No products in the cart.
Taflopress Rompharm, eye drops 0.015 mg/ml 2.5ml
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group: Antiglaucoma drug – prostaglandin F2-alpha analogue synthetic.
ATX code: S01EE05
Pharmacological properties
Pharmacodynamics
Tafluprost is a fluorinated analog of prostaglandin F2α. Tafluprost acid, the biologically active metabolite of tafluprost, is highly active and selective for the human FP-prostanoid receptor. The affinity of tafluprost acid to the FP receptor is 12 times higher than the affinity of latanoprost. Pharmacodynamic studies in monkeys have shown that tafluprost reduces intraocular pressure (IOP) by increasing uveoscleral aqueous outflow.
The experiments in monkeys with normal and elevated IOP showed that tafluprost is an effective medication for lowering IOP. In a study examining the IOP-lowering effects of tafluprost metabolites, tafluprost acid alone was found to significantly lower IOP.
The rabbit study showed that when tafluprost was administered as 0.0015% eye drops once daily for 4 weeks, blood flow in the optic disc was significantly (15%) increased compared to baseline when measured on days 14 and 28 using laser speckle-flowography.
Clinical efficacy
The decrease in IOP starts 2-4 h after the first instillation of tafluprost, and the maximum effect is achieved after about 12 h. The duration of the effect lasts for at least 24 h. In a 6-month study, tafluprost showed a significant IOP reduction effect of 6 to 8 mmHg at different time points compared to latanoprost, which reduced IOP by 7 to 9 mmHg. In another 6-month clinical trial, tafluprost reduced IOP by 5-7 mmHg compared to timolol, which reduced IOP by 4-6 mmHg. The IOP reduction effect of tafluprost was also maintained when these studies were extended to
12 months.
In a 6-week study, the IOP-lowering effect of tafluprost was compared with its indifferent filler when used with timolol. Compared with baseline values after a 4-week course of use with timolol, the additional effect of IOP reduction was 5-6 mmHg in the timolol-tafluprost group and 3-4 mmHg in the timolol-indifferent filler group. In a small cross-sectional study with a 4-week treatment period, the drug formulations of tafluprost with or without a preservative showed a similar IOP-lowering effect of more than 5 mm Hg.
In a 3-month study in the United States comparing the drug formulation of tafluprost without preservative with timolol (also without preservative), tafluprost was found to reduce IOP by 6.2-7.4 mmHg at different time points, whereas values for timolol varied between 5.3 and 7.5 mmHg.
Pharmacokinetics
Absorption
. After instillation of tafluprost, 0.0015% eye drops, once daily, one drop in both eyes for 8 days, plasma concentrations of tafluprost acid were low and had a similar profile on days 1 and 8. Maximum plasma concentrations (Cmax) were reached
10 minutes after instillation and declined below the lower limit of detection (10 pg/mL) in less than 1 hour after administration. Mean Cmax (24.4 and 31.4 pg/mL) and AUC0-last (405.9 and 581.1 pg*min/mL) values were almost identical at days 1 and 8, indicating that a sustained concentration of tafluprost was achieved during the first week of treatment. No statistically significant differences in systemic bioavailability were found between dosage forms with and without a preservative.
In a rabbit study, absorption of tafluprost into aqueous humor was comparable after a single injection of tafluprost, 0.0015% eye drops, with or without a preservative.
Distribution
. In a monkey study, there was no specific distribution of radioactively labeled tafluprost in the iris, ciliary body, or ocular vasculature, including the retinal pigment epithelium, indicating the low affinity of tafluprost for melanin pigment. In an autoradiographic study on rats, the highest concentration of radioactivity was observed in the cornea, followed by the eyelids, sclera, and iris. Systemically, radioactivity was distributed to the lacrimal system, palate, esophagus, gastrointestinal tract, kidneys, liver, gallbladder, and bladder.
The binding of tafluprost acid to human serum albumin
in vitro was 99% for 500 ng/mL tafluprost acid.
Metabolism
In the in vitro study found that the primary route of metabolism of tafluprost in humans is hydrolysis to form the pharmacologically active metabolite, tafluprost acid, which is further metabolized by glucuronidation or beta-oxidation. The beta-oxidation products, 1,2-dinor and 1,2,3,4-tetranor of tafluprost acid, which are pharmacologically inactive, can be glucuronidated or hydroxylated. The cytochrome P450 enzyme system (CYP) is not involved in metabolism of tafluprost acid. In a study performed on rabbit corneal tissue, it was found that the main esterase responsible for the ester hydrolysis of tafluprost to tafluprost acid is carboxylesterase. Butyrylcholinesterase, but not acetylcholinesterase, can also contribute to hydrolysis.
Elevation
In a study in rats after a single instillation of 3H-tafluprost (0.005% eye drops; 5 µl/eye) in both eyes for 21 days, about 87% of the total radioactive dose was detected in the feces. About 27-38% of the total dose was excreted by the kidneys and about
44-58% of the dose was excreted through the intestines.
Indications
Indications
Elevated intraocular pressure in patients with open-angle glaucoma and ophthalmohypertension:
As monotherapy in patients with insufficient response to first-line therapy or with intolerance to or contraindication of first-line therapy;
As adjunctive therapy to beta-blockers.
Active ingredient
Active ingredient
Composition
Composition
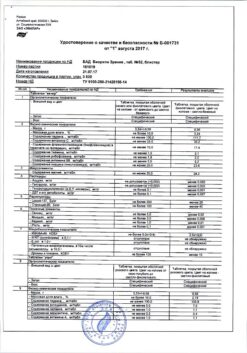
Composition per 1 ml of the drug:
Active substance:tafluprost – 0.0150 mg;
Auxiliary substances:dinatrate edetate – 0.50 mg, glycerol – 18.00 mg, boric acid – 5.00 mg, tiloxapol – 1.50 mg, polyquaternium-1 – 0.01 mg, 1 M hydrochloric acid solution or 1 M sodium hydroxide solution – to pH 6.0 ± 0.1, purified water – to 1.00 ml.
How to take, the dosage
How to take, the dosage
Doses
The recommended dose is one drop of Taflopress Romfarm into the conjunctival sac of the affected eye once daily, in the evening. The dose should be instilled strictly once a day because more frequent use may reduce the IOP-lowering effect.
To use
To prevent possible contamination of the solution, patients should not allow the tip of the bottle to come in contact with the eyelids, the skin around the eyes or any other surface.
Patients should remove excess solution from the skin to reduce the risk of darkening of the eyelid skin. As with other eye drops, a brief nasolacrimal occlusion or gentle eyelid closure after instillation is recommended. This may reduce systemic absorption of the drug.
When multiple ophthalmic drugs are used, intervals between applications should be at least 5 minutes.
Special patient groups
.Elderly patients
Dose adjustment in elderly patients is not necessary.
Children
The safety and effectiveness of tafluprost in children under 18 years of age have not been established.
Kidney/liver function impairment
There are no data on the use of tafluprost in patients with renal/hepatic impairment. Therefore, caution should be exercised when using the drug in these patient groups.
Interaction
Interaction
Due to the low plasma concentration of tafluprost after instillation of the drug, no cross interactions with other drugs are expected.
There have been no studies on the study of specific interactions of tafluprost with other drugs.
In co-administration of tafluprost with timolol no evidence of interaction has been observed in clinical studies.
Special Instructions
Special Instructions
Before treatment, patients should be informed of the possibility of eyelash growth, darkening of the eyelid skin, and increased iris pigmentation. Some of these changes may be permanent and may result in differences between the eyes if the drug is only injected in one eye.
The change in iris pigmentation is slow and may not be noticeable for several months. Eye discoloration occurs mostly in patients with mixed color irises, such as if the eyes are brownish-blue, grayish-brown, yellow-brown, or green-brown. Treatment of only one eye can lead to persistent heterochromia.
Tafluprost has no experience with neovascular, closed-angle, narrow-angle, or congenital glaucoma.
Tafluprost has limited experience with aphakia and pigmentary or pseudoexfoliative glaucoma.
Tafluprost should be used with caution in patients with aphakia, pseudophakia with posterior lens capsule rupture or with anterior chamber intraocular lenses, and in patients with established risk factors for cystoid macular edema or iritis/veitis.
Tafluprost has no experience in patients with severe bronchial asthma and in patients with impaired renal/liver function, so the drug should be used with caution in these patients.
There is a possibility of hair growth in areas where tafluprost solution is in constant contact with the skin surface.
Influence on the ability to drive vehicles and mechanisms
Tafluprost has no effect on the ability to drive vehicles and mechanisms. As with any other ophthalmologic agent after instillation of the drug a momentary blurring of vision may occur, therefore one should refrain from driving vehicles and performing activities requiring high concentration and quick psychomotor reactions until vision returns.
Synopsis
Synopsis
Contraindications
Contraindications
– Hypersensitivity to the active ingredient tafluprost or to any of the excipients of the drug.
– Age under 18 years (no data on clinical use).
Cautions
. Tafluprost should be used with caution in patients with aphakia, pseudophakia with posterior lens capsule rupture or with anterior chamber intraocular lenses, and in patients with established risk factors for cystoid macular edema or iritis/veitis.
Tafluprost should be used with caution in patients with aphakia and pigmentary or pseudoexfoliative glaucoma.
Tafluprost should be used with caution in patients with neovascular, closed-angle, narrow-angle, or congenital glaucoma.
Tafluprost should be used with caution in patients with severe bronchial asthma, in patients with impaired renal/liver function.
There is a possibility of hair growth in areas where tafluprost solution is in constant contact with the skin surface.
Side effects
Side effects
In clinical trials using tafluprost either as monotherapy or as adjunctive therapy to timolol 0.5%, the most commonly reported treatment-related adverse event was eye hyperemia. It was reported in approximately 13% of patients participating in clinical trials of tafluprost in Europe and the United States. In most cases, hyperemia was moderate and led to treatment discontinuation in an average of 0.4% of patients.
The adverse events with tafluprost are presented below according to organ involvement, organ system involvement, and frequency of occurrence.
The incidence of adverse reactions is defined as follows: very frequently (>1/10),often (>1/100 and <1/10), infrequently (>1/1000 and <1/100), rarely(⥠1/10000 and < 1/1000),very rarely(<1/10000),frequently unknown (frequency cannot be determined from available data).
Nervous system disorders
Frequently: headache.
From the visual organ
Often: Itchy eyes, eye irritation, eye pain, eye/conjunctival hyperemia, eyelash changes (increased length, thickness, and number of lashes), dry eyes, changes in lash color, sensation of foreign body in eyes, eyelid erythema, superficial pitting keratitis (PTC), blurred vision, increased tearfulness, decreased visual acuity, photophobia, and increased iris pigmentation.
Infrequent: Asthenopia, conjunctival edema, blepharitis, cellular opalescence of anterior chamber moisture, conjunctival follicles, allergic conjunctivitis, inflammatory reaction in anterior chamber moisture, conjunctival pigmentation, feeling of discomfort in the eye, eyelid pigmentation, eyelid edema, ocular discharge, atypical feeling in the eye.
Frequency unknown (cannot be estimated from available data): iritis/veitis, eyelid crease aggravation, retinal macular edema/cystic macular edema.
There have been reports of very rare cases of corneal tissue calcification due to the use of phosphate-containing eye drops in some patients with significant corneal damage.
Respiratory system, thorax and mediastinum
Frequency unknown: exacerbation of bronchial asthma, dyspnea.
Skin and subcutaneous tissue
Infrequent: hypertrichosis of eyelids.
Overdose
Overdose
Pregnancy use
Pregnancy use
Pregnancy
There are no data on the use of tafluprost in pregnant women. Tafluprost may have adverse pharmacological effects on the course of pregnancy and/or on the fetus/newborn child. Animal studies have shown reproductive toxicity. Therefore, tafluprost should not be used during pregnancy unless there are no other treatment options.
Women of preserved reproductive potential should not use tafluprost unless they are using adequate contraception.
Breastfeeding period
It is not known whether tafluprost or its metabolites penetrate into breast milk. Studies in rats have found penetration of tafluprost into breast milk after topical administration. Therefore, tafluprost should not be used during breastfeeding.
Fertility
Intravenous administration of tafluprost at doses up to 100 µg/kg/day had no effect on mating ability and fertility in female and male rats.
Similarities
Similarities
Additional information
| Weight | 0.015 kg |
|---|---|
| Shelf life | 3 years. After the first opening of the bottle – 4 weeks. Do not use after the expiration date! |
| Conditions of storage | At the temperature of 2-8 ° C, in the original package. Store at a temperature not exceeding 25 °С after opening the bottle. Store out of the reach of children! |
| Manufacturer | C.O.Rompharm Company S.R.L., Romania |
| Medication form | eye drops |
| Brand | C.O.Rompharm Company S.R.L. |
Related products
Buy Taflopress Rompharm, eye drops 0.015 mg/ml 2.5ml with delivery to USA, UK, Europe and over 120 other countries.