No products in the cart.
Rosuvastatin, 10 mg 90 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group:hypolipidemic drug – HMG-CoA reductase inhibitor
ATX code: C10AA07
Pharmacological properties
Pharmacodynamics
Rosuvastatin is a selective competitive inhibitor of HMG-CoA reductase, the enzyme that converts 3-hydroxy-3-methylglutaryl coenzyme A to mevalonic acid, a precursor of cholesterol (CH). The main target of rosuvastatin action is the liver, where the synthesis of cholesterol and catabolism of low-density lipoprotein cholesterol (LDL-C) take place.
Rosuvastatin increases the number of LDL-C receptors on the surface of liver cells, increasing the capture and catabolism of LDL-C, which in turn leads to inhibition of synthesis of very low-density lipoprotein cholesterol
(LDL-C), thereby reducing the total amount of LDL-C and LDL-C.
. Rosuvastatin reduces elevated concentrations of LDL-C, total cholesterol, triglycerides (TG), increases the concentration of high-density lipoprotein cholesterol (HDL-C) Reduces apolipoprotein B (ApoB), high-density lipoprotein cholesterol (HDL-C), HDL-C, TG and increases apolipoprotein A I (ApoA-I) concentration, decreases the ratiobr> HDL/CHDL, total cholesterol/CHDL and non-HDL/CHDL and ApoB/ApoA-I ratios.
Therapeutic effect appears within one week after the start of therapy with rosuvastatin, after 2 weeks of treatment it reaches 90% of the maximum possible effect. Maximum therapeutic effect is usually reached by the 4th week of therapy and is maintained with regular use of the drug.
Rosuvastatin is effective in adult patients with hypercholesterolemia, with or without hypertriglyceridemia, including patients with diabetes mellitus and familial hypercholesterolemia.
Additive effect is noted when combined with fenofibrate (for lower TG concentrations) and nicotinic acid at lipid-lowering doses ≥1 g/day (for HDL-C concentrations), but this combination must be evaluated by the treating physician with regard to possible risks.
Pharmacokinetics
Extraction. Maximum concentration (Cmax) of rosuvastatin in blood plasma is reached approximately 5 hours after oral administration. Absolute bioavailability is approximately 20%.
Distribution. Rosuvastatin accumulates mainly in the liver, the main organ of HC synthesis and LDL-C clearance. The volume of distribution (Vd) is approximately 134 liters. Binding to plasma proteins (predominantly to albumin) is approximately 90%.
Metabolism. Biotransformed to a small extent (about 10%), being a non-core substrate for metabolism by enzymes of cytochrome P450 system. The main isoenzyme involved in metabolism of rosuvastatin is CYP2C9. CYP2C19, CYP3A4 and CYP2D6 isoenzymes are less involved in metabolism. The main identified metabolites of rosuvastatin are N-dismethyl and lactone metabolites. N-dismethyl metabolite is about 50% less active than rosuvastatin, lactone metabolites are pharmacologically inactive. More than 90% of the pharmacological activity on inhibition of circulating HMG-CoA reductase is provided by rosuvastatin, the rest by its metabolites.
Evolution. 1/2) is approximately 19 hours. T1/2 does not change with increasing drug dose. Mean plasma clearance is approximately 50 L/hour (coefficient of variation 21.7%).
As in the case of other HMG-CoA reductase inhibitors, the membrane anion transporter of cholesterol is involved in the “hepatic” uptake of rosuvastatin and plays an important role in hepatic elimination of rosuvastatin.
Pharmacokinetics in special patient groups
Age and gender <
Percentage and age have no clinically significant effect on the pharmacokinetics of rosuvastatin.
Ethnic groups
Pharmacokinetic studies have shown an approximately twofold increase in median AUC (area under the concentration-time curve) and Cmax rosuvastatin in Asian patients (Japanese, Chinese, Filipinos, Vietnamese and Koreans) compared with Europeans; a 1.3-fold increase in median AUC and Cmax was shown in Indian patients. Pharmacokinetic analysis showed no clinically significant differences in pharmacokinetics between Europeans and members of the Negro race.
Renal failure
In patients with mild to moderate renal failure, the plasma concentration of rosuvastatin or N-dismethyl metabolite is not significantly changed.
In patients with severe renal failure (creatinine clearance (CK) < 30 ml/min) the plasma concentration of rosuvastatin is 3 times higher and the concentration of N-dismethyl metabolite is 9 times higher than in healthy volunteers. Plasma concentrations of rosuvastatin were approximately 50% higher in patients on hemodialysis than in healthy volunteers.
Hepatic failure
In patients with various stages of hepatic failure no increase in T1/2 rosuvastatin (patients with a Child-Pugh score of 7 or lower) was found. Individual patients with Child-Pugh scores of 8 and 9 showed at least a 2-fold increase in T1/2. There is no experience with rosuvastatin in patients with a Child-Pugh score above 9.
Genetic polymorphism
. HMG-CoA reductase inhibitors, including rosuvastatin, bind to the transport proteins OATP1B1 (an organic anion transporter involved in statin uptake by hepatocytes) and BCRP (efflux transporter). Carriers of SLCO1B1 (OATP1B1) c.521CC and ABCG2 (BCRP) c.421AA genotypes showed 1.6- and 2.4-fold increases in AUC to rosuvastatin, respectively, compared with SLCO1B1 c.521TT and ABCG2 c.421CC genotypes carriers.
Indications
Indications
Active ingredient
Active ingredient
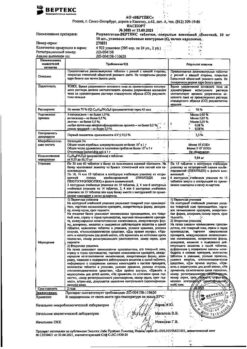
Composition
Composition
Tablets 5 mg. 1 tablet contains: acting substance rosuvastatin calcium (in terms of rosuvastatin) 5.21 (5.00) mg; excipients: microcrystalline cellulose 47.82 mg, crosspovidone 30.00 mg, lactose 54.97 mg, povidone-K30 8.50 mg, sodium stearyl fumarate 3.50 mg; coating film
How to take, the dosage
How to take, the dosage
In the body, the drug can be taken at any time of the day, regardless of meals. The tablet should be swallowed whole with water, without chewing or crushing.
Before starting therapy with the drug Rosuvastatin-Teva, the patient should start following a standard hypolipidemic diet and continue to follow it during treatment. The dose of the drug should be adjusted individually depending on the indication and therapeutic response, taking into account current recommendations for target lipid concentrations. The recommended starting dose of Rosuvastatin-Teva for patients starting to take the drug or for patients transferred from other HMG-CoA reductase inhibitors is 5 or 10 mg once daily. The initial dose should be guided by the patient’s plasma cholesterol concentration and the risk of cardiovascular complications should be taken into account, and the potential risk of adverse reactions (AR) should be assessed. If necessary, the dose may be increased after 4 weeks.
Patients with severe hypercholesterolemia and a high risk of cardiovascular complications (especially patients with familial hypercholesterolemia) who have not achieved the desired outcome with the 20 mg dose during
4-week therapy should be monitored by a physician when increasing the drug dose to 40 mg due to a possible increased risk of HP.
Particular close monitoring of patients receiving the drug at the 40 mg dose is recommended.
The 40 mg dose is not recommended for patients who have not previously seen a physician. After 2-4 weeks of therapy and/or increasing the dose of Rosuvastatin-Teva it is necessary to monitor lipid metabolism parameters.
In Elderly patients (over 65 years), no dose adjustment is required.
Patients with renal insufficiency. In patients with mild to moderate renal insufficiency, no dose adjustment is required. Rosuvastatin-Teva is contraindicated in any dose in patients with severe renal failure (CKD < 30 ml/min). The use of the drug Rosuvastatin-Teva in a dose of 40 mg is contraindicated in patients with moderate renal failure (CKR < 60 ml/min). In patients with moderate renal impairment, a starting dose of 5 mg is recommended.
Patients with hepatic impairment. Rosuvastatin is contraindicated in patients with active liver disease.
Special populations. Ethnic groups. When studying pharmacokinetic parameters of rosuvastatin in patients belonging to different ethnic groups, an increase in systemic concentration of rosuvastatin among Japanese and Chinese was noted (see section “Cautionary Note”). This fact should be considered when using Rosuvastatin-Teva in these patient groups. For Asian patients, the recommended starting dose is 5 mg. The use of Rosuvastatin-Teva in a dose of 40 mg is contraindicated in patients of Asian race.
Genetic polymorphisms
Carriers of the SLCO1B1 (OATP1B1) c.521CC and ABCG2 (BCRP) c.421AA had increased exposure (AUC) to rosuvastatin compared with SLCO1B1 c.521TT and ABCG2 c.421CC genotype carriers. For c.521CC or c.421AA genotype carriers, the recommended maximum daily dose of Rosuvastatin-Teva is 20 mg once daily (see sections “Pharmacokinetics” and “Precautions” and “Interaction with other medicinal products”).
Predisposition to myopathy
The use of Rosuvastatin-Teva in dose 40 mg is contraindicated in patients with factors that may indicate a predisposition to myopathy (See section “Special Precautions”). When using doses of 10 and 20 mg, a starting dose of 5 mg is recommended for patients in this group.
Companion therapy
Rosuvastatin binds to various transport proteins (in particular to OATP1B1 and BCRP). When concomitant use of Rosuvastatin-Teva with cyclosporine and HIV protease inhibitors (including the combination of ritonavir with atazanavir, lopinavir) the risk of myopathy (including rhabdomyolysis) increases, so alternative therapy or temporary withdrawal of Rosuvastatin-Teva should be considered. If concomitant use of these drugs is unavoidable, the benefit/risk ratio of concomitant therapy with Rosuvastatin-Teva should be assessed and the possibility of reducing its dose should be considered.
Interaction
Interaction
Influence of other drugs on rosuvastatin
Transport protein inhibitors: Rosuvastatin binds to several transport proteins, in particular OATP1B1 and BCRP. Concomitant use of drugs that are inhibitors of these transport proteins may be accompanied by increased plasma concentrations of rosuvastatin and an increased risk of myopathy (see Table 1 and sections “Administration and Dose” and “Precautions”).
Cyclosporine:when used concomitantly with rosuvastatin and cyclosporine, the AUC of rosuvastatin was on average 7 times higher than that observed in healthy volunteers (see Table 1). No effect on the plasma concentration of cyclosporine. Rosuvastatin is contraindicated in patients taking cyclosporine (see section “Contraindications”).
Human immunodeficiency virus (HIV) protease inhibitors:While the exact mechanism of interaction is unknown, co-administration of HIV protease inhibitors may result in a significant increase in exposure to rosuvastatin (see Table 1). A pharmacokinetic study of concomitant administration of 20 mg rosuvastatin with a combination drug containing two HIV protease inhibitors (400 mg lopinavir/100 mg ritonavir) in healthy volunteers resulted in approximately twofold and fivefold increases in AUC(0-24) and Cmax rosuvastatin, respectively. Therefore, concomitant administration of rosuvastatin and HIV protease inhibitors is not recommended (see Sections “Administration and Doses”, “Special Precautions”, Table 1).
Gemfibrozil and other hypolipidemic agents: Co-administration of rosuvastatin and gemfibrozil leads to a 2-fold increase in maximum plasma concentration of rosuvastatin and AUC of rosuvastatin (see section “Special Precautions”). Based on the data on specific interactions, no pharmacokinetic interaction with fenofibrate is expected, pharmacodynamic interaction is possible.
Hemfibrozil, fenofibrate, other fibrates and lipid-lowering doses of nicotinic acid increased the risk of myopathy when used concomitantly with HMG-CoA reductase inhibitors, possibly due to the fact that they may cause myopathy when used in monotherapy (see section “Special Instructions”). In concomitant use of the drug with gemfibrozil, fibrates, nicotinic acid in lipid-lowering doses (more than 1 g/day), patients are recommended the initial dose of the drug is 5 mg, taking a dose of 40 mg is contraindicated when combined with fibrates (see sections “Contraindications”, “Dosage and administration”, “Cautions”).
Ezetimibe: concomitant use of rosuvastatin in dose
10 mg and ezetimibe in dose
10 mg was accompanied by increased AUC of rosuvastatin in patients with hypercholesterolemia (see Table 1). An increased risk of side effects due to pharmacodynamic interaction between rosuvastatin and ezetimibe cannot be excluded.
Antacids: Concomitant use of rosuvastatin and suspensions of antacids containing magnesium and aluminum hydroxide leads to a decrease in plasma concentration of rosuvastatin by approximately 50%. This effect is weaker if antacids are used 2 hours after rosuvastatin administration. The clinical significance of this interaction has not been studied.
Eritromycin: Concomitant use of rosuvastatin and erythromycin leads to a decrease in AUC of rosuvastatin by 20% and Cmax of rosuvastatin by 30%. This interaction may occur as a result of increased intestinal motility caused by taking erythromycin.
Cytochrome P450 isoenzymes:the results of in vivo and in vitro studies showed that rosuvastatin is neither an inhibitor nor an inducer of cytochrome P450 isoenzymes. In addition, rosuvastatin is a weak substrate for these isoenzymes. Therefore, no interaction of rosuvastatin with other drugs at the level of metabolism involving cytochrome P450 isoenzymes is expected. No clinically significant interaction of rosuvastatin with fluconazole (CYP2C9 and CYP3A4 isoenzymes inhibitor) and ketoconazole (CYP2A6 and CYP3A4 isoenzymes inhibitor) was observed.
Fusidic acid:There have been no studies on the interaction between rosuvastatin and fusidic acid. As with other statins, in post-registration use of rosuvastatin, there have been reports of cases of rhabdomyolysis when co-administering rosuvastatin and fusidic acid. Close monitoring of patients is necessary. If necessary, temporary discontinuation of Rosuvastatin-Teva is possible.
Interactions with drugs that require dose adjustment of rosuvastatin (see Table 1)
The dose of rosuvastatin should be adjusted if its co-administration with drugs that increase the AUC of rosuvastatin is necessary. If the AUC is expected to increase 2-fold or more, the starting dose of rosuvastatin should be 5 mg once daily. The maximum daily dose of rosuvastatin should also be adjusted so that the expected AUC of rosuvastatin does not exceed that of a dose of 40 mg taken without concomitant administration of drugs that interact with rosuvastatin. For example, the maximum daily dose of rosuvastatin when concomitantly used with gemfibrozil is 20 mg (1.9-fold increase in exposure), with ritonavir/atazanavir is 10 mg (3.1-fold increase in AUC).
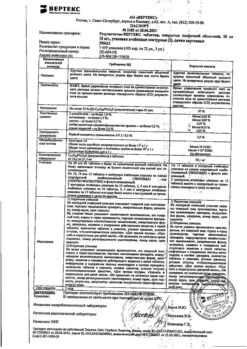
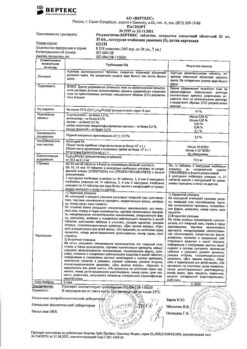
Table 1. Effect of concomitant therapy on rosuvastatin exposure (AUC, data are given in descending order) – results of published clinical trials.
Mode of concomitant therapy
Regime of taking rosuvastatin
Changing the AUC of rosuvastatin
Cyclosporine 75-200 mg
2 times daily, 6 months.
10 mg once daily,
10 days
7.1-fold increase
Regorafenib 160 mg,
once daily, 14 days
/p>
5 mg once
3.8-fold increase
Atazanavir 300 mg/ritonavir 100 mg
once daily, 8 days
10 mg once
3.1-fold increase
Simeprevir 150 mg
once daily, 7 days
10 mg once
Increased 2.8-fold
Velpatasvir 100 mg
/p>
once daily
10 mg once
Increase by 2.7 times
Ombitasvir 25 mg/Paritaprevir 150 mg/Ritonavir 100 mg once daily
Dasabuvir 400 mg
2 times daily, 14 days
5 mg once
Increase by 2.6 times
20 mg once daily,
7 days
Increased 2.1-fold
Clopidogrel 300 mg (loading dose), then 75 mg after 24 h
/p>
20 mg once
Increasing 2-fold
Gemfibrozil 600 mg 2 times daily, 7 days
80 mg once
1.9-fold increase
Eltrombopag 75 mg once daily, 10 days
10 mg once
1.6-fold increase
Darunavir 600 mg/ritonavir 100 mg
p> 2 times daily, 7 days
10 mg once daily,
7 days
1.5-fold increase
Tipranavir 500 mg/ritonavir 200 mg
/p>
2 times daily, 11 days
10 mg once
Increased 1.4 times
Dronedarone 400 mg 2 times daily
No data
1.4-fold increase
Itraconazole 200 mg
once daily, 5 days
10 mg or 80 mg once
1.4-fold increase
Ezetimibe 10 mg once daily, 14 days
10 mg once daily,
14 days
1.2-fold increase
Fosamprenavir 700 mg/ritonavir 100 mg
2 times daily, 8 days
once
No change
Aleglitazar 0.3 mg, 7 days
40 mg, 7 days
No change
Silymarin 140 mg 3 times daily, 5 days
10 mg once
No change
Fenofibrate 67 mg 3 times daily, 7 days
/td>
10 mg, 7 days
No change
Rifampicin 450 mg once daily, 7 days
20 mg once
No change
Ketoconazole 200 mg 2 times daily, 7 days
/p>
80 mg once
No change
Fluconazole 200 mg once daily, 11 days
80 mg once
No change
Erythromycin 500 mg 4 times daily, 7 days
80 mg once
28% reduction
Baicalin 50 mg 3 times daily, 14 days
20 mg once
47% reduction
.Influence of rosuvastatin use on other drugs
Vitamin K antagonists:The initiation of rosuvastatin therapy or increasing the dose of the drug in patients receiving concomitant vitamin K antagonists (e.g., warfarin) may result in an increase in the international normalized ratio (INR). Discontinuation of rosuvastatin or reduction of its dose may lead to a decrease in INR. INR control is recommended in such cases.
Incontinuous oral contraceptives/hormone replacement therapy: Concomitant use of rosuvastatin and oral contraceptives increases AUC of ethinylestradiol and AUC of nogestrel by 26% and 34%, respectively. This increase in plasma concentration should be considered when selecting a dose of oral contraceptives. There are no pharmacokinetic data on the simultaneous use of rosuvastatin and hormone replacement therapy, therefore, a similar effect cannot be excluded when using this combination. However, this combination was widely used during clinical trials and was well tolerated by patients.
Other drugs:no clinically significant interaction of rosuvastatin with digoxin is expected.
Special Instructions
Special Instructions
Influence on renal function
In patients receiving high doses of rosuvastatin (mainly 40 mg), tubular proteinuria was observed, which in most cases was transient. Such proteinuria was not indicative of acute kidney disease or progression of renal disease. In patients taking rosuvastatin at a dose of 40 mg, it is recommended to monitor renal function parameters during treatment.
Motor system disorders
The following musculoskeletal effects have been reported with rosuvastatin at all doses and particularly with doses above 20 mg: Myalgia, myopathy, rhabdomyolysis (in rare cases).
Creatine phosphokinase (CPK)
The determination of CPK activity should not be performed after intense physical activity or in the presence of other possible causes of increased CPK activity, which may lead to misinterpretation of the results. If the baseline CPK activity is significantly elevated (5 times higher than VGN), a repeat measurement should be performed after 5-7 days. The therapy should not be started if the repeat test confirms the initial CPK activity (higher by more than 5 times compared to IGN).
Before initiating therapy
Before using rosuvastatin, as well as before using other HMG-CoA reductase inhibitors, the risk-benefit ratio of therapy in patients with existing risk factors for myopathy/rhabdomyolysis should be considered (see section “Caution.
Cautions should be taken and these patients should be closely monitored by a physician.
At the time of treatment
The patient should be informed to inform the physician immediately if new, previously unreported symptoms of unexplained muscle pain, muscle weakness or seizures occur, especially if combined with malaise and fever. In such patients, CPK activity should be determined. Therapy should be discontinued if CPK activity is significantly increased (more than 5-fold compared to IGN) or if muscle symptoms and daily discomfort are acute (even if CPK activity is 5-fold lower than IGN). If symptoms disappear and CPK activity returns to normal, re-administration of rosuvastatin or other HMG-CoA reductase inhibitors at lower doses with close patient monitoring should be considered.
Routine monitoring of CPK activity in the absence of the symptoms described above is not advisable.
There have been very rare cases of immune-mediated necrotizing myopathy with clinical manifestations as persistent proximal muscle weakness and elevated plasma CPK activity during therapy or upon discontinuation of statins, including rosuvastatin. Additional muscular and nervous system studies, serologic studies, and therapy with immunosuppressive agents may be required.
There have been no indications of increased skeletal muscle effects with rosuvastatin and concomitant therapy. However, an increase in myositis and myopathy has been reported in patients taking other HMG-CoA reductase inhibitors in combination with fibrin acid derivatives, including gemfibrozil, cyclosporine, nicotinic acid, azole antifungals, protease inhibitors and macrolide antibiotics. Gemfibrozil increases the risk of myopathy when concomitantly prescribed with some HMG-CoA reductase inhibitors. Thus, concomitant administration of rosuvastatin and gemfibrozil is not recommended.
The risk/benefit ratio of co-administration of rosuvastatin and fibrates or lipid-lowering doses of nicotinic acid should be carefully weighed. Rosuvastatin at a dose of 40 mg in combination with fibrates is contraindicated (see sections “Contraindications” and “Interactions with other medicinal products”).
Two to four weeks after the start of treatment and/or when increasing the dose of Rosuvastatin-Teva it is necessary to monitor lipid metabolism parameters; if necessary, the dose of the drug is adjusted.
Influence on liver function
The determination of liver function parameters before the start of therapy and 3 months after the start of therapy is recommended. Rosuvastatin should be discontinued or the dose should be reduced if plasma hepatic transaminase activity is 3 times greater than BHF.
In patients with hypercholesterolemia due to hypothyroidism or nephrotic syndrome, therapy for underlying diseases should be performed before starting rosuvastatin.
There are no data or experience with rosuvastatin in patients with severe hepatic impairment (above 9 points on the Child-Pugh score).
Special populations. Ethnic groups
In pharmacokinetic studies in Chinese and Japanese patients, increased systemic concentrations of rosuvastatin have been observed compared to those obtained in European patients (see sections “Pharmacokinetics” and “Administration and Doses”).
HIV protease inhibitors
The co-administration of rosuvastatin with HIV protease inhibitors is not recommended (see section “Interaction with other medicinal products”).
Interstitial lung disease
Single cases of interstitial lung disease have been reported with some statins, especially for long periods of time. Manifestations of the disease may include dyspnea, non-productive cough, and deterioration in general well-being (weakness, weight loss, and fever). If interstitial lung disease is suspected, statin therapy should be discontinued.
Type 2 diabetes mellitus
In patients with glucose concentrations between 5.6 and 6.9 mmol/L, rosuvastatin therapy has been associated with an increased risk of developing type 2 diabetes mellitus.
Influence on ability to drive vehicles and mechanisms
There have been no studies on the effect of the drug Rosuvastatin-Teva on the ability to drive vehicles and mechanisms. When using Rosuvastatin-Teva, caution should be exercised when driving vehicles or working that requires high concentration and quick psychomotor reactions.
Synopsis
Synopsis
Tablets 5 mg. Circular biconvex film-coated tablets, light yellow or light orange (grayish tint possible) to orange in color, engraved “N” on one side and “5” on the other.
Tablets 10 mg. Circular biconvex film-coated tablets, light pink to pink in color, engraved “N” on one side and “10” on the other.
Tablets 20 mg. Circular biconvex film-coated tablets, light pink to pink in color, engraved “N” on one side and “20” on the other.
Tablets 40 mg. Oval film-coated tablets, light pink to pink in color, engraved “N” on one side and “40” on the other.
Contraindications
Contraindications
For doses of the drug of 5 mg, 10 mg, 20 mg:
Side effects
Side effects
NRs observed when taking Rosuvastatin-Teva are usually mild and go away on their own. As with other HMG-CoA reductase inhibitors, the incidence of HF is mostly dose-dependent.
The incidence of side effects is given according to the following classification: Very common (>1/10); common (>1/100, <1/10); infrequent (>1/1000, <1/100); rare (>1/10,000, <1/1000); very rare (<1/10,000); frequency unknown (cannot be determined from available data).
Immune system disorders: Rarely, hypersensitivity reactions, including angioedema.
Endocrine system disorders:often – diabetes mellitus type 2.
Nervous system disorders:often – headache, dizziness; frequency unknown – peripheral neuropathy.
Gastrointestinal tract disorders:often – constipation, nausea, abdominal pain; rarely – pancreatitis.
Hepatic and biliary tract disorders: when using rosuvastatin there is a dose-dependent increase in the activity of “hepatic” transaminases in a small number of patients. In most cases it is mild, asymptomatic and temporary.
Skin and subcutaneous tissue disorders: infrequent – skin itching, skin rash, urticaria.
Muscular and connective tissue disorders:often – myalgia; rarely – myopathy (including myositis), rhabdomyolysis, lupus-like syndrome, muscle rupture.
When using Rosuvastatin-Teva at all doses, and especially when taking doses of the drug greater than 20 mg, the following musculoskeletal effects have been reported: myalgia, myopathy (including myositis), in rare cases – rhabdomyolysis with or without acute renal failure. A dose-dependent increase in creatine phosphokinase (CPK) activity was observed in a small number of patients taking rosuvastatin. In most cases it was insignificant, asymptomatic and temporary. In the case of an increase in CPK activity (more than 5-fold that of IGN), therapy should be suspended.
Kidney and urinary tract disorders: Proteinuria may be detected in patients receiving Rosuvastatin-Teva. Changes in the amount of protein in the urine (from no or trace amounts to ++ or more) are observed in less than 1% of patients receiving the drug at a dose of 10-20 mg, and in approximately 3% of patients receiving the drug at a dose of 40 mg. Little change in urine protein has been observed with the 20 mg dose. In most cases, proteinuria decreases or disappears during therapy and does not indicate the occurrence of acute or progression of existing renal disease.
General disorders and disorders at the site of administration:Asthenic syndrome is common.
Laboratory and instrumental data:the following changes in laboratory parameters have also been observed when using rosuvastatin: increased glucose concentration, increased bilirubin concentration, increased gammaglutamyltransferase activity, increased alkaline phosphatase activity, thyroid function disorders.
Post-marketing use
The following HPs have been reported in the post-marketing use of rosuvastatin:
Disorders of the blood and lymphatic system: frequency unknown- thrombocytopenia.
Mental disorders:frequency unknown – depression, sleep disorders, including insomnia and “nightmares” dreams.
Nervous system disorders:very rare – loss or impairment of memory; frequency unknown – peripheral neuropathy.
Disorders of the respiratory system, chest and mediastinum: frequency unknown – cough, dyspnea, interstitial lung disease (especially with long-term use).
Gastrointestinal disorders:very rare – jaundice, hepatitis; frequency unknown – diarrhea.
Liver and biliary tract disorders: frequently – increased activity of “hepatic” transaminases.
Dermatological and subcutaneous tissue disorders:frequency unknown – Stevens-Johnson syndrome.
Muscular and connective tissue disorders:very rare – arthralgia; frequency unknown – immune-mediated necrotizing myopathy.
Kidney and urinary tract disorders:very rare – hematuria.
Renital and mammary gland disorders: frequency unknown – sexual dysfunction, gynecomastia.
General disorders and disorders at the site of administration:frequency unknown – peripheral edema.
The following HRs have been reported with some statins: depression, sleep disturbances including insomnia and “nightmares” dreams, sexual dysfunction, hyperglycemia, increased concentration of glycosylated hemoglobin. Single cases of interstitial lung disease have been reported, especially with long-term drug use.
Overdose
Overdose
Pregnancy use
Pregnancy use
Similarities
Similarities
Additional information
| Shelf life | 2 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | Store at a temperature not exceeding 25 °C. Keep out of reach of children! |
| Manufacturer | Teva LLC, Russia |
| Medication form | pills |
| Brand | Teva LLC |
Other forms…
Related products
Buy Rosuvastatin, 10 mg 90 pcs with delivery to USA, UK, Europe and over 120 other countries.