml/min/1.73 m2 body surface area) and is not recommended in other patients. Concomitant use of ARB II and ACE inhibitors is contraindicated in patients with diabetic nephropathy and is not recommended in other patients;
drugs that can cause hyperkalemia
Like other drugs acting on the RAAS, telmisartan may pose a risk of developing hyperkalemia. The risk may be increased in case of concomitant use with other drugs that can cause hyperkalemia (salt substitutes containing potassium, potassium-sparing diuretics [spironolactone, eplerenone, triamterene or amiloride], ACE inhibitors, ARB II and NSAIDs, including selective COX-2 inhibitors, heparin, immunosuppressants [cyclosporine, tacrolimus and trimethoprim]). Caution should be exercised during simultaneous use and periodic monitoring of potassium levels in the blood plasma;
Diuretics (thiazide or loop)
Previous treatment with high doses of diuretics, such as furosemide (loop diuretic) and hydrochlorothiazide (thiazide diuretic), may lead to hypovolemia and the risk of hypotension when starting treatment with telmisartan;
· corticosteroids (for systemic use)
Corticosteroids weaken the antihypertensive effect of telmisartan.
Overdose
Overdose
Information on overdose is limited.
Hydrochlorothiazide
Symptoms
The most common manifestations of an overdose of hydrochlorothiazide are an increase in diuresis, accompanied by acute loss of fluid (dehydration) and electrolyte disturbances (hypokalemia, hyponatremia, hypochloremia). An overdose of hydrochlorothiazide may be manifested by the following symptoms:
from the cardiovascular system: tachycardia, decreased blood pressure, shock;
from the nervous system: weakness, confusion, dizziness and spasms of the calf muscles, paresthesia, disturbances of consciousness, fatigue;
from the gastrointestinal tract: nausea, vomiting, thirst;
from the kidneys and urinary tract: polyuria, oliguria or anuria (due to hemoconcentration);
laboratory parameters: hypokalemia, hyponatremia, hypochloremia, alkalosis, increased concentration of residual urea nitrogen in the blood plasma (especially in patients with renal failure).
Treatment
In case of overdose, symptomatic and supportive therapy is provided. If hydrochlorothiazide has recently been taken, induction of vomiting or gastric lavage is indicated to remove it. The absorption of hydrochlorothiazide can be reduced by oral administration of activated charcoal. In case of a decrease in blood pressure or shock, the bcc should be replenished with the introduction of plasma replacement fluids and a deficiency of electrolytes (potassium, sodium). In case of respiratory failure, oxygen inhalation or artificial ventilation is indicated. Water and electrolyte balance (especially serum potassium levels) and renal function should be monitored until they return to normal.
There is no specific antidote. Hydrochlorothiazide is eliminated by hemodialysis, but the extent of its elimination has not been established.
Telmisartan
Symptoms
The most pronounced manifestations of overdose were an excessive decrease in blood pressure and tachycardia, and bradycardia, dizziness, increased serum creatinine concentrations and acute renal failure were also reported.
Treatment
Telmisartan is not eliminated by hemodialysis. Patients should be carefully monitored and treated symptomatically as well as supportively. The treatment approach depends on the time elapsed after taking the drug and the severity of symptoms. Recommended measures include inducing vomiting and/or gastric lavage; it is advisable to take activated charcoal. Electrolyte levels and plasma creatinine concentrations should be regularly monitored. If a pronounced decrease in blood pressure occurs, the patient should take a horizontal position with his legs elevated, and it is necessary to quickly replenish the volume of blood volume and the content of electrolytes.
Storage conditions
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C, in the original packaging (blister in a pack).
Keep out of the reach of children.
Shelf life
Shelf life
2 years.
Do not use the drug after the expiration date.
Manufacturer
Manufacturer
KRKA dd Novo Mesto, Slovenia
Additional information
| Shelf life | 2 years. Do not use the drug after the expiration date. |
|---|---|
| Conditions of storage | Storage conditions At the temperature not more than 25 °С, in the original package (blister in the package). Keep out of reach of children. |
| Manufacturer | KRKA dd Novo mesto, Slovenia |
| Medication form | pills |
| Brand | KRKA dd Novo mesto |
Related products
Buy Telmista N, tablets 12.5mg+40 mg 84 pcs with delivery to USA, UK, Europe and over 120 other countries.