No products in the cart.
Rosucard, 10 mg 30 pcs
€24.42 €20.35
Description
Rosucard is a hypolipidemic drug from the group of statins. It is a selective competitive inhibitor of Z-hydroxy-Z-methylglutaryl coenzyme A (HMG-CoA)-reductase – the enzyme that converts HMG-CoA into mevalonate, a precursor of cholesterol (CH).
Lincreases the number of low-density lipoprotein (LDL) receptors on the surface of hepatocytes, which leads to increased capture and catabolism of LDL, inhibiting the synthesis of very low-density lipoprotein (VLDL), reducing the total concentration of LDL and VLDL. Reduces concentrations of CH-LDL, high-density cholesterol-non-lipoproteins (HDL-C), LDL-C, total CH, triglycerides (TG), TG-LDL-C, apolipoprotein B (ApoB), decreases the ratios of CH-LDL/HC-LDL, total CH/CH-LDL, non-HC-LDL/HC-LDL, apoB/apolipoprotein A-1 (apoA-I), increases concentrations of CH-LDL and apoA-I.
The hypolipidemic effect is directly proportional to the dose prescribed. Therapeutic effect appears within 1 week after the start of therapy, after 2 weeks it reaches 90% of maximum, by 4 weeks it reaches maximum and after that it remains constant.
It is effective in adult patients with hypercholesterolemia with or without hypertriglyceridemia (regardless of race, sex or age), including patients with diabetes and familial hypercholesterolemia. In 80% of patients with hypercholesterolemia of IIa and IIb types (classification according to Fredrickson) with baseline mean concentration of CH-LDL about 4.8 mmol / L against the drug administration in a dose of 10 mg, HC-LDL concentration reaches values less than 3 mmol / L. In patients with homozygous familial hypercholesterolemia taking the drug in doses of 20 mg and 40 mg the mean decrease of LDL-C concentration is 22%.
Additive effect is noted in combination with fenofibrate (in regard to decrease of TG concentration and with nicotinic acid in lipid-lowering doses (at least 1 g/day) (in regard to decrease of HDL-C concentration).
Indications
Indications
Primary hypercholesterolemia (type IIa according to Fredrickson), including heterozygous hereditary hypercholesterolemia or mixed (combined) hypercholesterolemia (type IIb according to Fredrickson), as an addition to diet and other non-drug measures (physical activity and weight loss) when diet therapy and non-drug measures are ineffective;
Homozygous form of hereditary hypercholesterolemia and when diet therapy and other treatments aimed at lowering lipid levels (eg, LDL apheresis) are insufficiently effective, or if such treatments are not suitable for the patient.
Hypertriglyceridemia (Fredrickson type IV) as an adjunct to diet.
To slow the progression of atherosclerosis as an addition to diet in patients who are indicated for therapy to reduce the concentration of total cholesterol and LDL cholesterol.
Prevention of major cardiovascular complications (stroke, heart attack, arterial revascularization) in adult patients without clinical signs of coronary heart disease (CHD), but with an increased risk of its development (age over 50 years for men and over 60 years for women, increased concentration of C-reactive protein (≥ 2 mg/l) in the presence of at least one of the additional risk factors, such as arterial hypertension, low HDL-C concentration, smoking, family history of early onset ischemic heart disease).
Pharmacological effect
Pharmacological effect
Rosucard is a lipid-lowering drug from the group of statins. Selective competitive inhibitor of 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase, an enzyme that converts HMG-CoA into mevalonate, a precursor of cholesterol (CH).
Increases the number of low-density lipoprotein (LDL) receptors on the surface of hepatocytes, which leads to increased uptake and catabolism of LDL, inhibition of the synthesis of very low-density lipoproteins (VLDL), reducing the total concentration of LDL and VLDL. Reduces the concentrations of LDL-C, high-density non-lipoprotein cholesterol (non-HDL-C), VLDL-C, total cholesterol, triglycerides (TG), VLDL-TG, apolipoprotein B (ApoB), reduces the LDL-C/HDL-C ratio, total cholesterol/HDL-C, non-HDL-C/HDL-C, ApoB/apolipoprotein A-1 (ApoA-I), increases the concentrations of HDL-C and ApoA-I.
The lipid-lowering effect is directly proportional to the prescribed dose. The therapeutic effect appears within 1 week after the start of therapy, after 2 weeks it reaches 90% of the maximum, by 4 weeks it reaches a maximum and after that remains constant.
Effective in adult patients with hypercholesterolemia with or without hypertriglyceridemia (regardless of race, sex or age), including patients with diabetes mellitus and familial hypercholesterolemia. In 80% of patients with type IIa and IIb hypercholesterolemia (Fredrickson classification) with an average initial LDL-C concentration of about 4.8 mmol/L, when taking the drug at a dose of 10 mg, the LDL-C concentration reaches values of less than 3 mmol/L. In patients with homozygous familial hypercholesterolemia taking the drug at a dose of 20 mg and 40 mg, the average reduction in LDL-C concentration is 22%.
An additive effect is observed in combination with fenofibrate (in terms of reducing the concentration of TG and with nicotinic acid in lipid-lowering doses (at least 1 g/day) (in terms of reducing the concentration of HDL-C).
Special instructions
Special instructions
During treatment, especially during the period of dose adjustment of the drug Rosucard®, the lipid profile should be monitored every 2-4 weeks and the dose of the drug should be changed if necessary.
It is recommended to determine liver function indicators before starting therapy and 3 months after starting therapy. Taking Rosucard® should be stopped or the dose reduced if the level of hepatic transaminase activity in the blood serum is 3 times higher than the ULN.
When using the drug Rosucard® at a dose of 40 mg, it is recommended to monitor kidney function indicators.
In patients with hypercholesterolemia due to hypothyroidism or nephrotic syndrome, treatment of underlying diseases should be carried out before starting treatment with Rosucard®.
In patients with existing risk factors for rhabdomyolysis, it is necessary to consider the balance of expected benefit and potential risk and conduct clinical monitoring throughout the course of treatment.
The patient should be informed of the need to immediately report to the doctor if muscle pain, muscle weakness or cramps occur, especially in combination with malaise and fever.
In such patients, CPK activity should be determined. Therapy should be discontinued if CPK activity is significantly increased (more than 5 times the ULN) or muscle symptoms are severe and cause daily discomfort. If symptoms disappear and CPK activity returns to normal, re-prescribing Rosucard® or other HMG-CoA reductase inhibitors in lower doses should be considered with careful monitoring of the patient.
Determination of CPK activity should not be carried out after intense physical activity or in the presence of other possible reasons for its increase, which may lead to incorrect interpretation of the results obtained. If the initial CPK activity is significantly increased, a repeat measurement should be taken after 5-7 days; therapy cannot be started if a repeat test confirms the initial CPK activity (5 times higher than normal).
Routine monitoring of CPK activity in the absence of the above-described symptoms is impractical.
An increased incidence of myositis and myopathy has been reported in patients taking other HMG-CoA reductase inhibitors in combination with fibrates (including gemfibrozil), cyclosporine, niacin, azole antifungals, protease inhibitors and macrolide antibiotics. The ratio of expected benefits and potential risks should be carefully weighed when using the drug Rosucard® together with fibrates or nicotinic acid (in lipid-lowering doses – 1 g / day); simultaneous administration of gemfibrozil is not recommended.
In most cases, proteinuria decreases or disappears during therapy and does not indicate the occurrence of acute or exacerbation of existing kidney disease. Renal function should be assessed during routine assessment of patients receiving the 40 mg dose.
Drugs of the statin class can cause an increase in blood glucose concentrations. In some patients at high risk of developing diabetes mellitus, such changes may lead to its manifestation, which is an indication for the administration of hypoglycemic therapy. However, the reduction in the risk of vascular diseases while taking statins exceeds the risk of developing diabetes, so this factor should not serve as a basis for discontinuing statin treatment. Patients at risk (fasting blood glucose concentration 5.6–6.9 mmol/l, BMI >30 kg/m2, hypertriglyceridemia, history of arterial hypertension) should be under medical supervision and regularly monitor biochemical parameters.
Co-administration of rosuvastatin and HIV protease inhibitors is not recommended.
Isolated cases of interstitial lung disease have been reported with long-term use of rosuvastatin. If interstitial lung disease is suspected, therapy with Rosucard® should be discontinued.
When studying the pharmacokinetic parameters of rosuvastatin, an increase in the systemic concentration of the drug was noted in representatives of the Mongoloid race (see “Pharmacokinetics”). This fact should be taken into account when prescribing the drug Rosucard® to these patients.
Impact on the ability to drive vehicles and operate machinery. Caution should be exercised when driving vehicles and doing activities that require increased concentration and speed of psychomotor reactions (dizziness may occur during therapy).
Active ingredient
Active ingredient
Rosuvastatin
Composition
Composition
1 tab. – rosuvastatin calcium 10.4 mg, which corresponds to the content of rosuvastatin 10 mg.
Excipients:
lactose monohydrate – 60 mg,
microcrystalline cellulose – 45.4 mg,
croscarmellose sodium – 1.2 mg,
colloidal silicon dioxide – 600 mcg,
magnesium stearate – 2.4 mg.
Film shell composition:
hypromellose 2910/5 – 2.5 mg, macrogol 6000 – 400 mcg, titanium dioxide – 325 mcg, talc – 475 mcg, red iron oxide dye – 13 mcg.
Pregnancy
Pregnancy
The drug is contraindicated during pregnancy, lactation and under the age of 18 years
Contraindications
Contraindications
Hypersensitivity;
Liver disease in the active phase or a sustained increase in serum activity of “liver” transaminases (more than 3 times compared to the upper limit of normal) of unknown origin, liver failure (severity from 7 to 9 points on the Child-Pugh scale);
An increase in the concentration of creatinine phosphokinase (CPK) in the blood by more than 5 times compared to the upper limit of normal (ULN);
Hereditary diseases such as lactose intolerance, lactase deficiency or glucose-galactose malabsorption (due to the presence of lactose);
Severe renal dysfunction (creatinine clearance less than 30 ml/min);
Myopathy;
Patients predisposed to the development of myotoxic complications;
Concomitant use of cyclosporine;
Combined use with HIV protease inhibitors;
Women of reproductive age who do not use adequate methods of contraception.
Side Effects
Side Effects
From the central nervous system: often – headache, dizziness, asthenic syndrome; very rarely – peripheral neuropathy, memory loss.
From the digestive system: often – nausea, constipation, abdominal pain; infrequently – vomiting; rarely – pancreatitis; very rarely – hepatitis, jaundice; unspecified frequency – diarrhea.
From the respiratory system: infrequently – cough, dyspnea.
From the endocrine system: often – type 2 diabetes mellitus.
From the musculoskeletal system: often – myalgia; very rarely – arthralgia; rarely – myopathy (including myositis), rhabdomyolysis.
Allergic reactions: uncommon – itching, urticaria, rash; rarely – angioedema.
Skin and subcutaneous tissue: frequency not specified – Stevens-Johnson syndrome, peripheral edema.
From the urinary system: often – proteinuria (with a frequency of more than 3% in patients receiving a dose of 40 mg), decreasing during therapy and not associated with the occurrence of kidney disease, urinary tract infections; very rarely – hematuria.
Laboratory indicators: infrequently – a transient dose-dependent increase in the activity of serum creatine phosphokinase (CPK), with an increase of more than 5 times compared to the upper limit of normal, therapy should be temporarily suspended; rarely – transient increase in the activity of aspartate aminotransferase and alanine aminotransferase.
As with the use of other HMG-CoA reductase inhibitors, the incidence is dose-dependent, side effects are usually mild and go away on their own.
When using ROZUKARD®, changes in the following laboratory parameters were observed: increased concentrations of glucose, bilirubin, alkaline phosphatase activity, gamma-glutamyltransferase.
The following side effects have been reported with other statins: depression, insomnia, decreased potency.
Isolated cases of interstitial lung disease have been reported with long-term use of rosuvastatin.
Interaction
Interaction
The simultaneous use of rosuvastatin and cyclosporine does not affect the plasma concentration of cyclosporine, however, the effect of rosuvastatin is enhanced (its elimination slows down, AUC increases by 7 times, Cmax increases by 11 times).
Erythromycin increases intestinal motility, which leads to a decrease in the effect of rosuvastatin (AUC decreases by 20% and Cmax by 30%).
In patients receiving vitamin K antagonists (eg, warfarin), monitoring of the international normalized ratio (INR) is recommended, since initiating rosuvastatin therapy or increasing the dose of the drug may lead to an increase in the INR, and discontinuation of rosuvastatin or reducing its dose may lead to a decrease. Gemfibrozil enhances the effect of rosuvastatin (increases Cmax and AUC by 2 times). The simultaneous use of rosuvastatin and antacids containing aluminum and magnesium hydroxide leads to a decrease in the plasma concentration of rosuvastatin by approximately 50%. This effect is less pronounced if antacids are used 2 hours after taking rosuvastatin.
The simultaneous use of rosuvastatin and oral contraceptives increases the AUC of ethinyl estradiol and AUC of norgestrel by 26% and 34%, respectively, which should be taken into account when selecting the dose of oral contraceptives. There are no pharmacokinetic data on the simultaneous use of rosuvastatin and hormone replacement therapy; therefore, a similar effect cannot be excluded when using this combination.
The research results showed that rosuvastatin is neither an inhibitor nor an inducer of the action of cytochrome P450 isoenzymes. Rosuvastatin is a non-core substrate for these isoenzymes. No clinically significant interactions were observed with drugs such as fluconazole, ketoconazole and itraconazole, which are metabolized by the cytochrome P450 system.
There is no clinically significant interaction of rosuvastatin with digoxin or fenofibrate; Gemfibrozil, other fibrates and lipid-lowering doses of nicotinic acid (at least 1 g/day) increased the risk of myopathy when used simultaneously with other HMG-CoA reductase inhibitors. Possibly due to the fact that they can cause myopathy when used as monotherapy.
The combined use of rosuvastatin and ezetimibe did not lead to changes in the AUC or Cmax of both drugs.
The use of HIV (human immunodeficiency virus) protease inhibitors with rosuvastatin can lead to a significant increase in the effect of rosuvastatin. A pharmacokinetic study of co-administration of 20 mg rosuvastatin and a combination of two HIV protease inhibitors (400 mg lopinavir/100 mg ritonavir) in healthy volunteers resulted in approximately two- and five-fold increases in AUC(0-24) and Cmax, respectively. Therefore, co-administration of rosuvastatin with HIV protease inhibitors is not recommended in patients infected with HIV.
Overdose
Overdose
When taking several daily doses simultaneously, the pharmacokinetic parameters of rosuvastatin do not change.
Treatment: there is no specific treatment; symptomatic therapy is carried out to maintain the functions of vital organs and systems.
Monitoring of liver function indicators and CPK activity is necessary. Hemodialysis is ineffective.
Storage conditions
Storage conditions
At a temperature not exceeding 30 °C
Shelf life
Shelf life
2 years
Manufacturer
Manufacturer
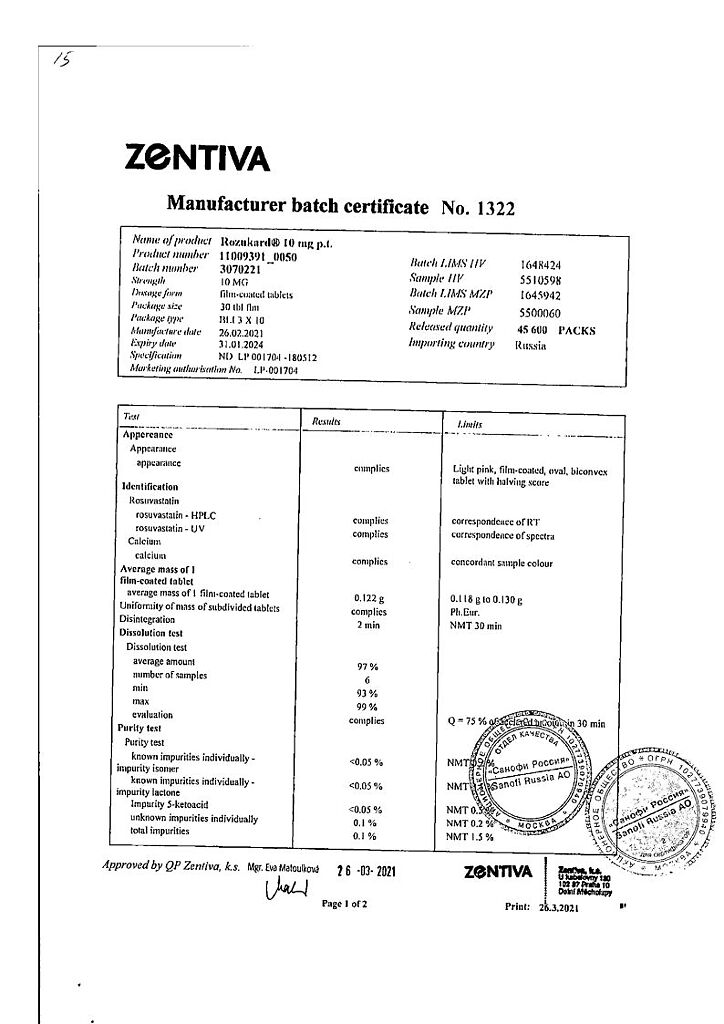
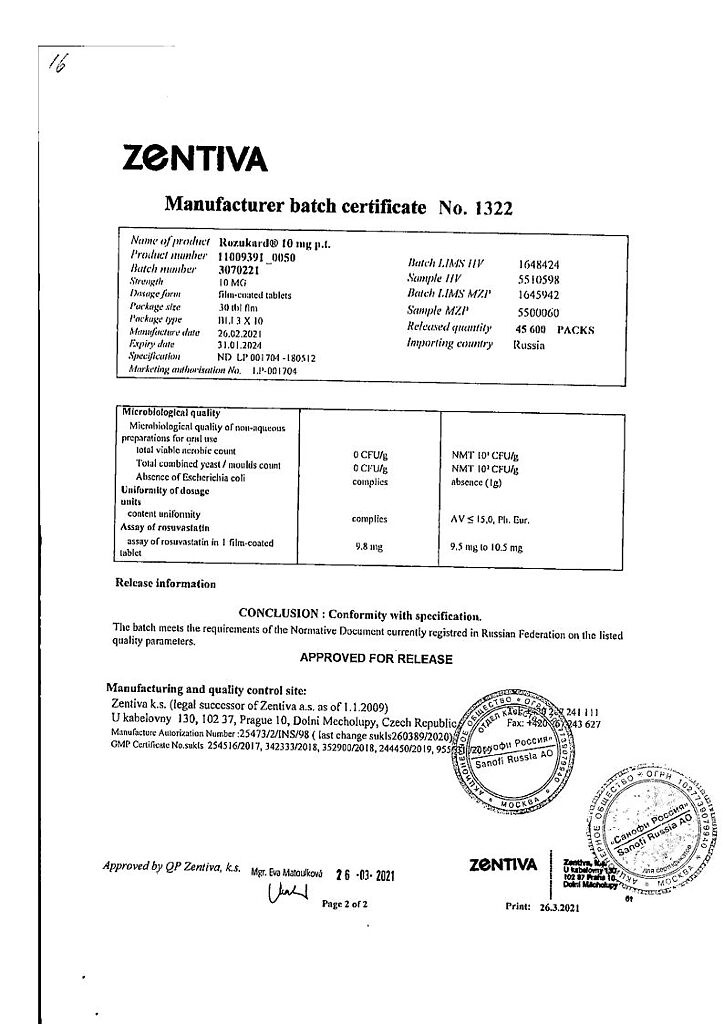
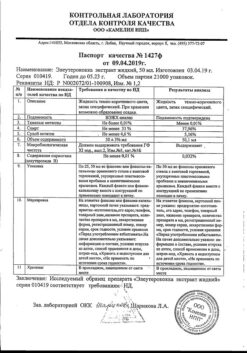
Zentiva k.s., Czech Republic
Additional information
| Shelf life | 2 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 30 °C |
| Manufacturer | Zentiva k.s., Czech Republic |
| Medication form | pills |
| Brand | Zentiva k.s. |
Other forms…
Related products
Buy Rosucard, 10 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.