No products in the cart.
Rexetine, 20 mg 30 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Rexetine has antidepressant effects.
Pharmacodynamics
Inhibits in the central nervous system neuronal reuptake of serotonin. Has little effect on the neuronal takeover of norepinephrine and dopamine. It also has anxiolytic and psychostimulant properties.
Pharmacokinetics
Paroxetine is well absorbed after oral administration. It is metabolized mainly in the liver, with the formation of mostly inactive metabolites. Simultaneous intake of food does not affect the absorption and pharmacokinetics of paroxetine. Paroxetine binds 93-95% to plasma proteins.
The half-life of paroxetine ranges from 6 to 71 hours, but averages one day.
Dynamic equilibrium in blood plasma is reached 7-14 days after initiation of therapy; thereafter, pharmacokinetics does not change during long-term therapy. Approximately 64% of paroxetine is excreted in the urine (2% unchanged, 62% as metabolites); about 36% is excreted through the gastrointestinal tract mainly as metabolites, less than 1% is excreted unchanged in the feces.
Plasma concentrations of paroxetine increase with hepatic and renal dysfunction, as well as in old age.
Indications
Indications
Depression of various etiologies, incl. states accompanied by anxiety;
Obsessive-compulsive disorder (compulsive disorder);
Panic disorders, including fear of being in a crowd (agoraphobia);
Social phobias;
Generalized anxiety disorder (GAD);
Post-traumatic stress disorders.
It is also used as part of anti-relapse treatment.
Pharmacological effect
Pharmacological effect
Rexetine has an antidepressant effect.
Pharmacodynamics
Inhibits the reverse neuronal uptake of serotonin in the central nervous system. Has little effect on the neuronal uptake of norepinephrine and dopamine. It also has anxiolytic and psychostimulant properties.
Pharmacokinetics
After oral administration, paroxetine is well absorbed. Metabolized mainly in the liver, with the formation of mainly inactive metabolites. Concomitant food intake does not affect the absorption and pharmacokinetics of paroxetine. Paroxetine binds to plasma proteins by 93-95%.
The half-life of paroxetine ranges from 6 to 71 hours, but averages one day.
Dynamic equilibrium in the blood plasma is achieved 7-14 days after the start of therapy; subsequently, the pharmacokinetics do not change with long-term therapy. Approximately 64% of paroxetine is excreted in the urine (2% unchanged, 62% as metabolites); approximately 36% is excreted through the gastrointestinal tract mainly in the form of metabolites, less than 1% is excreted unchanged in the feces.
The concentration of paroxetine in the blood plasma increases with impaired liver and kidney function, as well as in old age.
Special instructions
Special instructions
Taking paroxetine simultaneously with MAO inhibitors and within 14 days after their discontinuation is contraindicated. In the future, paroxetine should be used with extreme caution, starting treatment with small doses and gradually increasing the dosage until the desired therapeutic effect is achieved. After completing paroxetine therapy, treatment with MAO inhibitors should not be started for 14 days.
If the patient has previously been in a manic state, the possibility of relapse should be considered while taking paroxetine (as with other antidepressants).
There is insufficient experience with the simultaneous use of electroconvulsive therapy and paroxetine.
Due to the predisposition to suicide attempts in patients with depression and patients with drug addiction during the abstinence period, this category of patients requires careful monitoring during the treatment process.
Hyponatremia has been reported in many cases, especially in elderly patients receiving diuretics. After stopping paroxetine, blood sodium levels return to normal.
In some cases, increased bleeding (mainly ecchymosis and purpura) occurred during treatment with paroxetine.
Hyperglycemic conditions have rarely been reported with the use of paroxetine.
Suicide/Suicidal ideation
Depression is associated with an increased risk of suicidal ideation, self-injury, and suicide. This risk persists until remission occurs. Because improvement may not occur within the first few weeks or more of treatment, patients should be closely monitored until such improvement occurs. Current clinical experience suggests that during treatment with antidepressants, the risk of suicide may increase in the early stages of recovery.
Other psychiatric conditions for which Rexetine is prescribed may also be associated with an increased risk of suicidal behavior. In addition, these conditions may be comorbid with major depressive disorder. The same precautions that are taken when treating patients with major depressive disorder should be observed when it comes to treating patients with other psychiatric disorders. Patients with a history of suicidal behavior or thoughts, or who demonstrate a significant degree of suicidal ideation before treatment, are at greater risk for suicidal ideation or suicide attempts and should be closely monitored during treatment. There is an increased risk of suicide in such patients aged 18-29 years, so treatment with the drug should be carefully monitored.
Patients (and those who provide care to patients) should be prepared for the need to monitor in emergency situations – the emergence of suicidal intentions/behavior or thoughts of self-aggression, in order to seek medical help immediately if these symptoms are present.
Impact on the ability to drive vehicles and operate machinery
Controlled studies have not revealed a negative effect of paroxetine on psychomotor or cognitive function. Despite this, at the beginning of the course of therapy, for an individually determined period, you should not drive a car or work in high-risk conditions that require quick reactions. The degree of restriction is determined individually.
Active ingredient
Active ingredient
Paroxetine
Composition
Composition
1 film-coated tablet contains:
Active ingredient:
paroxetine hydrochloride hemihydrate 22.76 mg, which corresponds to the content of paroxetine 20 mg;
Excipients:
hypromellose – 15 mg;
calcium hydrogen phosphate dihydrate – 244.24 mg;
sodium carboxymethyl starch – 15 mg;
magnesium stearate – 3 mg
Film shell:
hypromellose – 7.2 mg;
macrogol 400 – 0.07 mg;
macrogol 6000 – 0.956 mg;
polysorbate 80 – 0.044 mg;
titanium dioxide – 1.03 mg.
Pregnancy
Pregnancy
The safety of paroxetine during pregnancy has not been studied, so it should not be used during pregnancy and lactation, unless from a medical point of view, the potential benefits of treatment outweigh the possible risks associated with taking the drug.
If it is necessary to use the drug during lactation, the issue of stopping breastfeeding should be decided.
During the period of use of the drug, women of childbearing age should avoid conception (use reliable methods of contraception).
Contraindications
Contraindications
History of hypersensitivity to the components of the drug.
Therapy with monoamine oxidase inhibitors (MAOIs) and the period after stopping treatment with MAO inhibitors for two weeks.
Pregnancy and lactation period. The safety of paroxetine during pregnancy has not been studied, so it should not be used during pregnancy and lactation, unless from a medical point of view, the potential benefits of treatment outweigh the possible risks associated with taking the drug.
Children under 18 years of age (due to lack of clinical experience).
Side Effects
Side Effects
From the gastrointestinal tract, liver: Nausea (12%); sometimes constipation, diarrhea, loss of appetite. Rarely increased liver function tests; sometimes severe liver dysfunction. A cause-and-effect relationship has not been proven between taking paroxetine and changes in liver enzyme activity, but discontinuation of paroxetine is recommended in case of liver dysfunction.
From the side of the central nervous system: Drowsiness (9%); tremor (8%); general weakness and increased fatigue (7%); insomnia (6%); in some cases, headache, increased irritability, paresthesia, dizziness, somnambulism. Extrapyramidal disorders and orofacial dystonia were rarely observed. Extrapyramidal disorders are observed mainly with previous intensive use of antipsychotics. Epileptiform seizures were rarely observed, which is also typical for therapy with other antidepressants; increased intracranial pressure.
From the autonomic nervous system: Increased sweating (9%), dry mouth (7%).
From the senses: In some cases, visual impairment and mydriasis were noted; rarely – an attack of acute glaucoma.
From the cardiovascular system: In some cases, tachycardia, ECG changes, lability of blood pressure, and fainting conditions have been described.
From the genital area and urinary system: Ejaculation disorder (13%), in some cases, changes in libido, rarely difficulty urinating.
Electrolyte imbalance: In some cases, hyponatremia with the development of peripheral edema, impaired consciousness or epileptiform symptoms has been noted. After discontinuation of the drug, the sodium level in the blood normalizes. In some cases, this condition developed due to overproduction of antidiuretic hormone. Most of these cases were observed in elderly patients who, in addition to paroxetine, received diuretics and other medications.
Dermatological reactions and hypersensitivity reactions: In rare cases, skin hyperemia, subcutaneous hemorrhages, swelling in the face and extremities, anaphylactic reactions (urticaria, bronchospasm, angioedema), and skin itching have been described.
Others: In isolated cases, myopathies, myalgia, hyperglycemia, rarely hyperprolactinemia, galactorrhea, hypoglycemia, fever and the development of a flu-like condition were noted. Thrombocytopenia rarely develops, but a cause-and-effect relationship with the drug has not been proven. Taking paroxetine may be accompanied by an increase or decrease in body weight. A few cases of increased bleeding have been reported (See Warnings). Paroxetine, compared with tricyclic antidepressants, is less likely to cause dry mouth, constipation and drowsiness. Sudden discontinuation of the drug can cause dizziness, sensory disturbances (for example, paresthesia), fear, sleep disturbance, agitation, tremor, nausea, increased sweating and confusion, so discontinuation of drug therapy should be done gradually, it is advisable to reduce the dosage every second day.
Interaction
Interaction
Food and antacids do not affect the absorption and pharmacokinetics of paroxetine.
Like other serotonin reuptake inhibitors, undesirable interactions between MAO inhibitors and paroxetine have been observed in animal studies.
The simultaneous use of paroxetine with tryptophan leads to headache, nausea, increased sweating and dizziness, so this combination should be avoided.
A pharmacodynamic interaction is expected between paroxetine and warfarin (increased bleeding was noted with unchanged prothrombin time); the use of such a combination requires caution.
When paroxetine is used together with sumatriptan, general weakness, hyperreflexia, and coordination problems are observed. If their simultaneous use is necessary, extreme caution should be exercised (medical supervision is required).
When used concomitantly, paroxetine may inhibit the metabolism of tricyclic antidepressants (due to inhibition of the CYP2D6 isoenzyme), so the use of this combination requires caution and a reduction in the dose of tricyclic antidepressants.
Drugs that enhance or inhibit the activity of liver enzyme systems may affect the metabolism and pharmacokinetics of paroxetine. When used concomitantly with inhibitors of metabolic liver enzymes, the lowest effective dose of paroxetine should be used. Combined use with liver enzyme inducers does not require adjustment of the initial dose of paroxetine; further changes in dosage depend on the clinical effect (efficacy and tolerability).
Paroxetine significantly inhibits the activity of the CYP2D6 isoenzyme. Therefore, special caution requires the simultaneous use of paroxetine with drugs whose metabolism occurs with the participation of this isoenzyme, incl. with certain antidepressants (for example, nortriptyline, amitriptyline, imipramine, desipramine and fluoxetine), phenothiazines (for example, thioridazine), class 1 C antiarrhythmic drugs (for example, propafenone, flecainide and encainide) or with those drugs that block its action (for example, quinidine, cimetidine, codeine).
There are no reliable clinical data on the inhibition of the CYP3A4 isoenzyme by paroxetine, so use with drugs that inhibit this enzyme (for example, terfenadine) is possible.
Cimetidine inhibits some cytochrome P450 isoenzymes. As a result, the combined use of paroxetine with cimetidine increases the level of paroxetine in the blood plasma at the steady-state stage.
Phenobarbital increases the activity of some cytochrome P450 isoenzymes. When paroxetine is used together with phenobarbital, the concentration of paroxetine in the blood plasma decreases and its T1/2 is also shortened.
When paroxetine and phenytoin are used together, the concentration of paroxetine in the blood plasma decreases and the frequency of side effects of phenytoin may increase. When using other anticonvulsants, the incidence of their side effects may also increase. In patients with epilepsy treated for a long time with carbamazepine, phenytoin or sodium valproate, additional administration of paroxetine did not cause changes in the pharmacokinetic and pharmacodynamic properties of anticonvulsants; There was no increase in paroxysmal convulsive readiness.
Paroxetine is highly bound to plasma proteins. When used simultaneously with drugs that also bind to plasma proteins, side effects may increase due to an increase in the concentration of paroxetine in the blood plasma.
Due to the lack of sufficient clinical experience with the combined use of digoxin and paroxetine, the use of this combination requires caution.
Diazepam during a course of use does not affect the pharmacokinetics of paroxetine.
Paroxetine significantly increases the concentration of procyclidine in the blood plasma, therefore, if anticholinergic side effects occur, it is necessary to reduce the dose of procyclidine.
In clinical trials, paroxetine had no effect on propranolol blood levels.
In some cases, an increase in the concentration of theophylline in the blood was noted. Although the interaction between paroxetine and theophylline has not been proven in clinical studies, regular monitoring of theophylline blood levels is recommended.
An increase in the effect of ethanol when used simultaneously with paroxetine was not detected. However, due to the effect of paroxetine on the liver enzyme system, it is necessary to avoid drinking alcohol during treatment with paroxetine.
Overdose
Overdose
Symptoms: nausea, vomiting, tremor, dilated pupils, dry mouth, general agitation, increased sweating, drowsiness, dizziness, flushing of the facial skin. No coma or convulsions were observed. Fatal outcome has been reported rarely, usually with a simultaneous overdose of paroxetine and another drug that causes adverse interactions. Signs of overdose appear when 2 g of paroxetine is used simultaneously or when a large dose of paroxetine is taken with other drugs or with alcohol. Paroxetine therapy is safe over a wide range of doses.
Treatment: gastric lavage, 20-30 g of activated carbon every 4-6 hours for the first 24-48 hours; The airways should be cleared and oxygenation administered if necessary. Carry out monitoring of the vital functions of the body and general measures aimed at maintaining them. There is no specific antidote. Forced diuresis, hemodialysis or hemoperfusion are ineffective if a large dose of paroxetine has entered the tissues from the blood.
Storage conditions
Storage conditions
At 15–30 °C
Shelf life
Shelf life
5 years
Manufacturer
Manufacturer
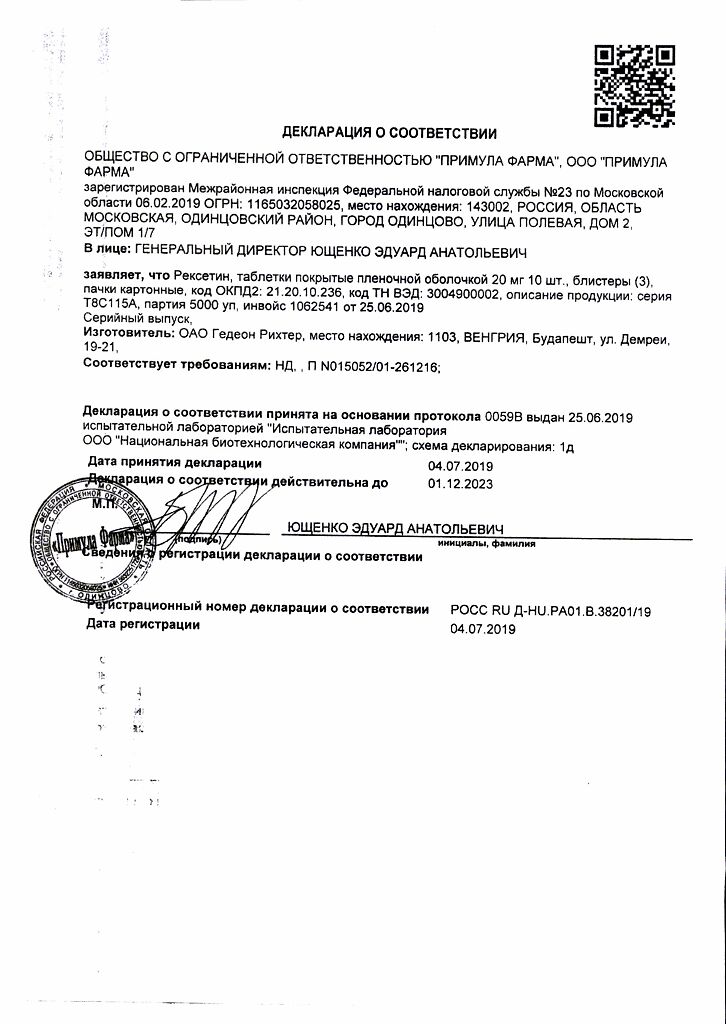
Gedeon Richter, Hungary
Additional information
| Shelf life | 5 years |
|---|---|
| Conditions of storage | At 15-30 °C |
| Manufacturer | Gedeon Richter, Hungary |
| Medication form | pills |
| Brand | Gedeon Richter |
Related products
Buy Rexetine, 20 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.