No products in the cart.
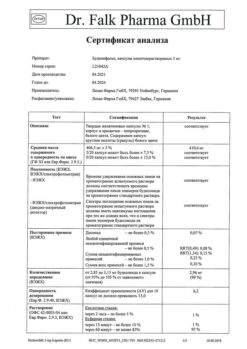
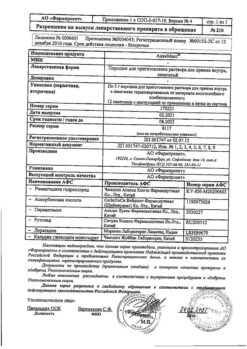
Salticasone, 50 mcg+100 mcg 60 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Clinical and pharmacological group: Anti-inflammatory and bronchodilator
Pharmacological action
Combination drug that contains salmeterol and fluticasone propionate with different mechanisms of action. Salmeterol prevents symptoms of bronchospasm; fluticasone propionate improves pulmonary function and prevents exacerbation of the disease.
Salmeterol is a selective long-acting (up to 12 h) β2 adrenoreceptor agonist that has a long side chain that binds to the outer domain of the receptor. The pharmacological properties of salmeterol provide more effective protection against histamine-induced bronchoconstriction and longer bronchodilation (lasting at least 12 h) than short-acting β2-adrenoreceptor agonists.
In vitro studies have shown that salmeterol is a potent inhibitor of the release from the human lung of mast cell mediators such as histamine, leukotrienes and prostaglandin D2 and has a long duration of action.
Salmeterol inhibits the early and late phases of response to inhaled allergens. Inhibition of the late phase response persists for more than 30 h after a single dose, at which time the bronchodilator effect is no longer present. A single dose of salmeterol attenuates bronchial hyperresponsiveness. This indicates that salmeterol, in addition to its bronchodilator activity, has an additional action unrelated to bronchial dilation, the clinical significance of which has not been definitively established. This mechanism of action is different from the anti-inflammatory effect of GCS.
Fluticasone – GCS for topical use and when administered by inhalation in recommended doses has a pronounced anti-inflammatory and anti-allergic effect in the lungs, which leads to a reduction of clinical symptoms, reducing the frequency of exacerbations of bronchial asthma.
Pharmacokinetics
Salmeterol
Acts locally in the lung tissues, so its plasma content does not correlate with therapeutic effects. Data on its pharmacokinetics are very limited because when inhaled at therapeutic doses, its Cmax in plasma is extremely low (about 200 pg/mL and below). After regular inhalation with salmeterol, hydroxynaphthic acid, Css of which is about 100 ng/mL, can be detected in the blood. These concentrations are 1000 times lower than the Css observed in toxicity studies. Results of in vitro studies have shown that salmeterol is extensively metabolized by the CYP3A4 isoenzyme of the cytochrome P450 system to α-hydroxysalmeterol by aliphatic oxidation.
The absolute bioavailability of inhaled fluticasone propionate in healthy subjects varies depending on the inhaler used; it is 5.3% when the combination of salmeterol and fluticasone propionate is administered with a metered dose inhalation aerosol. Patients with bronchial asthma and COPD have lower plasma concentrations of fluticasone propionate. Systemic absorption occurs primarily through the lungs. At first it is more rapid, but then its rate slows down. Part of the inhaled dose can be swallowed, but this part makes a minimal contribution to systemic absorption due to the low solubility of fluticasone propionate in water and due to its presystemic metabolism; bioavailability from the GI tract is less than 1%. As the inhaled dose increases, there is a linear increase in plasma concentrations of fluticasone propionate. Fluticasone has a large Vd in equilibrium (about 300 l) and has a relatively high degree of binding to plasma proteins (91%). It is rapidly eliminated from the blood, mainly as a result of metabolism by the CYP3A4 isoenzyme of the cytochrome P450 system to an inactive carboxyl metabolite. Fluticasone distribution is characterized by rapid plasma clearance (1150 ml/min) and a final T1/2 of approximately 8 h. Renal clearance of unchanged fluticasone propionate is negligible (< 0.2%), with less than 5% of the dose excreted in the urine as a metabolite.
Indications
Indications
For the regular treatment of bronchial asthma, if combination therapy with a long-acting beta2-adrenergic agonist and inhaled corticosteroids is indicated.
For maintenance therapy in patients with COPD with an FEV1 value <60% of normal before bronchodilator inhalation and a history of repeated exacerbations, in whom severe symptoms of the disease persist despite regular bronchodilator therapy.
Pharmacological effect
Pharmacological effect
Clinical and pharmacological group: Drug with anti-inflammatory and bronchodilator action
Pharmacological action
A combination drug that contains salmeterol and fluticasone propionate, which have different mechanisms of action. Salmeterol prevents the occurrence of symptoms of bronchospasm, fluticasone propionate improves pulmonary function and prevents exacerbation of the disease.
Salmeterol is a selective, long-acting (up to 12 hours) β2-adrenergic receptor agonist with a long side chain that binds to the outer domain of the receptor. The pharmacological properties of salmeterol provide more effective protection against histamine-induced bronchoconstriction and longer-lasting bronchodilation (lasting at least 12 hours) than short-acting β2-adrenergic receptor agonists.
In vitro studies have shown that salmeterol is a potent inhibitor of the release of mast cell mediators such as histamine, leukotrienes and prostaglandin D2 from the human lung, and has a long period of action.
Salmeterol inhibits the early and late phases of the response to inhaled allergens. Inhibition of the late phase response persists for more than 30 hours after taking a single dose, at a time when the bronchodilator effect is no longer present. A single administration of salmeterol weakens the hyperreactivity of the bronchial tree. This indicates that salmeterol, in addition to bronchodilator activity, has an additional effect not associated with bronchial dilation, the clinical significance of which has not been fully established. This mechanism of action differs from the anti-inflammatory effect of GCS.
Fluticasone – GCS for topical use and inhalation administration in recommended doses has a pronounced anti-inflammatory and antiallergic effect in the lungs, which leads to a decrease in clinical symptoms and a decrease in the frequency of exacerbations of bronchial asthma.
Pharmacokinetics
Salmeterol
It acts locally in the lung tissues, so its content in the blood plasma does not correlate with therapeutic effects. Data on its pharmacokinetics are very limited, because when inhaled in therapeutic doses, its Cmax in plasma is extremely low (about 200 pg/ml and below). After regular inhalations of salmeterol, hydroxynaphthoic acid can be detected in the blood, the Css of which is about 100 ng/ml. These concentrations are 1000 times lower than the Css observed in toxicity studies. The results of an in vitro study showed that salmeterol is extensively metabolized by the CYP3A4 isoenzyme of the cytochrome P450 system to α-hydroxysalmeterol by aliphatic oxidation.
Fluticasone
The absolute bioavailability of inhaled fluticasone propionate in healthy subjects varies depending on the inhaler used; when administering a combination of salmeterol and fluticasone propionate using a metered dose inhalation aerosol, it is 5.3%. In patients with bronchial asthma and COPD, lower plasma concentrations of fluticasone propionate are observed. Systemic absorption occurs primarily through the lungs. At first she is faster, but then her speed slows down. Part of the inhalation dose may be swallowed, but this part makes a minimal contribution to systemic absorption due to the low solubility of fluticasone propionate in water and due to its first-pass metabolism; bioavailability from the gastrointestinal tract is less than 1%. As the inhalation dose increases, a linear increase in the concentration of fluticasone propionate in the blood plasma is observed. Fluticasone has a large Vd at steady state (about 300 L) and has a relatively high degree of binding to plasma proteins (91%). It is quickly eliminated from the blood, mainly as a result of metabolism under the influence of the CYP3A4 isoenzyme of the cytochrome P450 system to an inactive carboxyl metabolite. The distribution of fluticasone is characterized by rapid plasma clearance (1150 ml/min) and a final T1/2 of approximately 8 hours. The renal clearance of unchanged fluticasone propionate is negligible (<0.2%), less than 5% of the dose is excreted in the form of a metabolite in the urine.
Special instructions
Special instructions
This combination is not intended for the relief of acute symptoms, since in such cases a fast-acting, short-acting inhaled bronchodilator (eg, salbutamol) should be used.
More frequent use of short-acting bronchodilators to relieve symptoms indicates worsening disease control, and in such situations the patient should consult a doctor.
Sudden and increasing deterioration in control of bronchospastic syndrome poses a potential threat to life, and in such situations the patient should also consult a doctor.
Patients with asthma should not abruptly stop treatment with this combination; the dose of the drug should be reduced gradually under the supervision of a physician. In patients with COPD, drug withdrawal may be accompanied by symptoms of decompensation and requires medical supervision.
Any inhaled GCS can cause systemic effects, especially with long-term use in high doses; however, the likelihood of such symptoms occurring is much lower than with treatment with oral corticosteroids. Possible systemic reactions include Cushing’s syndrome, Cushingoid features, adrenal suppression, growth retardation in children and adolescents, decreased bone mineral density, cataracts, and glaucoma. Therefore, when treating asthma, it is important to reduce the dose to the lowest dose that provides effective control of the disease.
In emergency and planned situations with the likelihood of stress, the possibility of suppressing the function of the adrenal cortex and the need to use GCS should always be taken into account.
When carrying out resuscitation measures or surgical interventions, it is necessary to determine the degree of adrenal insufficiency.
It is recommended to regularly measure the height of children who receive long-term therapy with inhaled corticosteroids.
Due to the possibility of adrenal suppression, patients switched from oral corticosteroids to inhaled fluticasone propionate therapy should be treated with extreme caution and their adrenal function regularly monitored.
After starting treatment with inhaled fluticasone, systemic corticosteroids should be withdrawn gradually, and such patients should have a special patient card containing an indication of the possible need for additional administration of corticosteroids in stressful situations.
In patients with exacerbation of bronchial asthma, hypoxia, it is necessary to monitor the concentration of potassium in plasma.
There are very rare reports of increased blood glucose levels; this should be taken into account when using this combination in patients with diabetes mellitus.
Active ingredient
Active ingredient
Salmeterol, Fluticasone
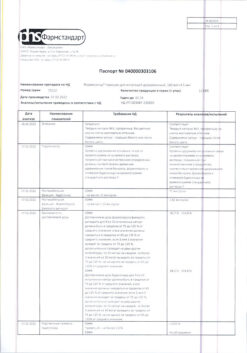
Composition
Composition
Composition per dose:
Active ingredients:
Salmeterol xinafoate 72.5 mcg (in terms of salmeterol) 50 mcg
Fluticasone propionate 250 mcg
Excipients:
Sodium benzoate 2.0 mg
Lactose monohydrate up to 12.0 mg
Gelatin capsules* capsule body: titanium dioxide 2%, gelatin up to 100%
capsule cap: titanium dioxide 1%, gelatin up to 100%
* applicable for the drug intended for use using the single-dose inhaler “Inhaler CDM®”
Pregnancy
Pregnancy
Use during pregnancy and breastfeeding is permissible only if the potential benefit to the mother outweighs the possible risk to the fetus or infant.
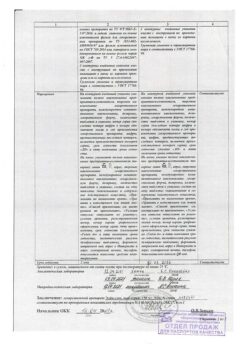
Contraindications
Contraindications
Hypersensitivity to the components of the drug; children under 4 years of age.
With caution: patients with acute or latent pulmonary tuberculosis; thyrotoxicosis; fungal, viral or bacterial infections of the respiratory system; cardiovascular diseases, supraventricular tachycardia and extrasystole, ventricular extrasystole, atrial fibrillation; hypokalemia; glaucoma, cataracts, osteoporosis; diabetes mellitus
Side Effects
Side Effects
Infectious and parasitic diseases: often – candidiasis of the oral cavity and pharynx, pneumonia (in patients with COPD); rarely – esophageal candidiasis.
From the immune system: hypersensitivity reactions: infrequently – skin hypersensitivity reactions, shortness of breath; rarely – anaphylactic reactions.
From the endocrine system: infrequently – cataracts; rarely – glaucoma, Cushing’s syndrome, Cushingoid symptoms, suppression of adrenal function, growth retardation in children and adolescents, decreased bone mineral density.
From the side of metabolism and nutrition: infrequently – hyperglycemia; very rarely – hypokalemia.
Mental disorders: infrequently – anxiety, sleep disorders; rarely – changes in behavior, incl. hyperactivity and irritability (especially in children).
From the nervous system: very often – headache; infrequently – tremor.
From the heart: infrequently – rapid heartbeat, tachycardia, atrial fibrillation; rarely – arrhythmia, including ventricular extrasystole, supraventricular tachycardia and extrasystole.
From the respiratory system: often – hoarseness and/or dysphonia; uncommon – pharyngeal irritation; rarely – paradoxical bronchospasm.
From the skin and subcutaneous tissues: infrequently – bruising.
From the musculoskeletal system: often – muscle spasms, arthralgia.
Interaction
Interaction
Due to the risk of developing bronchospasm, the use of selective and non-selective beta-blockers should be avoided, unless they are absolutely necessary for the patient.
A drug interaction study showed that ritonavir, a highly active inhibitor of the CYP3A4 isoenzyme, can cause a sharp increase in plasma fluticasone propionate concentrations, resulting in a significant decrease in serum cortisol concentrations. There have been reports of clinically significant drug interactions between fluticasone and ritonavir, which resulted in systemic effects of GCS, including Cushing’s syndrome and adrenal suppression. Therefore, it is recommended to avoid the combined use of fluticasone propionate and ritonavir, unless the potential benefit to the patient outweighs the risk associated with the systemic effects of GCS.
Studies have shown that other inhibitors of the CYP3A4 isoenzyme cause a negligible (erythromycin) and insignificant (ketoconazole) increase in plasma fluticasone levels, with virtually no decrease in serum cortisol concentrations. Despite this, caution is recommended during concomitant use of fluticasone propionate and strong CYP3A4 inhibitors (e.g. ketoconazole), as such combinations may increase plasma concentrations of fluticasone, which could potentially increase its systemic effects.
When studying drug interactions, it was found that the use of ketoconazole as concomitant systemic therapy significantly increases the concentration of salmeterol in the blood plasma (increase in Cmax by 1.4 times and AUC by 15 times). This may lead to prolongation of the QTc interval. Caution should be exercised when co-administering strong CYP3A4 inhibitors (eg, ketoconazole) and salmeterol.
Xanthine derivatives, corticosteroids and diuretics increase the risk of developing hypokalemia (especially in patients with exacerbation of bronchial asthma, during hypoxia).
MAO inhibitors and tricyclic antidepressants increase the risk of side effects from the cardiovascular system.
Manufacturer
Manufacturer
Pharmstandard-Leksredstva, Russia
Additional information
| Manufacturer | Pharmstandard-Leksredstva, Russia |
|---|---|
| Medication form | metered inhalation powder |
| Brand | Pharmstandard-Leksredstva |
Related products
Buy Salticasone, 50 mcg+100 mcg 60 pcs with delivery to USA, UK, Europe and over 120 other countries.