No products in the cart.
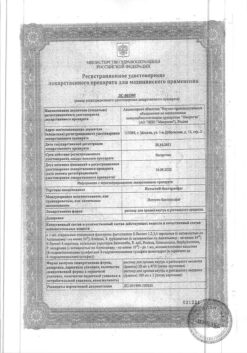
Selsept, 500 mg 50 pcs.
€1.00
Out of stock
(E-mail when Stock is available)
Description
In combination therapy with cyclosporine and corticosteroids:
- Prevention of acute organ rejection and treatment of therapy-refractory organ rejection in patients after allogeneic kidney transplantation;
- Prevention of acute organ rejection in patients after allogeneic liver transplantation.
.
Indications
Indications
As a combination therapy with cyclosporine and corticosteroids:
prevention of acute organ rejection and treatment of organ rejection refractory to therapy in patients after allogeneic kidney transplantation;
prevention of acute organ rejection and improvement of graft survival and patient survival after allogeneic heart transplantation;
prevention of acute organ rejection in patients after allogeneic liver transplantation.
Special instructions
Special instructions
As with the background of combined immunosuppression in general, and when MMF is prescribed as a component of an immunosuppressive regimen, there is an increased risk of developing lymphomas and other malignant neoplasms, especially of the skin (see “Side effects”). This risk does not appear to be related to the use of any drug per se, but to the intensity and duration of immunosuppression.
As with all patients at increased risk of skin cancer, exposure to sunlight and UV rays should be limited by wearing appropriate, covered clothing and using sunscreens with a high protection factor.
Patients receiving MMF should be instructed to promptly report any signs of infection, bleeding, hemorrhage, or other signs of bone marrow suppression to their physician.
Excessive suppression of the immune system may also increase susceptibility to infections, including opportunistic, sepsis and other fatal infections.
Cases of PML, sometimes fatal, have been observed in patients taking CellCept®. These case reports suggest that patients have additional risk factors for developing PML, including immunosuppressive therapy and immune deterioration. In immunosuppressed patients with neurological symptoms, a differential diagnosis of PML should be made and consultation with a neurologist should be recommended.
Cases of the development of PRCA have been observed in patients taking Cellcept in combination with other immunosuppressive drugs. The mechanism of development of PRCA when prescribing Cellcept, as well as other immunosuppressants and their combinations, is unknown. In some cases, PRCA was reversible after CellCept dose reduction or discontinuation. However, in transplant patients, decreased immunosuppression may compromise the graft.
Vaccination may be less effective during treatment with MMF; The use of live attenuated vaccines should be avoided. Influenza vaccination can be administered according to national guidelines.
Since taking MMF may be accompanied by adverse reactions from the gastrointestinal tract (ulceration of the mucous membrane, gastrointestinal bleeding, perforation), caution must be exercised when prescribing MMF to patients with diseases of the digestive tract in the acute stage.
Since MMF is an IMPDH inhibitor, theoretically, it should not be prescribed to patients with rare genetically determined hereditary deficiency of hypoxanthine guanine phosphoribosyltransferase (Lesch-Nyhan and Kelly-Siegmiller syndromes).
MMF is not recommended for coadministration with azathioprine because both drugs are bone marrow depressants and concomitant use has not been studied.
Caution should be exercised when concomitantly prescribing MMF with drugs that affect the enterohepatic circulation, as they may reduce the effectiveness of MMF (see “Interactions”).
In patients with severe chronic renal failure, dosages of more than 1 g 2 times a day should be avoided.
No dosage adjustment is required for patients with delayed renal graft function, but they should be closely monitored. There are no data available for patients who have undergone heart or liver transplantation and have severe renal failure.
Elderly patients may have a higher risk of adverse events than younger patients.
Laboratory control: when treating MMF, it is necessary to determine the complete blood count weekly during the first month, during the second and third months of treatment – 2 times a month, and then during the first year – monthly. Neutropenia may be associated with MMF, other medications, viral infections, or a combination of these reasons. If neutropenia occurs (absolute neutrophil count less than 1300 per 1 μl), it is necessary to interrupt MMF treatment or reduce the dose, while carefully monitoring these patients.
Handling the drug. Since MMF showed a teratogenic effect in experiments on rats and rabbits, CellCept tablets should not be broken and the integrity of the capsules should not be damaged. Avoid inhalation of the powder contained in CellCept capsules or direct contact with the skin or mucous membranes. If this happens, you need to thoroughly wash the area with soap and water, and your eyes with just water.
Active ingredient
Active ingredient
Mycophenolate mofetil
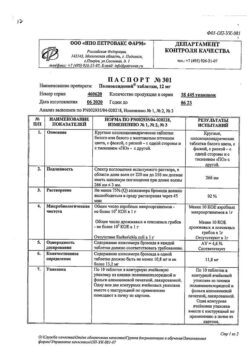
Composition
Composition
1 film-coated tablet contains:
active ingredient:
mycophenolate mofetil 500 mg,
excipients:
MCC;
croscarmellose sodium;
povidone (K-90);
magnesium stearate
shell:
Opadry Lavender Y-5-10272-A (hypromellose; hyprolose; titanium dioxide (E171); macrogol 400; indigo carmine dye (E132); iron oxide red dye (E172))
Contraindications
Contraindications
Hypersensitivity to mycophenolate mofetil or mycophenolic acid and other components of the drug.
With caution – gastrointestinal diseases (in the acute phase).
Side Effects
Side Effects
The side effect profile associated with the use of immunosuppressive drugs is often difficult to determine due to the presence of an underlying disease and the concomitant use of many other drugs.
Clinical trial data. The main adverse reactions associated with the use of MMF in combination with cyclosporine and corticosteroids for the prevention of renal, cardiac or liver transplant rejection are diarrhea, leukopenia, sepsis and vomiting; There is also evidence of an increased incidence of opportunistic infections.
The safety profile of MMF in the treatment of refractory kidney rejection is similar to that in the prevention of kidney rejection when using the drug at a dose of 3 g per day. Diarrhea and leukopenia, followed by anemia, nausea, vomiting, abdominal pain, and sepsis were the predominant adverse reactions occurring in patients receiving MMF more often than in patients receiving IV corticosteroids.
Malignant neoplasms. Lymphoproliferative diseases or lymphomas developed in 0.4–1% of patients who underwent kidney, heart or liver transplantation and were followed for at least 1 year receiving MMF (at doses of 2 or 3 g per day) in combination with other immunosuppressants. Skin carcinoma (excluding melanoma) was observed in 1.6–4.2% of patients, malignant neoplasms of other types – in 0.7–2.1% of patients. Three-year safety data in kidney or heart transplant patients did not reveal any unexpected changes in the incidence of malignancies compared with one-year rates. After liver transplantation, patients were followed up for at least 1 year, but less than 3 years.
In the treatment of refractory kidney rejection, the incidence of lymphoma during a mean follow-up period of up to 42 months was 3.9%.
Opportunistic infections. The risk of opportunistic infections is increased in all post-transplant patients and increases with the degree of immunosuppression. When MMF (2 or 3 g per day) was prescribed in combination with other immunosuppressants in patients observed for 1 year after kidney (at a dose of 2 g per day), heart and liver transplantation, the most common infections were candidiasis of the skin and mucous membranes, CMV viremia/CMV syndrome (13.5%) and infection caused by the herpes simplex virus.
The type of adverse reactions and the frequency of their occurrence with oral administration of 600 mg of MMF 2 times a day in children aged 3 months to 18 years were practically no different from those in adult patients receiving the drug at a dose of 1 g 2 times a day. However, adverse reactions such as diarrhea, leukopenia, sepsis, infections, and anemia were more common (≥10%) in children, especially under the age of 6 years.
In elderly and senile patients (≥65 years), when treated with MMF as part of combination immunosuppressive therapy, the risk of some infections (including tissue invasive forms of manifest WVD infection), and possibly gastrointestinal bleeding and pulmonary edema, is higher than in younger patients.
Adverse events reported in ≥10 and 3–10% of patients receiving MMF in combination with cyclosporine and corticosteroids after kidney, heart and liver transplantation
Organs and systems of the body
Frequency, %
Adverse events after kidney transplant
Adverse events after heart transplant
Adverse events after liver transplantation
Body as a whole
≥10
Asthenia, fever, headache, infections, pain (abdominal, lower back, chest), peripheral edema, sepsis
Asthenia, fever, chills, headache, infections, pain (abdominal, lower back, chest), peripheral edema, sepsis
Ascites, asthenia, fever, chills, bloating, headache, infections, pain (abdominal, lower back, chest), peripheral edema, sepsis, hernia, peritonitis
3–< 10
Cysts (including lymphocele and hydrocele), facial swelling, flu-like syndrome, bleeding, hernia, malaise, pelvic pain, bloating
Inflammation of the subcutaneous tissue, cysts (including lymphocele and hydrocele), facial swelling, flu-like syndrome, bleeding, hernia, bloating, malaise, pelvic pain, neck pain, pale skin
Abscess, inflammation of subcutaneous tissue, cysts (including lymphocele and hydrocele), flu-like syndrome, bleeding, malaise, neck pain
Blood system and lymphatic system
≥10
Anemia (including hypochromic), leukocytosis, leukopenia, thrombocytopenia
Anemia (including hypochromic), leukocytosis, leukopenia, thrombocytopenia, ecchymosis
Anemia (including hypochromic), leukocytosis, leukopenia, thrombocytopenia
3–< 10
Ecchymosis, polycythemia
Petechiae, increased prothrombin and thromboplastin times
Ecchymosis, increased prothrombin time, pancytopenia
Genitourinary tract
≥10
Hematuria, renal tubular necrosis, urinary tract infection
Renal dysfunction, oliguria, urinary tract infections
Renal dysfunction, oliguria, urinary tract infections
3–< 10
Albuminuria, dysuria, hydronephrosis, impotence, pyelonephritis, frequent urination
Dysuria, hematuria, impotence, nocturia, renal failure, urinary frequency, incontinence and urinary retention
Acute renal failure, dysuria, hematuria, renal failure, scrotal edema, frequent urination, urinary incontinence
Cardiovascular system
≥10
Increased blood pressure
Arrhythmia, bradycardia, heart failure, decreased or increased blood pressure, pericardial effusion
Decreased or increased blood pressure, tachycardia
3–< 10
Angina pectoris, atrial fibrillation, decreased blood pressure, orthostatic hypotension, tachycardia, thrombosis, vasodilation
Angina pectoris, arrhythmias (supraventricular and ventricular extrasystoles, atrial flutter and fibrillation, supraventricular and ventricular tachycardia), cardiac arrest, congestive heart failure, orthostatic hypotension, pulmonary hypertension, fainting, vasospasm, increased venous pressure
Arterial thrombosis, atrial fibrillation, arrhythmias, bradycardia, vasodilation, syncope
Metabolism
≥10
-
Acidosis (metabolic or respiratory), hypervolemia, weight gain
Impaired wound healing
3–< 10
Acidosis (metabolic or respiratory), dehydration, hypervolemia, weight gain
Impaired wound healing, alkalosis, dehydration, gout, hypovolemia, hypoxia, respiratory acidosis, thirst, weight loss
Acidosis (metabolic or respiratory), dehydration, hypervolemia, hypoxia, hypovolemia, weight gain, weight loss
Laboratory indicators
≥10
Hypercholesterolemia, hyperglycemia, hyperkalemia, hypokalemia, hypophosphatemia
Hyperbilirubinemia, increased residual nitrogen, increased creatinine, increased enzyme activity (LDH, AST, ALT) in the blood serum, hypercholesterolemia, hyperglycemia, hyperkalemia, hyperlipidemia, hyperuricemia, hypokalemia, hypomagnesemia, hyponatremia
Hyperbilirubinemia, increased residual nitrogen, increased creatinine, hyperglycemia, hyperkalemia, hypokalemia, hypocalcemia, hypoglycemia, hypomagnesemia, hypophosphatemia, hypoproteinemia
3–< 10
Increased ALP activity, increased enzyme activity (gamma-glutamyl transpeptidase, LDH, AST and ALT) in blood serum, increased serum creatinine, hypercalcemia, hyperlipidemia, hypocalcemia, hypoglycemia, hypoproteinemia, hyperuricemia
Increased ALP activity, hypocalcemia, hypochloremia, hypoglycemia, hypoproteinemia, hypophosphatemia
Increased alkaline phosphatase activity, increased enzyme activity (AST and ALT) in the blood serum, hypercholesterolemia, hyperlipidemia, hyperphosphatemia, hyponatremia
Gastrointestinal tract
≥10
Constipation, diarrhea, dyspepsia, nausea and vomiting, oral candidiasis
Constipation, diarrhea, dyspepsia, flatulence, nausea and vomiting, oral candidiasis
Anorexia, cholangitis, cholestatic jaundice, constipation, diarrhea, dyspepsia, flatulence, hepatitis, nausea and vomiting, oral candidiasis
3–< 10
Anorexia, flatulence, gastroenteritis, gastrointestinal bleeding, gastrointestinal candidiasis, gingivitis, gingival hyperplasia, hepatitis, intestinal obstruction, stomatitis, esophagitis
Anorexia, dysphagia, gastroenteritis, gingivitis, gingival hyperplasia, jaundice, melena, stomatitis, esophagitis
Dysphagia, gastritis, gastrointestinal bleeding, intestinal obstruction, jaundice, melena, ulceration of the oral mucosa, esophagitis, rectal damage, gastric ulcer, dry mouth
Respiratory organs
≥10
Increased cough, shortness of breath, pharyngitis, pneumonia, bronchitis
Asthma, increased cough, shortness of breath, pharyngitis, pleural effusion, pneumonia, rhinitis, sinusitis
Increased cough, shortness of breath, pharyngitis, pneumonia, pleural effusion, sinusitis, atelectasis
3–< 10
Asthma, pleural effusion, pulmonary edema, rhinitis, sinusitis
Apnea, atelectasis, bronchitis, nosebleeds, hemoptysis, hiccups, neoplasms, pneumothorax, pulmonary edema, increased sputum production, voice change
Asthma, bronchitis, nosebleeds, hyperventilation, pneumothorax, pulmonary edema, respiratory tract candidiasis, rhinitis
Skin and its appendages
≥10
Acne, herpes simplex
Acne, herpes simplex, shingles, rash
Rash, itching, excessive sweating
3–< 10
Hair loss, benign skin growths, fungal dermatitis, herpes zoster, hirsutism, itching, skin cancer, skin hypertrophy (including actinic keratosis), increased sweating, skin ulcers, rash
Benign skin neoplasms, fungal dermatitis, hemorrhages, itching, skin cancer, skin hypertrophy, excessive sweating, skin ulcers
Acne, fungal dermatitis, hemorrhages, herpes simplex, herpes zoster, hirsutism, benign skin neoplasms, skin ulcers, vesicular bullous rash
Nervous system
≥10
Dizziness, insomnia, tremor
Psychomotor agitation, anxiety, confusion, depression, dizziness, hypertonicity, insomnia, paresthesia, drowsiness, tremor
Anxiety, confusion, depression, dizziness, insomnia, paresthesia, tremor
3–< 10
Anxiety, depression, hypertonicity, paresthesia, drowsiness
Convulsions, emotional lability, hallucinations, neuropathy, memory loss, vertigo
Psychomotor agitation, convulsions, delirium, hypertonicity, hypoesthesia, neuropathy, psychosis, drowsiness, memory loss
Musculoskeletal system
≥10
-
Leg cramps, muscle pain, muscle weakness
-
3–< 10
Joint pain, leg cramps, muscle pain, muscle weakness
Joint pain
Joint pain, leg cramps, muscle pain, muscle weakness, osteoporosis
Sense organs
≥10
-
Amblyopia
-
3–< 10
Amblyopia, cataracts, conjunctivitis
Visual impairment, conjunctivitis, deafness, ear pain, eye hemorrhage, tinnitus
Visual impairment, amblyopia, conjunctivitis, deafness
Endocrine system
≥10
-
-
-
3–< 10
Diabetes mellitus, parathyroid disease (increased levels of parathyroid hormone)
Diabetes mellitus, Cushing's syndrome, hypothyroidism
Diabetes mellitus
In the prevention of renal transplant rejection, the safety profile of MMF at a daily dose of 2 g was slightly better than at a daily dose of 3 g.
Post-registration use of the drug
From the digestive system: colitis (sometimes of cytomegalovirus etiology), pancreatitis, isolated cases of intestinal villi atrophy.
From the immune system: isolated cases of severe, life-threatening infections (meningitis, infective endocarditis), increased frequency of certain infections such as tuberculosis and atypical mycobacterial infections.
Cases of progressive multifocal leukoencephalopathy (PML), sometimes fatal, have been observed in patients taking CellCept®. These case reports suggest that patients have additional risk factors for developing PML, including immunosuppressive therapy and immune deterioration.
Cases of partial red cell aplasia (PRCA) have been observed in patients taking Cellcept in combination with other immunosuppressive drugs.
Developmental abnormalities: Cases of fetal abnormalities (including ear malformations) have been reported in patients taking MMF during pregnancy in combination with other immunosuppressants.
Other adverse reactions observed during post-registration use of the drug do not differ from the adverse reactions recorded in clinical studies.
Interaction
Interaction
Acyclovir. Concomitant use of mycophenolate mofetil and acyclovir increases plasma concentrations of both drugs in renal failure, possibly as a result of competition for tubular secretion, which may lead to further increases in the concentrations of both drugs.
Antacids containing magnesium and aluminum hydroxide reduce the absorption of MMF.
Cholestyramine. After administering a single dose of mycophenolate mofetil 1.5 g to healthy volunteers who had previously taken 4 g of cholestyramine 3 times a day for 4 days, a decrease in AUCMPC by 40% was observed. Caution must be exercised when coadministering MMF and drugs that affect enterohepatic recirculation.
Cyclosporine A. Mycophenolate mofetil does not affect the pharmacokinetics of cyclosporine A. When administered concomitantly, exposure to mycophenolic acid is reduced by 30-50% compared to patients receiving MMF in combination with sirolimus.
Ganciclovir. Based on the results of a study with single oral administration of the recommended doses of mycophenolate mofetil and intravenous administration of ganciclovir, no significant change in the pharmacokinetics of MMF is expected, therefore no dose adjustment of MMF is necessary. If MMF and ganciclovir are prescribed to patients with renal insufficiency, patients should be monitored carefully.
Oral contraceptives. MMF does not affect the pharmacokinetics of oral contraceptives. When taken simultaneously with combined oral contraceptives containing ethinyl estradiol (0.02–0.04 mg) and levonorgestrel (0.05–0.2 mg), desogestrel (0.15 mg) or gestodene (0.05–0.1 mg), Cellcept (1 g 2 times a day) does not have a clinically significant effect on the levels of progesterone, LH and FSH. Thus, Cellcept has no effect on the suppression of ovulation under the influence of oral contraceptives.
However, while taking Cellcept, other methods of contraception must be used in addition to oral contraceptives.
Trimethoprim/sulfamethoxazole, norfloxacin, metronidazole. They do not affect the bioavailability of MPA when prescribed with one of the antibacterial drugs. But simultaneous administration of the drug Cellcept in combination with norfloxacin and metronidazole reduces the AUC0-48 MFC by 30% after a single dose of the drug Cellcept.
Tacrolimus. When administered simultaneously, there was no effect on the AUC and Cmax of MPA in patients after liver and kidney transplantation. In patients after kidney transplantation, the administration of Cellcept did not affect the concentration of tacrolimus. In patients with a stable liver transplant, the AUC of tacrolimus after repeated doses of MMF at a dose of 1.5 g twice daily increased by approximately 20%.
Rifampicin. After dose adjustment, a 70% reduction in mycophenolic acid exposure (AUC0-12) was observed in patients after simultaneous heart and lung transplantation; monitoring of MPA exposure and dose adjustment of CellCept is recommended to maintain the clinical effect when administered together.
Ciprofloxacin and amoxicillin in combination with clavulanic acid. In patients after kidney transplantation, in the days immediately after oral administration of ciprofloxacin or amoxicillin in combination with clavulanic acid, a decrease in IPA Cmin by 54% was observed. With continued antibiotic therapy, this effect decreases and disappears after cessation of therapy. The clinical significance of this phenomenon is unknown since changes in Cmin may not adequately reflect changes in total MPA exposure.
Other interactions. Blockers of tubular secretion (probenecid) increase the concentration of MPAG.
Concomitant use of sevelamer and MPA in adults and children reduces the Cmax and AUC0–12 of MPA by 30 and 25%, respectively. Sevelamer and other non-calcium containing phosphate binders should be administered 2 hours after taking CellCept to reduce the effect on MPA absorption.
Live vaccines. Should not be administered to immunosuppressed patients. Antibody production in response to other vaccines may be reduced.
Overdose
Overdose
Data on overdose of MMF have been obtained from clinical studies and post-marketing use. In most cases, no data on adverse events were recorded. The adverse events that developed during the overdose coincided with the known safety profile of the drug.
Expected symptoms: MMF overdose is expected to likely lead to immunosuppression (consequently increased susceptibility to infection) and bone marrow suppression.
Treatment: if neutropenia develops, CellCept should be discontinued or the dose reduced.
MPA cannot be removed from the body by hemodialysis. However, at high plasma concentrations of MPAG (>100 μg/ml), small amounts are still excreted.
Bile acid binders, such as cholestyramine, may help eliminate MPA from the body by increasing its excretion.
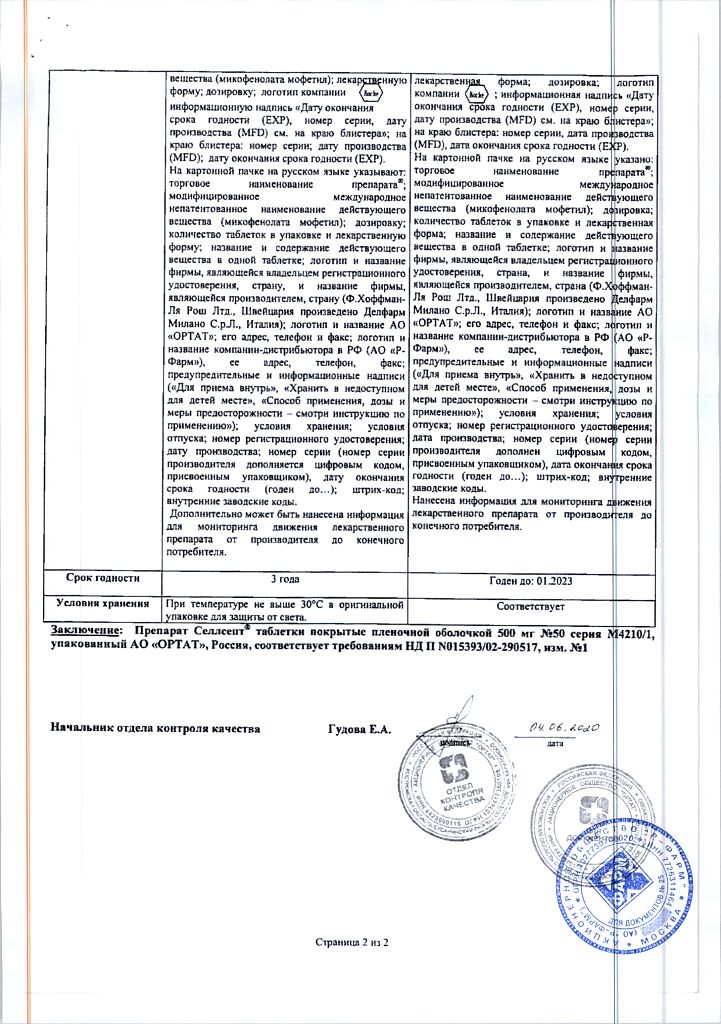
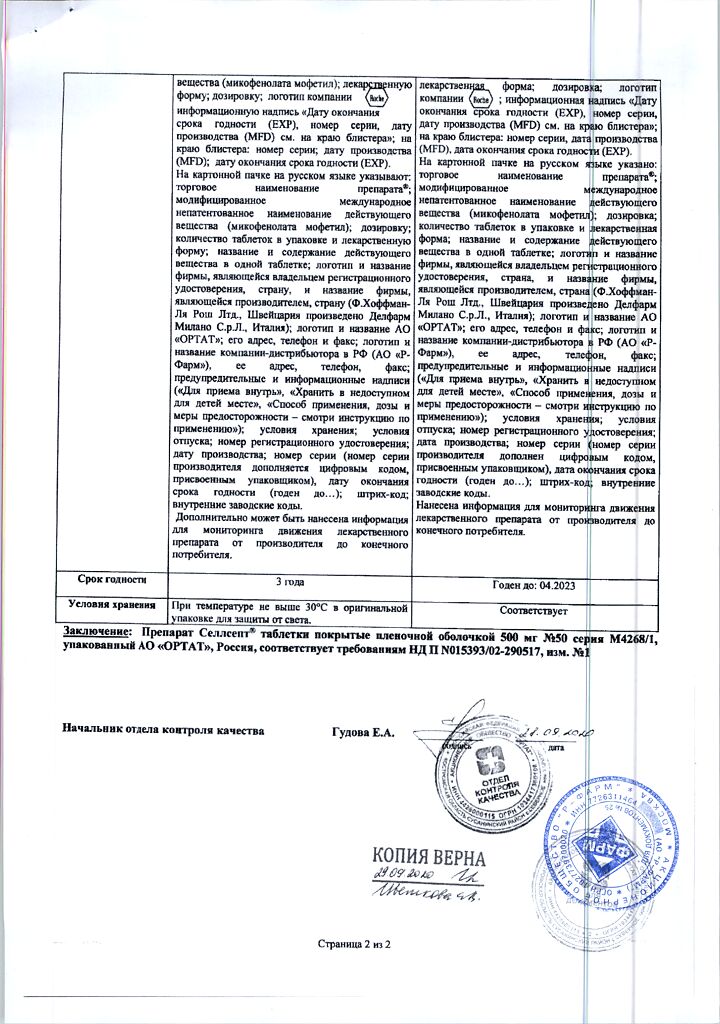
Storage conditions
Storage conditions
In a dry place, protected from light, at a temperature not exceeding 30 °C
Shelf life
Shelf life
3 years
Manufacturer
Manufacturer
Delfarm Milano S.r.L./Hoffmann la Roche, Italy
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | In a dry, light-protected place at a temperature not exceeding 30 °C |
| Manufacturer | Delpharm Milano S.r.l./Hoffmann la Roche, Italy |
| Medication form | pills |
| Brand | Delpharm Milano S.r.l./Hoffmann la Roche |
Related products
Buy Selsept, 500 mg 50 pcs. with delivery to USA, UK, Europe and over 120 other countries.