No products in the cart.
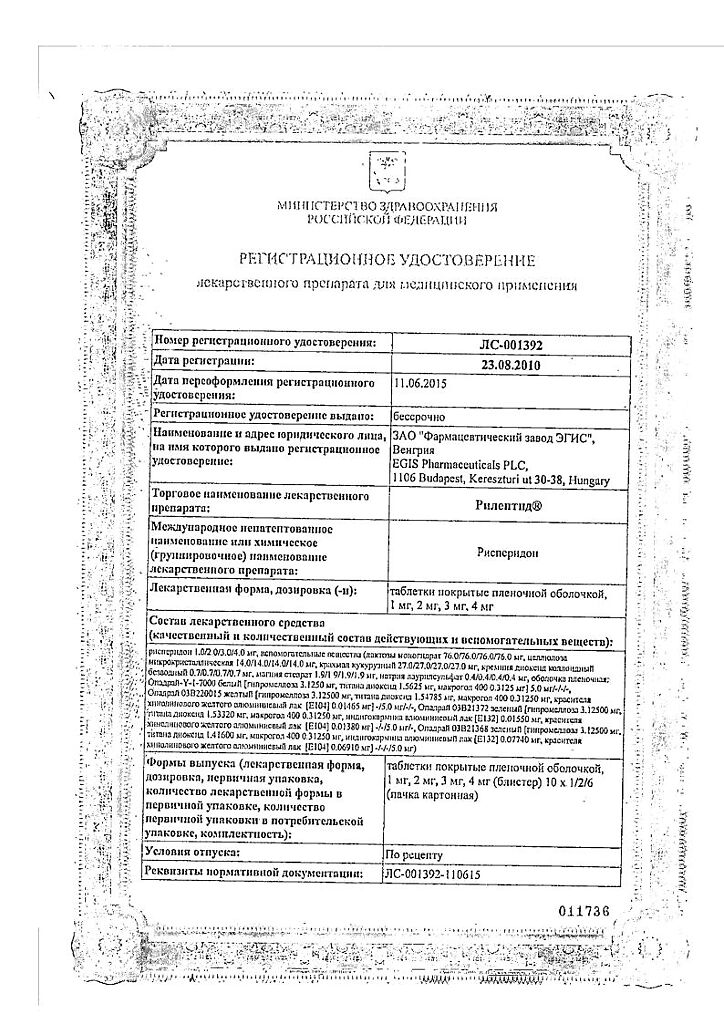
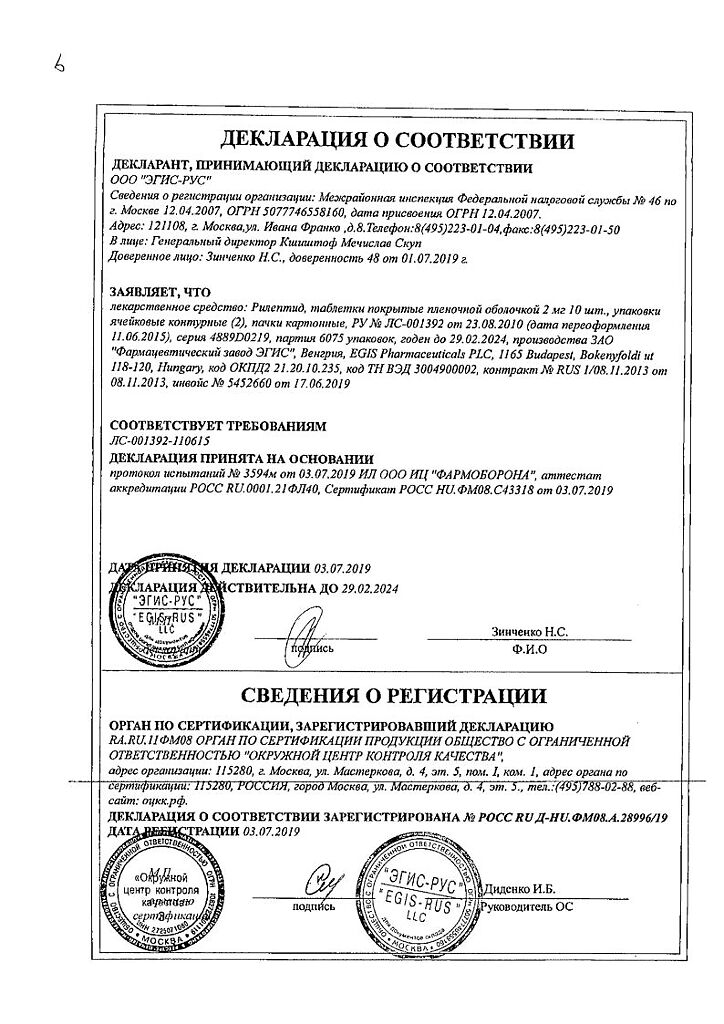
Rileptide, 2 mg 20 pcs.
€1.00
Out of stock
(E-mail when Stock is available)
Description
Rileptide is an antipsychotic.
Pharmacodynamics
Risperidone is an antipsychotic and also has sedative, antiemetic and hypothermic effects. Risperidone is a monoaminergic antagonist with marked affinity for serotonergic 5-NT2– and dopaminergic D2-receptors, also binds to α1-adrenoceptors and, with slightly lower affinity, to H1-histaminergic and α2-adrenergic receptors. It has no tropism to cholinoreceptors.
The antipsychotic action is caused by blockade of dopamine D2 receptors of mesolimbic and mesocortical system.
Sedative action is caused by blockade of adrenoreceptors of reticular formation of brain stem; antiemetic action – by blockade of dopamine D2-receptors of trigger zone of vomiting center; hypothermic action – by blockade of dopamine receptors of hypothalamus.
Reduces productive symptomatology (delirium, hallucinations), automatism. Causes less suppression of motor activity and induces catalepsy to a lesser extent than classical antipsychotics (neuroleptics).
The balanced central antagonism to serotonin and dopamine may reduce the risk of extrapyramidal symptomatology.
Risperidone may cause a dose-dependent increase in plasma prolactin concentrations.
Pharmacokinetics
In oral administration, risperidone is completely absorbed (regardless of ingestion) and Cmax in plasma is observed after 1 -2 h. Risperidone is metabolized with the cytochrome P450 isoenzyme CYP2D6 to form 9-hydroxysperidone, which has similar pharmacological effects. Risperidone and 9-hydroxyrisperidone constitute an effective antipsychotic fraction. Further metabolism of risperidone consists of N-dealkylation. When ingested, risperidone is excreted with a T1/2 of approximately 3 h. The T1/2 of 9-hydroxysperidone and the active antipsychotic fraction has been found to be 24 h.
In most patients the equilibrium concentration of risperidone is observed one day after the start of treatment. The equilibrium state of 9-hydroxirisperidone in most cases is reached 3-4 days after the start of treatment.
The concentration of risperidone in plasma is proportional to the dose of the drug (within therapeutic doses).
Risperidone is rapidly distributed in the body. The volume of distribution is 1-2 l/kg. In plasma risperidone is bound to albumin and acidic α1-glycoprotein. The fraction of risperidone and 9-hydroxysperidone bound to plasma proteins is 88% and 77%, respectively.
Extracted by the kidneys – 70% (of which 35-45% as pharmacologically active fraction) and 14% in the bile. In single administration high levels of active plasma concentrations and slow excretion in elderly patients and patients with insufficient renal function are noted.
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
Active ingredient:
Risperidone;
Associates:
Lactose monohydrate;
MCC;
Corn starch;
Anhydrous colloidal silica;
Magnesium stearate;
sodium lauryl sulfate
How to take, the dosage
How to take, the dosage
Schizophrenia
Adults and children over 15 years of age. Rileptide® may be administered 1 or 2 times daily. The initial dose is 2 mg/day. On the second day, the dose should be increased to 4 mg/day. From then on, the dose can either be maintained at the same level or individually adjusted if necessary. Usually the optimal dose is 4-6 mg/day. In some cases, a slower dose increase and lower starting and maintenance doses may be warranted.
Doses above 10 mg/day have not been shown to be more effective than lower doses and may cause extrapyramidal symptoms. Because the safety of doses above 16 mg/day has not been studied, doses above this level should not be used.
There is no information on use for the treatment of schizophrenia in children younger than 15 years of age.
Elderly patients. A starting dose of 0.5 mg per administration 2 times daily is recommended. The dosage can be individually increased from 0.5 mg 2 times a day to 1-2 mg 2 times a day.
Hepatic and renal diseases. An initial dose of 0.5 mg per dose 2 times daily is recommended. This dose can be gradually increased to 1-2 mg per dose 2 times a day.
Medication abuse or drug dependence. The recommended daily dose of the drug is 2-4 mg.
Behavioral disorders in patients with dementia
The recommended starting dose is 0.25 mg per dose 2 times daily. The dosage can be increased individually at 0.25 mg 2 times a day if necessary, no more often than every other day. For most patients, the optimal dose is 0.5 mg 2 times a day. However, some patients can take 1 mg twice a day.
Interaction
Interaction
Given that risperidone primarily affects the CNS, it should be used with caution in combination with other centrally acting drugs and with alcohol.
Risperidone decreases the effectiveness of levodopa and other dopamine agonists.
Clozapine decreases the clearance of risperidone.
Carbamazepine has been observed to decrease the plasma concentration of the active antipsychotic fraction of risperidone. Similar effects may be observed with other hepatic enzyme inducers.
Phenothiazines, tricyclic antidepressants and some beta-adrenoblockers may increase the plasma concentration of risperidone, but this does not affect the concentration of the active antipsychotic fraction.
Fluoxetine may increase the plasma concentration of risperidone, but less so the concentration of the active antipsychotic fraction, so doses of risperidone should be adjusted.
When using risperidone together with other drugs that are highly bound to plasma proteins, clinically pronounced displacement of any drug from the plasma protein fraction is not observed.
Hypotensive drugs increase the severity of BP reduction with risperidone.
Special Instructions
Special Instructions
Transition from therapy with other antipsychotic drugs. In schizophrenia, at the beginning of treatment with risperidone, it is recommended that previous therapy be gradually withdrawn if clinically justified. If patients are being transferred from depot-form antipsychotic therapy, it is recommended that risperidone be started instead of the next scheduled injection. The need for continuation of antiparkinsonian drug therapy should be evaluated periodically.
Due to the α-adrenoblocking effect of Risperidone® orthostatic hypotension may occur, especially during initial dose adjustment. If hypotension occurs, dose reduction should be considered. In patients with cardiovascular disease, as well as in dehydration, hypovolemia or cerebrovascular disorders, the dose should be increased gradually, according to the recommendations (see “Dosage and administration”).
The occurrence of extrapyramidal symptoms is a risk factor for the development of tardive dyskinesia. If signs and symptoms of tardive dyskinesia occur, withdrawal of all antipsychotic medications should be considered. If neuroleptic malignant syndrome occurs, characterized by hyperthermia, muscle rigidity, instability of autonomic functions, impaired consciousness and elevated creatine phosphokinase levels, all antipsychotic drugs, including risperidone, should be withdrawn.
Patients with schizophrenia have an increased risk of suicide attempts, so treatment of patients at increased risk of suicide should be closely monitored.
The dose of risperidone should be reduced when carbamazepine and other hepatic enzyme inducers are withdrawn.
Patients should be advised to refrain from overeating due to the possibility of weight gain.
During treatment it is necessary to refrain from engaging in potentially hazardous activities requiring increased concentration and rapid psychomotor reactions, and from drinking alcohol.
Contraindications
Contraindications
With caution: cardiovascular diseases (chronic cardiac insufficiency, myocardial infarction, cardiac conduction disorders); dehydration and hypovolemia; cerebral circulation disorders; Parkinson’s disease; seizures (incl.severe renal or hepatic impairment (see dosing guidelines); drug abuse or dependence (see dosing guidelines)
Dosage recommendations; conditions predisposing to development of pirouette tachycardia (bradycardia, electrolyte imbalance, concomitant use of QT prolonging drugs); brain tumor, intestinal obstruction, cases of acute drug overdose, Reye syndrome (antiemetic effect of risperidone may mask symptoms of these conditions); pregnancy, childhood under 15 years (effectiveness and safety not established).
Side effects
Side effects
Nervous system disorders: Insomnia, agitation, anxiety, headache; sometimes – drowsiness, increased fatigue, dizziness, impaired concentration, blurred vision; rarely – extrapyramidal symptoms (tremor, rigidity, hypersalivation, bradykinesia, akathisia, acute dystonia), mania or hypomania, stroke (in elderly patients with predisposing factors), and hypervolemia (either due to polydipsia or inadequate ADH secretion syndrome) tardive dyskinesia (involuntary rhythmic movements primarily of the tongue and/or face), neuroleptic malignant syndrome (hyperthermia, muscle rigidity, instability of autonomic functions, impaired consciousness and increased creatine phosphokinase levels), thermoregulatory disorders and epileptic seizures.
Digestive system disorders: constipation, dyspepsia, nausea or vomiting, abdominal pain, increased liver transaminase activity, dry mouth, hypo- or hypersalivation, anorexia and/or increased appetite, weight gain or loss.
Systemic diseases: sometimes – orthostatic hypotension, reflex tachycardia or hypertension.
Hematopoietic disorders: neutropenia, thrombocytopenia.
Endocrine system disorders: galactorrhea, gynecomastia, menstrual cycle disorders, amenorrhea, weight gain, hyperglycemia and exacerbation of pre-existing diabetes.
Urogenital system disorders: priapism, erectile dysfunction, ejaculation disorders, anorgasmia, urinary incontinence.
Allergic reactions: rhinitis, rash, angioedema, photosensitization.
Skin disorders: dry skin, hyperpigmentation, itching, seborrhea.
Others: arthralgia.
Overdose
Overdose
Symptoms: somnolence, sedation, depression of consciousness, tachycardia, arterial hypotension, extrapyramidal disorders, in rare cases – QT interval prolongation.
Treatment: it is necessary to provide free airway patency to ensure adequate oxygenation and ventilation, gastric lavage (after intubation if the patient is unconscious) and administration of activated charcoal in combination with laxatives. Symptomatic therapy aimed at maintenance of vital body functions.
In order to diagnose possible cardiac rhythm disturbances in time, ECG monitoring should be started as soon as possible. Close medical observation and ECG monitoring is carried out until symptoms of intoxication have completely disappeared. There is no specific antidote.
Similarities
Similarities
Additional information
| Shelf life | 5 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C |
| Manufacturer | EGIS, Hungary |
| Medication form | pills |
| Brand | EGIS |
Related products
Buy Rileptide, 2 mg 20 pcs. with delivery to USA, UK, Europe and over 120 other countries.