No products in the cart.
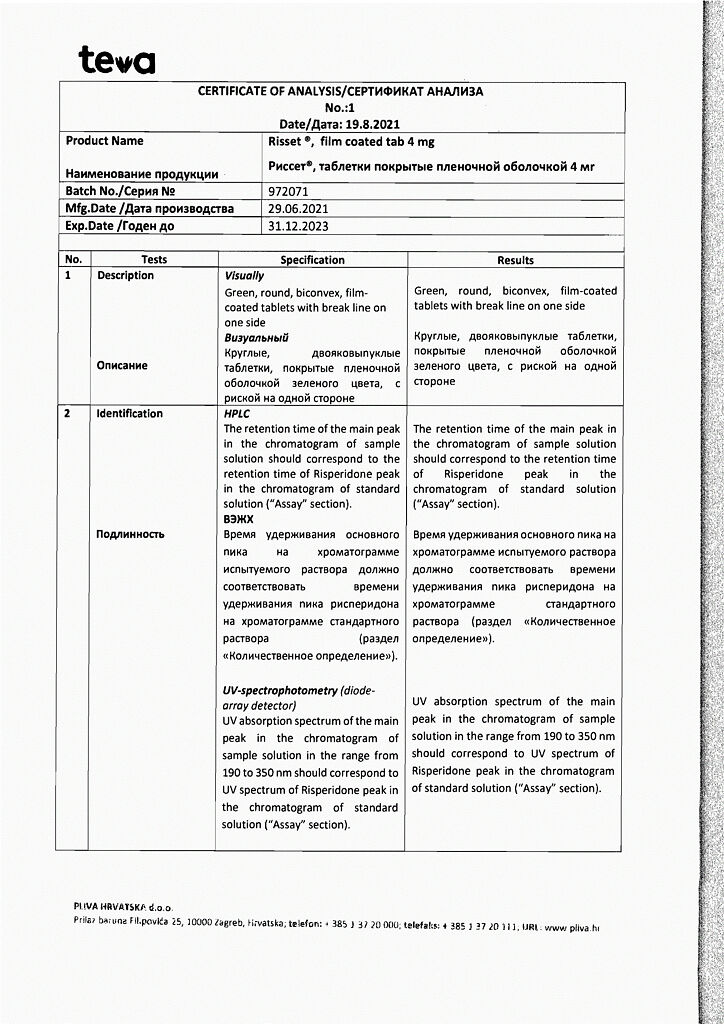
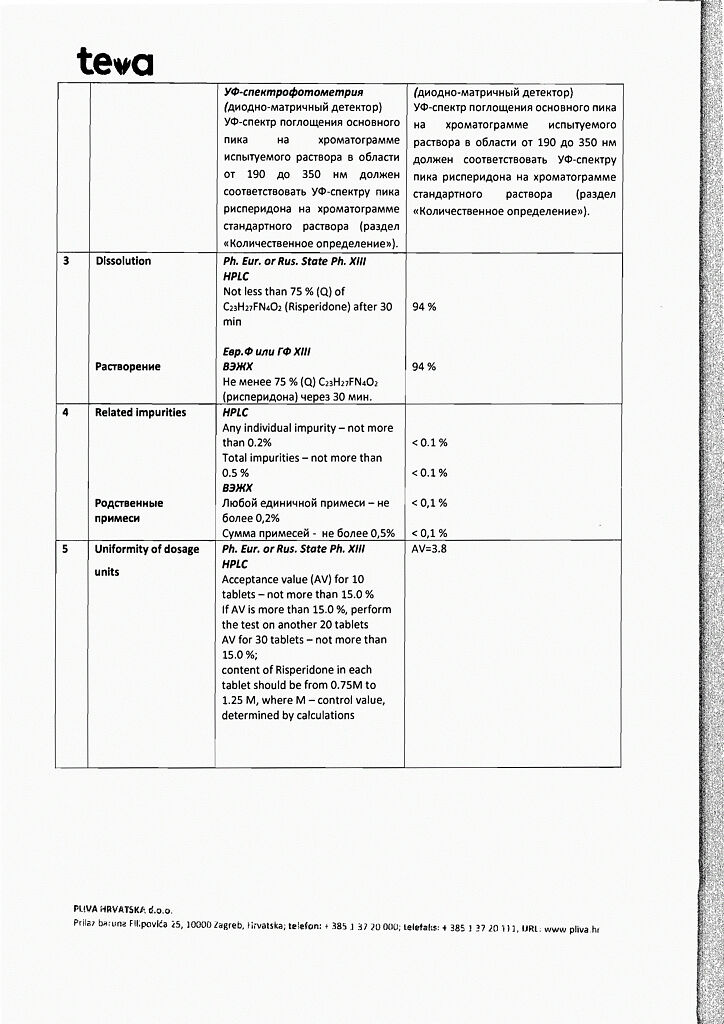
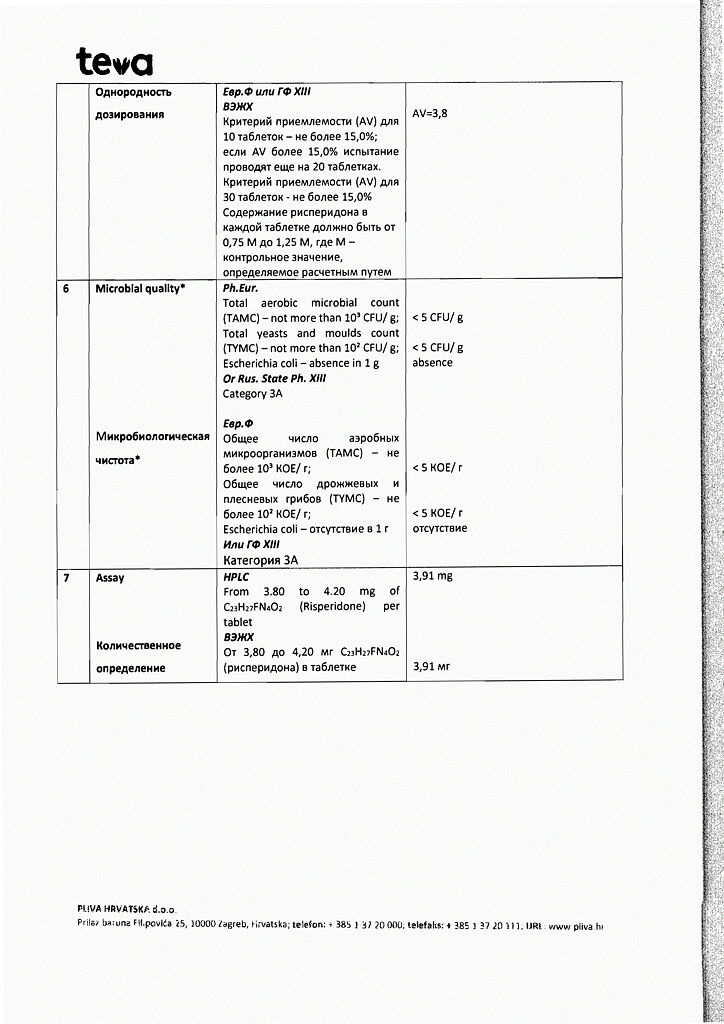
Risset, 4 mg 20 pcs.
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacological group: antipsychotic (neuroleptic).
ATX code: N05AX08
Pharmacological properties
Pharmacodynamics
Risperidone is a selective monoaminergic antagonist with high affinity for serotonergic 5-NT2 and dopaminergic D2 receptors. Risperidone also binds to ɑ1-adrenergic receptors and, somewhat more weakly, to H1-histamine and ɑ2-adrenergic receptors. Risperidone has no tropism to cholinergic receptors. Risperidone reduces the productive symptomatology of schizophrenia, causes less suppression of motor activity, and is less likely to induce catalepsy than classical neuroleptics. Balanced central antagonism to serotonin and dopamine probably reduces the propensity for extrapyramidal side effects and extends the therapeutic effects of the drug to include negative and affective symptoms of schizophrenia.
Pharmacokinetics
Assimilation. Risperidone is completely absorbed after oral administration, reaching maximum plasma concentrations after 1-2 hours. The absolute bioavailability of risperidone after oral administration is 70%. Relative bioavailability after oral administration in tablet form is 94 % compared to risperidone in solution form. Food has no effect on absorption of the drug, therefore risperidone may be prescribed regardless of meals. The equilibrium concentration of risperidone in the body in most patients is reached within 1 day. The equilibrium concentration of 9-hydroxirisperidone is reached within 4-5 days.
Distribution. Risperidone is rapidly distributed in the body. The volume of distribution is 1-2 l/kg. In the blood plasma, risperidone binds to albumin and alpha1-acid glycoprotein. Risperidone is 90% bound by plasma proteins, 9-hydroxysperidone – 77%.
Metabolism and excretion. Risperidone is metabolized by CYP 2D6 isoenzyme to 9-hydroxysperidone, which has similar pharmacological effects to risperidone. Risperidone and 9-hydroxysperidone constitute the active antipsychotic fraction. The CYP 2D6 isoenzyme is subject to genetic polymorphism. In patients with intensive metabolism by CYP 2D6 isoenzyme, risperidone is rapidly converted to 9 – hydroxirisperidone, while in patients with poor metabolism this transformation is much slower. Although patients with intensive metabolism have lower risperidone concentrations and higher 9-hydroxysperidone concentrations than patients with poor metabolism, the total pharmacokinetics of risperidone and 9-hydroxysperidone (active antipsychotic fraction) after one or more doses are similar in patients with intensive and with poor CYP 2D6 metabolism.
The other pathway of risperidone metabolism is N-dealkylation. Studies in vitro on human liver microsomes have shown that risperidone at clinically significant concentrations, in general, does not inhibit the metabolism of drugs undergoing biotransformation by P450 system isoenzymes, including CYP 1A2, CYP 2A6, CYP 2C8/9/10, CYP 2D6, CYP 2E1, CYP WA4 and CYP WA5. One week after the start of the drug 70% of the dose is excreted by the kidneys, 14% – through the intestine. In the urine, risperidone together with 9-hydroxyrisperidone make up 35-45% of the dose. The remaining amount consists of inactive metabolites. After oral administration in patients with psychosis, risperidone is excreted with a half-life (T1/2) of about 3 hours. The T1/2 of 9-hydroxysperidone and the active antipsychotic fraction is 24 hours.
Linearity. The plasma concentration of risperidone is directly proportional to the dose taken in the therapeutic dose range.
Elderly patients and patients with hepatic and renal impairment. After a single dose of risperidone, plasma concentrations of the active antipsychotic fraction were on average 43% higher, the half-life was 38% longer, and clearance was decreased by 30% in elderly patients. In patients with renal insufficiency, an increase in plasma concentration and a decrease in clearance of the active antipsychotic fraction by 60% on average were observed. In patients with hepatic insufficiency plasma concentrations of risperidone did not change, but the average concentration of free fraction of the drug increased by 35%.
Children. Pharmacokinetics of risperidone, 9-hydroxirisperidone and the active antipsychotic fraction in children are comparable to those in adult patients.
The influence of race and smoking. Population pharmacokinetic analysis showed no apparent effect of sex, race, or smoking on the pharmacokinetics of risperidone and the active pharmacokinetic fraction.
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
How to take, the dosage
How to take, the dosage
Ingestion. Food intake has no effect on absorption of the drug. When a dose of less than 0.5 mg is prescribed, it is recommended to start therapy with a drug from another manufacturer that provides the required lower dosage.
Schizophrenia
Adults. Risset® may be prescribed once or twice daily.
The initial dose is 2 mg per day. On day 2, the dose should be increased to 4 mg per day. From that point on, the dose can either be kept at the same level or individually adjusted if necessary. Usually the optimal dose is 4-6 mg per day. In some cases, a slower dose increase and lower starting and maintenance doses may be warranted.
Doses above 10 mg daily have not been shown to be more effective than lower doses and may cause extrapyramidal symptoms. Because the safety of doses above 16 mg daily has not been studied, doses above this level are not recommended.
Elderly patients. The initial dose of 0.5 mg 2 times daily is recommended. The dosage can be increased individually by 0.5 mg 2 times a day to 1-2 mg 2 times a day.
Children from 13 years old. The initial dose of 0.5 mg once daily in the morning or evening is recommended. If necessary, the dosage may be increased at least 24 hours later by 0.5-1 mg daily to the recommended dose of 3 mg daily if well tolerated. Although efficacy has been demonstrated in the treatment of schizophrenia in adolescents at doses of 1-6 mg daily, no additional efficacy has been observed at doses above 3 mg daily, and higher doses have caused more side effects. The use of doses higher than 6 mg daily has not been studied.
Patients who have experienced persistent somnolence are advised to take half of the daily dose twice daily.
Manic episodes associated with bipolar disorder
Adults. The recommended starting dose of the drug is 2 mg per day at a single dose. If necessary, this dose may be increased after at least 24 hours by 1 mg per day. For most patients, the optimal dose is 1-6 mg daily. The use of doses higher than 6 mg daily in patients with manic episodes has not been studied.
As with any symptomatic therapy, the appropriateness of continuing treatment with Risset® should be regularly evaluated and confirmed.
Elderly patients. The starting dose of 0.5 mg twice daily is recommended. The dosage can be increased individually by 0.5 mg 2 times a day to 1-2 mg 2 times a day. Caution is necessary due to limited experience of using the drug in elderly patients.
Children over 10 years of age.
Interaction
Interaction
Pharmacodynamic drug interactions
Drugs that prolong the QT interval. As with other antipsychotics, caution should be exercised when prescribing risperidone with drugs that prolong the QT interval, such as antiarrhythmic agents (quinidine, disopyramide, procainamide, propafenone, amiodarone, sotalol, etc.), tricyclic antidepressants (amitriptyline and others) and tetracyclic antidepressants.), tetracyclic antidepressants (maprotiline etc.), some antihistamines, other antipsychotics, some antimalarials (quinine, mefloquine etc.), drugs causing electrolyte imbalance (hypokalemia, hypomagnesemia), bradycardia or inhibiting hepatic metabolism of risperidone. This list is not exhaustive.
Central agents and alcohol. Risperidone should be used with caution in combination with other centrally acting drugs and substances, especially alcohol, opiates, antihistamines, and benzodiazepines because of the increased risk of sedation.
Levodopa and dopamine receptor agonists. Risperidone may decrease the effectiveness of levodopa and other dopamine receptor agonists. If this combination is necessary, especially in terminal Parkinson’s disease, the lowest effective dose of each drug should be administered.
Psychostimulants Concomitant use of psychostimulants (e.g., methylphenidate) and risperidone may cause extrapyramidal symptoms if the dosage of either or both drugs is changed (see Special Precautions).
Antihypertensive drugs. When using risperidone together with antihypertensive drugs, clinically significant hypotension has been observed in the post-registration period.
Paliperidone. It is not recommended to use risperidone and paliperidone concomitantly, because paliperidone is the active metabolite of risperidone. Concomitant use of a combination of risperidone and paliperidone may lead to increased plasma concentrations of the active antipsychotic fraction.
Interactions related to the pharmacokinetics of the drug
The absorption of risperidone is not affected by food intake. Risperidone is mainly metabolized by CYP 2D6 isoenzyme and to a lesser extent by CYP 3A4 isoenzyme. Risperidone and its active metabolite 9-hydroxyrisperidone are substrates of P-glycoprotein (P-gp). Drugs that affect the activity of CYP 2D6 isoenzyme and drugs that significantly inhibit or induce the activity of CYP 3A4 isoenzyme and/or P-gp may affect the pharmacokinetics of the active antipsychotic fraction of risperidone.
Active inhibitors of CYP isoenzyme 2D6. Concomitant use of risperidone and active CYP 2D6 isoenzyme inhibitors may increase plasma concentrations of risperidone and, to a lesser extent, the active antipsychotic fraction. Higher doses of a potent CYP 2D6 isoenzyme inhibitor may increase the concentration of the active antipsychotic fraction of risperidone (e.g., paroxetine – see below). It is expected that other CYP 2D6 isoenzyme inhibitors, such as quinidine, may have a similar effect on the plasma concentration of risperidone. When initiating or withdrawing therapy with a combination of risperidone and paroxetine, quinidine, or another potent CYP 2D6 isoenzyme inhibitor, especially at higher doses, the dose of risperidone should be adjusted.
Inhibitors of CYP isoenzyme 3A4 and/or P-gp. Combined use of risperidone and potent inhibitors of CYP 3A4 isoenzyme and/or P-gp may significantly increase the plasma concentration of the active antipsychotic fraction of risperidone. When initiating or cancelling therapy with a combination of risperidone and itraconazole or another active inhibitor of CYP 3A4 and/or P-gp isoenzyme, the dose of risperidone should be adjusted.
Inductors of CYP isoenzyme 3A4 and/or P-gp. Co-administration of risperidone with an active inducer of CYP 3A4 isoenzyme and/or P-gp may decrease the plasma concentration of the active antipsychotic fraction of risperidone. When initiating or cancelling therapy with a combination of risperidone and carbamazepine or another active inducer of CYP 3A4 and/or P-gp isoenzyme, the dose of risperidone should be adjusted. The effect of CYP 3A4 isoenzyme inducers occurs over time, so it may take up to 2 weeks before the maximum effect is achieved after the start of administration. Accordingly, if a CYP 3A4 isoenzyme inducer is withdrawn, it may take up to 2 weeks before the effect disappears.
Drugs firmly bound to plasma proteins. When using risperidone concomitantly with drugs that are highly bound to plasma proteins, there is no clinically significant displacement of the drug from the indicated proteins. If concomitant treatment is used, refer to the instructions for use of the respective medication and adjust the doses of the drugs taken if necessary.
Children
Drug interaction studies have only been performed in adult patients. The relevance of the results of these studies in children is unknown. Co-administration of psychostimulants (e.g., methylphenidate) and risperidone in children does not alter the pharmacokinetic parameters and effectiveness of risperidone.
Influence of other drugs on the pharmacokinetics of risperidone
Antibacterial drugs
Anticholinesterase drugs
Special Instructions
Special Instructions
Higher mortality in elderly patients with dementia
Elderly patients with dementia treated with atypical antipsychotics have an increased mortality rate compared to placebo in studies of atypical antipsychotics, including risperidone. For this population, the mortality rate for risperidone was 4.0% for patients taking risperidone compared with 3.1% for placebo. The mean age of patients who died was 86 years (range 67-100 years). Data collected from two extensive observational studies indicate that elderly patients with dementia treated with typical antipsychotics also have a slightly increased risk of death compared with untreated patients. At this time, insufficient data have been collected to estimate this risk accurately. Nor is the cause of the increased risk known. Also, the extent to which the increased mortality may be applicable to antipsychotic medications, rather than to the characteristics of this group of patients, has not been determined.
Combined use with furosemide
.Elderly patients with dementia had increased mortality with concomitant oral administration of furosemide and risperidone (7.3%, mean age 89 years, range 75-97 years) compared with the group taking risperidone alone (3.1%, mean age 84 years, range 70-96 years) and the group taking furosemide alone (4.1%, mean age 80 years, range 67-90 years). Increased mortality in patients taking risperidone together with furosemide was observed in 2 of the 4 clinical trials. Co-administration of risperidone with other diuretics (mainly low-dose thiazide diuretics) was not associated with increased mortality.
No pathophysiologic mechanisms have been identified to explain this observation. Nevertheless, special caution should be exercised when prescribing the drug in such cases. The risk/benefit ratio should be carefully evaluated before prescribing. No increase in mortality has been found in patients taking other diuretics concomitantly with risperidone. Regardless of treatment, dehydration is a common risk factor for mortality and should be carefully controlled in elderly patients with dementia.
In elderly patients with dementia, an increase in cerebrovascular side effects (acute and transient cerebrovascular events), including deaths in patients (mean age 85 years, range 73-97 years), has been observed with risperidone compared to placebo.
Cerebrovascular effects
In placebo-controlled clinical trials, patients with dementia taking certain atypical antipsychotics had an approximately 3-fold increased risk of cerebrovascular side effects. Combined data from 6 placebo-controlled studies including mostly elderly patients with dementia (age over 65 years) demonstrate that cerebrovascular side effects (serious and non-serious) occurred in 3.3% (33/1009) of patients taking risperidone and in 1.2% (8/712) of patients taking placebo. The risk ratio was 2.96 (1.34, 7.50) with a 95% confidence interval. The mechanism of increased risk is unknown. Increased risk has not been ruled out for other antipsychotics, nor for other patient populations. Risperidone should be used with caution in patients with risk factors for stroke. The risk of cerebrovascular side effects is much higher in patients with mixed or vascular dementia compared to patients with Alzheimer’s dementia. Therefore, patients with any type of dementia other than Alzheimer’s should not take risperidone.
Physicians should evaluate the risk/benefit ratio of using risperidone in older patients with dementia, taking into account precursors to stroke risk individually in each patient. Patients and caregivers should be cautioned to immediately report signs and symptoms of cardiovascular events, such as: sudden weakness or immobility/sensitivity in the face, legs, arms, as well as speech difficulties and vision problems. All treatment options should be considered, including discontinuation of risperidone.
Risperidone may only be used for short-term treatment of persistent aggression in patients with moderate to severe dementia due to Alzheimer’s disease, as an adjunct to non-pharmacological correction methods, when they are ineffective or of limited effectiveness, and when there is a risk of harm to the patient himself or others. Patients’ condition and the need for continuation of therapy with risperidone should be continually evaluated.
Ortostatic hypotension
Risperidone has alpha-adrenoblocking activity and therefore may cause orthostatic hypotension in some patients, especially during initial dose adjustment. Clinically significant hypotension has been observed in the post-marketing period when coadministered with antihypertensive drugs. Risperidone should be used with caution in patients with known cardiovascular diseases (e.g., heart failure, myocardial infarction, cardiac conduction disorders, dehydration, hypovolemia or cerebrovascular disease). Appropriate dose adjustment is also necessary. It is recommended to evaluate the possibility of reducing the dose if hypotension occurs.
Leukopenia, neutropenia and agranulocytosis
When using antipsychotic drugs, cases of leukopenia, neutropenia and agranulocytosis have been reported. Patients with a history of clinically significant decrease in leukocyte counts or leukopenia/neutropenia should be monitored during the first months of therapy; if the first signs of clinically significant decrease in leukocyte counts occur without other causes of such changes, the therapy with risperidone should be stopped.
Patients with clinically significant neutropenia should be monitored for fever or other symptoms of infection, and appropriate therapy should be started immediately if such symptoms appear. In patients with severe neutropenia (blood neutrophil granulocyte concentration below 1×109/L) risperidone should be discontinued and blood leukocyte concentrations should be monitored until normal values return.
Late dyskinesia and extrapyramidal disorders
Drugs with dopamine receptor antagonist properties may cause late dyskinesia, which is characterized by rhythmic involuntary movements, primarily of the tongue and/or facial muscles. The occurrence of extrapyramidal symptoms is a risk factor for the development of tardive dyskinesia. If a patient presents with objective or subjective symptoms suggestive of tardive dyskinesia, withdrawal of all antipsychotic medications, including risperidone, should be considered.
Extrapyramidal symptoms and psychostimulants
Particular caution should be exercised when co-administering psychostimulants (e.g., methylphenidate) with risperidone, extrapyramidal symptoms may occur when adjusting the dose of one or both drugs (see See section “Interaction with other medications”).
Malignant neuroleptic syndrome (MNS)
.Antipsychotics, including risperidone, may cause MNS, which is characterized by hyperthermia, muscle rigidity, instability of autonomic nervous system function, depressed consciousness, and elevated serum creatine phosphokinase concentrations. Myoglobinuria (rhabdomyolysis) and acute renal failure may also occur in patients with MNS. If a patient presents with objective or subjective symptoms of MNS, all antipsychotic medications, including risperidone, should be withdrawn immediately.
Parkinson’s disease and dementia with Levi’s corpuscles
Prescribing antipsychotics, including risperidone, to patients with Parkinson’s disease or dementia with Levi’s corpuscles should be done with caution, because both groups of patients have an increased risk for Parkinson’s disease.because both groups of patients have an increased risk of MNS and increased sensitivity to antipsychotics (including blunting of pain sensitivity, confusion, postural instability with frequent falls, and extrapyramidal symptoms). Risperidone may worsen the course of Parkinson’s disease.
Hyperglycemia and Diabetes Mellitus
Hyperglycemia, diabetes and exacerbation of existing diabetes have been observed during treatment with risperidone. Assessing the relationship between the use of atypical antipsychotic drugs and abnormalities in glucose concentrations is difficult because of the possibility of an increased baseline risk of diabetes mellitus in the general population. Given additional influencing factors, the relationship between atypical antipsychotic medication use and hyperglycemia is not fully understood. It is likely that prior treatment weight gain is also a predisposing factor. Ketoacidosis may be very rare and diabetic coma is rare. All patients should be clinically monitored for symptoms of hyperglycemia (such as polydipsia, polyuria, polyphagia, and weakness). Patients with diabetes mellitus should be monitored regularly for worsening blood glucose control.
Body weight gain
A significant increase in body weight has been observed with risperidone treatment. Patients’ body weight should be monitored.
Hyperprolactinemia
Based on the results of studies on tissue cultures, it has been suggested that growth of breast tumor cells may be stimulated by prolactin. Although clinical and epidemiologic studies have not shown a clear association of hyperprolactinemia with antipsychotic medication, caution should be exercised when prescribing risperidone to patients with a history of severe complications. Risperidone should be used with caution in patients with existing hyperprolactinemia and in patients with possible prolactin-dependent tumors.
QT interval prolongationQT
QT interval prolongation has very rarely been observed in the post-marketing follow-up period. As with other antipsychotics, caution should be exercised when prescribing risperidone to patients with known cardiovascular disease, a family history of QT interval prolongation, bradycardia, electrolyte disturbances (hypokalemia, hypomagnesemia), as this may increase the risk of arrhythmogenic effects; and when used in combination with QT interval prolongers.
Convulsions
Risperidone should be used with caution in patients with a history of seizures or with other medical conditions in which the seizure threshold may decrease.
Intraoperative flabby iris syndrome
Intraoperative flabby iris syndrome (ISDS) has been observed during cataract surgery in patients taking medications with anti-alpha-1a-adrenergic effects, including risperidone (see See section “Side Effects”). ISDR may increase the risk of ocular complications during and after surgery. If the patient is taking (or has previously taken) alpha-1a adrenergic receptor antagonists, the surgeon should be informed before surgery.
Priapism
Priapism can occur when taking risperidone because of the alpha-adreno-blocking effects.
Body temperature regulation
Antipsychotic drugs have been attributed such undesirable effects as impairment of the body’s ability to regulate temperature. Caution should be exercised when prescribing risperidone to patients with conditions that may contribute to body temperature, which include: intense physical activity, dehydration of the body, exposure to high external temperatures, or concurrent use of drugs with anticholinergic activity.
Venous thromboembolism
Cases of venous thromboembolism have been reported with antipsychotic drugs. Because patients taking antipsychotic medications are often at risk for venous thromboembolism, all possible risk factors should be identified before and during risperidone treatment, and preventive measures should be taken.
Children and adolescents
Before prescribing risperidone, children or adolescents with mental retardation should be carefully evaluated for physical or social causes of aggressive behavior, such as pain or inadequate social demands.
The sedative effects of risperidone should be carefully monitored in this population because of possible effects on learning ability. Changing the timing of risperidone administration may improve control of the effects of sedation on attention in adolescents and children. Risperidone use has been associated with mean increases in body weight and BMI. Growth changes in long-term studies were within expected age norms. The effects of long-term risperidone administration on sexual development and growth have not been fully investigated.
Because of the possible effects of long-term hyperprolactinemia on growth and sexual development in children and adolescents, regular clinical evaluation of hormonal status should be performed, including measurement of growth, body weight, observation of sexual development, menstrual cycle and other possible prolactin-dependent effects.
While being treated with risperidone, the presence of extrapyramidal symptoms and other movement disorders should be checked regularly.
Associates
The drug Risset®, film-coated tablets, contains lactose. In patients with rare hereditary diseases associated with galactose intolerance, Lapp lactase deficiency or glucose-galactose malabsorption, Risset®, film-coated tablets should not be used. The 2 mg film-coated tablets contain the dye sunset yellow (E110) which may cause allergic reactions.
Influence on driving and operating machinery
The drug Risset® may have mild to moderate effect on driving and operating machinery. Patients should be advised to refrain from driving and operating machinery until their individual sensitivity to the drug is clarified.
Synopsis
Synopsis
Contraindications
Contraindications
With caution
Side effects
Side effects
The most frequently observed side effects (frequency of occurrence â¥10%) were: parkinsonism, sedation, headache, and insomnia.
The side effects of risperidone in therapeutic doses are listed with frequency and organ system distributions. The frequency of side effects was classified as follows: very frequent (â¥1/10 cases), frequent (â¥1/100 and < 1/10 cases), infrequent (â¥1/1000 and < 1/100 cases), rare (â¥1/10000 and < 1/1000 cases), very rare (< 1/10000 cases) and with unknown frequency (frequency cannot be estimated from available data).
In each frequency group, side effects are presented in decreasing order of importance.
Cardiovascular side:often, tachycardia; infrequently, atrial fibrillation, atrioventricular block, conduction disturbances, prolonged QT interval, bradycardia, abnormal electrocardiographic readings, palpitations; rarely, sinus arrhythmia.
Hematological disorders and disorders of the lymphatic system: infrequent – neutropenia, decreased leukocyte count, thrombocytopenia, anemia, decreased hematocrit, decreased eosinophil count; rare – agranulocytosis3.
Nervous system disorders: very frequently, sedation, somnolence, parkinsonism4, headache; frequently, akathisia4, dystonia4, dizziness, dyskinesia4, tremor; infrequent – tardive dyskinesia, cerebral ischemia, lack of response to stimulation, loss of consciousness, decreased level of consciousness, seizures4, syncope, psychomotor hyperactivity, balance disorder, coordination disorder, postural vertigo, attention disorder, dysarthria, dysgeusia, hypoesthesia, paresthesia; rarely, malignant neuroleptic syndrome, cerebrovascular disorders, diabetic coma, head tremor.
Ophthalmological disorders: frequent – blurred vision, conjunctivitis; infrequent – photophobia, dry eyes, increased lacrimation, eye hyperemia; rare – glaucoma, involuntary rotation of eyeballs, eye movement disorders, crust formation at the eyelid margin, intraoperative flabby iris syndrome3.
On the ear and labyrinth side: frequently, tinnitus, vertigo, ear pain.
Respiratory, thoracic and mediastinal disorders: frequently, dyspnea, pain in the larynx and pharynx, cough, nasal bleeding, nasal congestion; infrequently, aspiration pneumonia, pulmonary congestion, breathing disorders, wheezing, wheezing, wheezing, airway obstruction, dysphonia, respiratory distress; rarely, sleep apnea syndrome, hyperventilation.
Gastrointestinal tract:often, abdominal pain, stomach discomfort, vomiting, diarrhea, constipation, nausea, dyspepsia, dry mouth, toothache; infrequent, fecal incontinence, fecaloma, gastroenteritis, dysphagia, flatulence; rare, pancreatitis, bowel obstruction, tongue swelling, heylitis; very rare, ileus.
Kidney and urinary tract pathways: often – enuresis; infrequently – pollakiuria, urinary retention, dysuria.
Skin and subcutaneous tissue: frequently, rash, erythema; infrequently, urticaria, pruritus, alopecia, hyperkeratosis, eczema, dry skin, skin discoloration, acne, seborrheic dermatitis, skin inflammation, skin disorders; rarely, toxicoderma, dandruff; very rarely, Quincke’s edema.
Musculoskeletal and connective tissue: often – muscle cramps, skeletal muscle soreness, back pain, arthralgia; infrequent – increased blood creatine phosphokinase levels, forced posture, joint stiffness, joint swelling, muscle weakness, neck pain; rare – rhabdomyolysis.
Endocrine system: frequent hyperprolactemia1; rare – disruption of antidiuretic hormone production.
Metabolic and nutritional disorders: frequent – increased appetite, decreased appetite; infrequent – diabetes2, hyperglycemia, polydipsia, decreased body weight, anorexia, increased blood cholesterol levels; rarely – water intoxication3, hypoglycemia, hyperinsulinemia3, increased blood triglyceride levels; very rarely – diabetic ketoacidosis.
Infections:often, pneumonia, bronchitis, upper respiratory tract infections, sinusitis, urinary tract infections, ear infections, influenza; infrequently, respiratory tract infections, cystitis, onychomycosis, phlegmon, local infection, viral infections, acarodermatitis; rarely, infection.
vascular disorders: often – arterial hypertension; infrequently – hypotension, orthostatic hypotension, hot flashes; rarely – pulmonary embolism, deep vein thrombosis.
General disorders and phenomena due to the use of the drug: often – edema4, fever, asthenia, pain; infrequently – facial edema, elevated body temperature, gait disturbance, malaise, thirst, chest discomfort, chills, malaise, discomfort; rarely – hypothermia, cold extremities, decreased body temperature, “withdrawal” syndrome, thickening of organs and tissues3.
In immune system: infrequently – hypersensitivity; rarely – anaphylactic reaction3.
Hepatobiliary disorders: infrequent – increased transaminase activity, increased gamma-glutamyltransferase activity, increased liver enzyme activity; rarely – jaundice.
Reproductive system and mammary glands: infrequent – erectile dysfunction, impaired ejaculation, amenorrhea, menstrual cycle disorders4, gynecomastia, galactorrhea, sexual dysfunction, breast pain, discomfort in the breast, vaginal discharge; Rarely, priapism3, delayed menstrual cycle, inability to ejaculate, breast engorgement, breast enlargement, mammary gland discharge.
Pregnancy, postpartum and neonatal periods: rarely, “withdrawal” syndrome in newborns3.
Psychiatric disorders: very common – insomnia4; common – sleep disturbances, agitation, depression, anxiety; infrequent – mania, confusion, decreased libido, nervousness, nightmares; rare – flattening of affect, anorgasmia, catatonia, somnambulism; very rare – sleep-related eating disorder.
Overdose
Overdose
Symptoms. In general, the observed symptoms of overdose were the already known pharmacological effects of risperidone in an enhanced form: drowsiness, sedation, tachycardia, arterial hypotension, extrapyramidal symptoms. QT interval prolongation and seizures have been observed. Bidirectional ventricular tachycardia has been observed when a higher dose of risperidone and paroxetine are taken together.
In cases of acute overdose, the possibility of overdose from taking more than one drug should be considered.
Treatment. Free airway patency should be achieved and maintained to ensure adequate oxygen supply and ventilation. Gastric lavage (after intubation if unconscious) and administration of activated charcoal, along with a laxative, should be done only if the drug was taken no more than one hour ago. ECG monitoring should be started immediately to detect possible arrhythmias.
There is no specific antidote, appropriate symptomatic therapy should be given. Arterial hypotension and vascular collapse should be treated with intravenous fluid infusions and/or sympathomimetic drugs. If severe extrapyramidal symptoms develop, anticholinergic drugs should be prescribed. Continuous medical observation and monitoring should be continued until symptoms of intoxication disappear.
Pregnancy use
Pregnancy use
Pregnancy. Relevant data on the use of risperidone during pregnancy are not available. Animal studies have not shown teratogenic effects of risperidone, but other types of toxic effects on reproduction have been observed. The potential risk to humans is unknown.
Newborns exposed to antipsychotic drugs (including risperidone) during the third trimester of pregnancy are at risk for adverse reactions, including extrapyramidal symptoms and/or withdrawal symptoms, which may vary in severity and duration after delivery. There have been reports of agitation, decreased or increased muscle tone, tremor, somnolence, impaired respiratory function, or difficulty in feeding. Therefore, newborns should be closely monitored.
The drug Risset® must not be used during pregnancy unless clearly necessary. If it is necessary to discontinue the drug during pregnancy, the drug should be withdrawn gradually.
The period of breastfeeding. In animal studies, risperidone and 9-hydroxyrisperidone have penetrated into breast milk. In addition, risperidone and 9-hydroxyrisperidone have been shown to penetrate into breast milk in humans in small amounts. There are no data on adverse reactions in breastfed infants. Therefore, breastfeeding should be considered in light of the possible risk to the baby.
Fertility. Like other D2-dopamine receptor antagonist drugs, Risset® contributes to increased prolactin levels. Hyperprolactinemia contributes to inhibition of gonadotopin-releasing hormone of hypothalamus, which leads to decrease of gonadotopin secretion by pituitary. This, in turn, contributes to the suppression of reproductive function as a result of impaired gonadal steroid synthesis in women and men.
Similarities
Similarities
Additional information
| Weight | 0.012 kg |
|---|---|
| Shelf life | 30 months. Do not use after the expiration date. |
| Conditions of storage | Store at a temperature not exceeding 25 ° C. Keep out of reach of children! |
| Manufacturer | Pliva Hrvatska d.o.o., Croatia |
| Medication form | pills |
| Brand | Pliva Hrvatska d.o.o. |
Related products
Buy Risset, 4 mg 20 pcs. with delivery to USA, UK, Europe and over 120 other countries.