No products in the cart.
Description
Pharmacotherapeutic group: Antiviral [HIV] medicine.
ATX code:
J05AG Nenucleosides – reverse transcriptase inhibitors
J05AG03 Efavirenz
Pharmacological properties
/p>
Pharmacodynamics
Efavirenz is a non-nucleoside reverse transcriptase inhibitor (NNRTI) of HIV-1. Efavirenz is a non-competitive HIV-1 reverse transcriptase inhibitor and does not significantly inhibit HIV-2 reverse transcriptase or human cellular DNA polymerases (alpha, beta, gamma and delta).
HIV sensitivity in vitro. The clinical significance of HIV-1 sensitivity to efavirenz in vitro has not been established. The in vitro antiviral efficacy of efavirenz was evaluated on lymphoblast cell lines, peripheral blood mononuclear cells and macrophage/monocyte cultures. The concentration of efavirenz required for 90 to 95% inhibition (IC90-95) of laboratory-adapted wild-type strains and zidovudine-resistant clinical isolates ranged from 0.46 to 6.8 nmol/L.
Efavirenz showed synergistic activity in cell culture in combination with the nucleoside reverse transcriptase inhibitors (NRTIs) zidovudine and didanosine and the protease inhibitor indinavir.
Resistance. The antiviral efficacy of efavirenz in cell culture against virus strains with amino acid substitutions in the reverse transcriptase at positions 48, 108, 179, 181 or 236, as well as against strains with amino acid substitutions in the protease, was similar to that of wild-type virus strains. The only substitutions that resulted in the highest resistance to efavirenz in cell culture were the substitution of leucine for isoleucine at position 100 (L100I, 17-22-fold resistance) and lysine for asparagine at position 103 (K103N, 18-33-fold resistance). A more than 100-fold decrease in viral susceptibility to the drug was observed for HIV varieties expressing the K103N substitution in addition to other amino acid substitutions in the reverse transcriptase.
K103N is the most commonly observed substitution in reverse transcriptase in viral isolates obtained from patients who had a significant increase in viral particles after treatment withdrawal in clinical trials of efavirenz in combination with indinavir or in the combination of zidovudine with lamivudine. Substitutions in reverse transcriptase at positions 98, 100, 101, 101, 108, 138, 188, 190, and 225 were also observed, but less frequently and often only in combination with K103N. The type of amino acid substitutions in the reverse transcriptase associated with efavirenz resistance was independent of the other antiviral drugs used in combination with efavirenz.
Cross-resistance. A study of the cross-resistance profiles of efavirenz, nevirapine and delavirdine on cell cultures showed that K103N substitution results in loss of susceptibility to all three non-nucleoside reverse transcriptase inhibitors. Two of the three delavirdin-resistant clinical isolates studied had cross-resistance to efavirenz and contained the K103N substitution. The third isolate, which had a substitution in the reverse transcriptase at position 236, had no cross-resistance to efavirenz.
Viral isolates isolated from peripheral blood mononuclei of patients enrolled in clinical trials of efavirenz in whom therapy was ineffective (increased number of viral particles) were examined for susceptibility to NNRTIs. Thirteen isolates that had been previously characterized as resistant to efavirenz were also found to be resistant to nevirapine and delavirdine. Five of these NNRTI-resistant isolates were found to contain a K103N substitution or a valine to isoleucine substitution at position 108 (V1081) in the reverse transcriptase. Among the isolates tested after ineffective efavirenz therapy, three isolates remained sensitive to efavirenz on cell cultures and also had sensitivity to nevirapine and delavirdine.
The likelihood of cross-resistance between efavirenz and protease inhibitors is low because of the different target enzymes. Cross-resistance between efavirenz and nucleoside reverse transcriptase inhibitors is also unlikely due to different target binding sites and mechanisms of action.
Pharmacokinetics
Intake
In healthy volunteers, the maximum plasma concentration (Cmax) of efavirenz of 1.6 to 9.1 µM was reached 5 hours after a single oral administration of the drug at doses ranging from 100 mg to 1600 mg. A dose-dependent increase in maximum concentration (Smh) and area under the curve “concentration-time” was observed when taking the drug in doses up to 1600 mg; at the same time, there was no proportional relationship between the degree of increase in these indicators with the dose, suggesting that at higher doses absorption is reduced. The time to reach Plasma Cmax (3-5 hours) did not change after multiple doses of the drug, and the equilibrium plasma concentration was reached after 6-7 days.
In HIV-infected patients during the steady state period, the mean Cmax, minimum concentration (Cmin) and area under the concentration-time curve have a linear relationship with the daily dose. In 35 patients treated with efavirenz at a dose of 600 mg once daily, Cmax at equilibrium concentration was 12.9 ± 3.7 μM, Cmin was 5.6 ± 3.2 μM, and the area under the concentration-time curve was 184 ± 73 μM per hour.
The effect of food on absorption
Efavirenz can be taken regardless of meals. Taking efavirenz with food may increase its effects and lead to an increased incidence of adverse reactions. Bioavailability of a single dose of Efavirenz 600 mg in healthy volunteers increased by 22% and 17%, respectively, when taking the tablets with a meal with normal or high fat content compared to taking the same dose of the drug on an empty stomach. Efavirenz is recommended to be taken before bedtime on an empty stomach.
Distribution
Efavirenz is highly bound to plasma proteins (approximately 99.5 to 99.75%), primarily to albumin. In HIV-infected patients (N = 9) who received efavirenz in doses of 200 to 600 mg once a day for at least one month the drug concentration in cerebrospinal fluid was 0.26 to 1.19% (0.69% on average) of the corresponding concentration in blood plasma. This figure is approximately 3 times higher than the concentration of non-protein bound (free) fraction of efavirenz in blood plasma.
Metabolism
The clinical and in vitro studies using human liver microsomes have shown that efavirenz is metabolized primarily by the cytochrome P450 system to hydroxylated derivatives, which then bind to glucuronic acid to form glucuronides. These metabolites are mostly inactive against HIV-1. In vitro studies suggest that CYP3A4 and CYP2B6 are the main isoenzymes involved in the metabolism of efavirenz. In vitro studies showed that efavirenz in concentrations corresponding to those in plasma inhibits CYP2C9, CYP2C19 and CYP3A4 isoenzymes of cytochrome P450 system. In in vitro studies efavirenz did not inhibit CYP2E1 isoenzyme and inhibited CYP206 and CYP1A2 isoenzymes only in concentrations much higher than those in clinical practice.
Efavirenz has been shown to induce enzymes of the cytochrome P450 system, leading to induction of its own metabolism. When multiple doses of 200-400 mg per day for 10 days, a lower degree of cumulation of the drug was observed than expected (22-42% lower) and a shorter final elimination half-life of 40 – 55 hours (the elimination half-life of a single dose is 52 – 76 hours). The degree of induction of CYP3A4 isoenzyme is similar with efavirenz 400 mg and 600 mg doses. Pharmacokinetic interactive studies have shown that daily administration of efavirenz 400 mg or 600 mg in combination with indinavir does not cause a further decrease in the area under the concentration-time curve of indinavir compared to cases where a dose of efavirenz 200 mg was administered.
Efavirenz has a relatively long elimination half-life, ranging from 52 to 76 hours after a single dose and 40 to 55 hours after long-term use. Approximately 14% to 34% of the isotope-labeled dose of efavirenz is detected in the urine; less than 1% of the dose of efavirenz is excreted unchanged by the kidneys.
Pharmacokinetics in special patient groups
Hepatic impairment
. When efavirenz was administered once, a two-fold increase in its half-life was observed in one patient with severe hepatic impairment (Child-Pugh class C), indicating an increased degree of cumulation in these cases. Repeated administration of efavirenz showed no significant effect of liver damage on efavirenz pharmacokinetics in patients with mild hepatic impairment (Child-Pugh class A) compared to patients in the control group. There are currently insufficient data to conclude whether moderate to severe hepatic impairment (Child-Pugh class B and C) affects the pharmacokinetics of efavirenz (see Contraindications, Caution).
Renal Impairment
The pharmacokinetics of efavirenz in patients with renal impairment have not been studied, but because less than 1% of the dose of efavirenz is excreted unchanged by the kidneys, renal impairment should not significantly affect efavirenz excretion (see section “Cautionary Note”).
Gender and race
The pharmacokinetic parameters of efavirenz are similar in men and women as well as in patients of different racial backgrounds.
Age
There are no pharmacokinetic differences in patients 65 years of age or older and younger patients, although clinical studies of efavirenz have not included a sufficient number of patients 65 years of age or older.
Children
The use of efavirenz in children under 3 years of age and patients weighing less than 13 kg has not been studied. Pharmacokinetic parameters of efavirenz in children and adults were similar. In 49 children who received a dose of efavirenz equivalent to 600 mg (dose was calculated based on body weight), Cmax was 14.2 μM, Cmin was 5.6 μM and the area under the concentration-time curve was 218 μM per hour.
Indications
Indications
As part of combination antiviral therapy for the treatment of adults, adolescents and children over 3 years of age infected with the human immunodeficiency virus (HIV-1).
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: Antiviral [HIV] agent.
ATX code:
J05AG Nonnucleosides – reverse transcriptase inhibitors
J05AG03 Efavirenz
Pharmacological properties
Pharmacodynamics
Efavirenz is a non-nucleoside reverse transcriptase inhibitor (NNRTI) of HIV-1. Efavirenz is a non-competitive inhibitor of HIV-1 reverse transcriptase and does not significantly inhibit HIV-2 reverse transcriptase and human cellular DNA polymerases (alpha, beta, gamma and delta).
HIV sensitivity in vitro. The clinical significance of HIV-1 sensitivity to efavirenz in vitro has not been established. The in vitro antiviral efficacy of efavirenz was assessed in lymphoblastic cell lines, peripheral blood mononuclear cells and macrophage/monocyte cultures. The concentration of efavirenz required for 90 to 95% inhibition (IC90-95) of laboratory-adapted wild-type strains and zidovudine-resistant clinical isolates ranges from 0.46 to 6.8 nmol/L.
Efavirenz demonstrated synergistic activity in cell culture in combination with the nucleoside reverse transcriptase inhibitors (NRTIs) zidovudine and didanosine and the protease inhibitor indinavir.
Sustainability. The antiviral efficacy of efavirenz in cell culture against viral variants with amino acid substitutions in the reverse transcriptase at positions 48, 108, 179, 181, or 236, as well as against variants with amino acid substitutions in the protease, was similar to that of wild-type viral strains. The only substitutions that resulted in the highest resistance to efavirenz in cell culture were the substitution of leucine for isoleucine at position 100 (L100I, 17-22-fold resistance) and lysine for asparagine at position 103 (K103N, 18-33-fold resistance). A more than 100-fold reduction in viral susceptibility to the drug was observed for HIV variants expressing the K103N substitution in addition to other amino acid substitutions in the reverse transcriptase.
K103N is the most commonly observed reverse transcriptase substitution in viral isolates obtained from patients who experienced a significant increase in viral particle counts after treatment discontinuation in clinical trials of efavirenz plus indinavir or zidovudine plus lamivudine. Reverse transcriptase substitutions at positions 98, 100, 101, 108, 138, 188, 190 and 225 have also been observed, but less frequently and often only in combination with K103N. The type of amino acid substitutions in reverse transcriptase associated with resistance to efavirenz was independent of other antiviral drugs used in combination with efavirenz.
Cross resistance. A study of the cross-resistance profiles of efavirenz, nevirapine and delavirdine in cell cultures showed that the K103N substitution leads to loss of susceptibility to all three non-nucleoside reverse transcriptase inhibitors. Two of the three delavirdine-resistant clinical isolates tested were cross-resistant to efavirenz and contained the K103N substitution. The third isolate, which had a substitution in reverse transcriptase at position 236, was not cross-resistant to efavirenz.
Viral isolates isolated from peripheral blood mononuclear cells of patients enrolled in clinical trials of efavirenz in whom therapy had failed (increased numbers of viral particles) were tested for susceptibility to NNRTIs. Thirteen isolates that were previously characterized as resistant to efavirenz were also resistant to nevirapine and delavirdine. Five of these NNRTI-resistant isolates were found to contain a K103N substitution or a valine to isoleucine substitution at position 108 (V1081) in the reverse transcriptase. Among the isolates tested after failure of efavirenz therapy, three isolates remained sensitive to efavirenz in cell culture and were also sensitive to nevirapine and delavirdine.
The likelihood of cross-resistance between efavirenz and protease inhibitors is low due to the presence of different target enzymes. Cross-resistance between efavirenz and nucleoside reverse transcriptase inhibitors is also unlikely due to different target binding sites and different mechanisms of action.
Pharmacokinetics
Suction
In healthy volunteers, the maximum concentration (Cmax) of efavirenz in blood plasma of 1.6 – 9.1 μM was achieved 5 hours after a single oral dose of the drug in doses from 100 mg to 1600 mg. A dose-dependent increase in maximum concentration (Cmax) and area under the concentration-time curve was observed when taking the drug in doses up to 1600 mg; however, the proportional dependence of the degree of increase in these indicators on the dose was not achieved, from which it can be assumed that at higher doses absorption decreases. The time to reach Cmax in plasma (3-5 hours) did not change after repeated doses of the drug, and equilibrium plasma concentrations were reached after 6-7 days.
In HIV-infected patients during the period of stable condition, the average values of Cmax, minimum concentration (Cmin) and area under the concentration-time curve have a linear relationship with the daily dose. In 35 patients receiving efavirenz at a dose of 600 mg once daily, Cmax when the steady-state concentration was reached was 12.9 ± 3.7 μM, Cmin was 5.6 ± 3.2 μM, and the area under the concentration-time curve was 184 ± 73 μM per hour.
Effect of food on absorption
Efavirenz can be taken with or without food. Taking efavirenz with food may increase its effect and lead to an increase in the incidence of adverse reactions. The bioavailability of a single 600 mg dose of efavirenz in healthy volunteers increased when the tablets were taken with a normal-fat or high-fat meal by 22% and 17%, respectively, compared with the same dose taken on an empty stomach. It is recommended to take efavirenz before bed on an empty stomach.
Distribution
Efavirenz is highly bound to plasma proteins (approximately 99.5-99.75%), primarily to albumin. In HIV-infected patients (N = 9) who received efavirenz in doses of 200 to 600 mg once daily for at least one month, drug concentrations in the cerebrospinal fluid ranged from 0.26 to 1.19% (mean 0.69%) of the corresponding plasma concentrations. This figure is approximately 3 times higher than the concentration of the non-protein-bound (free) fraction of efavirenz in blood plasma.
Metabolism
Clinical and in vitro studies using human liver microsomes have shown that efavirenz is metabolized primarily by the cytochrome P450 system to hydroxylated derivatives, which then bind to glucuronic acid to form glucuronides. These metabolites are generally inactive against HIV-1. In vitro studies suggest that CYP3A4 and CYP2B6 are the main isoenzymes involved in the metabolism of efavirenz. In vitro studies have shown that efavirenz at concentrations corresponding to those in plasma inhibits the isoenzymes CYP2C9, CYP2C19 and CYP3A4 of the cytochrome P450 system. In in vitro studies, efavirenz did not inhibit CYP2E1 and inhibited CYP206 and CYP1A2 only at concentrations much higher than those in clinical practice.
Efavirenz has been shown to induce cytochrome P450 enzymes, leading to the induction of its own metabolism. With repeated dosing of 200-400 mg per day for 10 days, there was less accumulation of the drug than expected (22-42% lower) and a shorter final half-life of 40-55 hours (single dose half-life is 52-76 hours). The degree of induction of the CYP3A4 isoenzyme is similar when administered doses of efavirenz 400 mg and 600 mg. Pharmacokinetic interactive studies have shown that daily administration of 400 mg or 600 mg of efavirenz in combination with indinavir does not cause a further reduction in the area under the concentration-time curve of indinavir compared with cases when a dose of efavirenz 200 mg was prescribed.
Removal
Efavirenz has a relatively long half-life, ranging from 52 to 76 hours after a single dose and 40 to 55 hours after long-term use. Approximately 14-34% of the isotope-labeled dose of efavirenz is found in urine; less than 1% of the dose of efavirenz is excreted unchanged by the kidneys.
Pharmacokinetics in special groups of patients
Liver failure
With a single dose of efavirenz, a two-fold increase in its half-life was observed in one patient with severe hepatic impairment (Child-Pugh class C), indicating an increased degree of accumulation in such cases. With repeated doses of efavirenz, there was no significant effect of liver damage on the pharmacokinetics of efavirenz in patients with mild hepatic impairment (Child-Pugh class A) compared with patients in the control group. There are currently insufficient data to conclude whether moderate to severe hepatic impairment (Child-Pugh class B and C) affects the pharmacokinetics of efavirenz (see Contraindications, Precautions).
Kidney failure
The pharmacokinetics of efavirenz in patients with renal impairment have not been studied, however, due to the fact that less than 1% of the efavirenz dose is excreted unchanged by the kidneys, impaired renal function should not have a significant effect on the elimination of efavirenz (see section “Special Instructions”).
Gender and race
In men and women, as well as in patients of different races, the pharmacokinetic parameters of efavirenz are similar.
Age
No pharmacokinetic differences were observed between patients 65 years of age and older and younger patients, although clinical studies of efavirenz did not include a sufficient number of patients 65 years of age and older.
Children
Efavirenz has not been studied in children under 3 years of age and in patients weighing less than 13 kg. The pharmacokinetics of efavirenz in children and adults were similar. In 49 children receiving a dose equivalent to 600 mg of efavirenz (dose calculated based on body weight), Cmax was 14.2 μM, Cmin was 5.6 μM, and AUC was 218 μM per hour.
Special instructions
Special instructions
Efavirenz should not be used as the sole treatment for HIV infection, nor should it be added as the sole treatment to an ineffective treatment regimen.
During therapy, the risk of transmitting HIV infection to others during sexual contact or through blood cannot be excluded. In this regard, appropriate precautions should be taken.
Concomitant use of efavirenz with fixed combinations containing efavirenz, emtricitabine and tenofovir disoproxil fumarate is not recommended unless dose adjustment is required (for example, when used concomitantly with rifampicin). When prescribing drugs that should be taken concomitantly with efavirenz, the doctor should refer to the appropriate “Instructions for Medical Use” for these drugs. If any antiretroviral drug is discontinued in combination therapy due to suspected intolerance, simultaneous discontinuation of all antiretroviral drugs should be considered. All discontinued antiretroviral drugs should be resumed immediately after symptoms of intolerance have resolved.
Interrupted monotherapy followed by repeated doses of antiretroviral drugs is not recommended due to the increased likelihood of selection of mutagenic viruses that are resistant to therapy.
The use of efavirenz with Gingo Biloba extracts is not recommended.
Taking efavirenz with food may increase its effect and lead to an increase in the incidence of adverse reactions. Therefore, it is recommended to use the drug before bed on an empty stomach.
Skin rash: In clinical studies of efavirenz, mild to moderate rash was reported and usually resolved with continued therapy. Taking appropriate H1-receptor blockers and/or glucocorticosteroid drugs may improve tolerability and promote rapid resolution of the rash. Severe rash accompanied by blistering, desquamation, or ulceration occurred in less than 1% of patients receiving efavirenz. Multimorphic exudative erythema or Stevens-Johnson syndrome occurred in 0.14% of cases. If patients develop severe rash accompanied by blistering, desquamation involving mucous membranes, or fever, efavirenz should be stopped immediately. If efavirenz therapy is discontinued, consideration should be given to discontinuing other antiretroviral agents to avoid the emergence of treatment-resistant virus.
Rash was observed in 26 of 57 (46%) children receiving efavirenz for 48 weeks, with three patients experiencing severe rash. Prescribing H1-histamine receptor blockers before starting efavirenz therapy in children to prevent rash may be advisable.
Psychiatric symptoms: There is evidence of psychiatric adverse events in patients receiving efavirenz. Patients with a history of mental disorders are at increased risk of developing serious adverse mental events. There are also post-marketing data on cases of suicide, delusional ideas and psychosis-like behavior. Patients should be advised that if they develop these symptoms, they should contact their physician immediately. The physician should determine the possible relationship of these symptoms with taking efavirenz, and, if this connection is confirmed, assess the balance of risk for the patient with continued therapy and the potential benefits of taking the drug (see section “Precautions”).
Nervous system symptoms: Patients receiving efavirenz 600 mg once daily in clinical trials often experience the following symptoms: dizziness, insomnia, drowsiness, decreased concentration, dream pathology, and other adverse effects. Symptoms from the nervous system are usually observed during the first or second day of therapy and in most cases disappear after the first 2-4 weeks. Patients should be informed that such symptoms, if they occur, usually disappear with continued therapy and are not a sign of possible mental disorders, which are less common.
Immune reconstitution syndrome: HIV-infected patients with severe immunodeficiency may develop an inflammatory response to asymptomatic or residual opportunistic infections during initiation of antiretroviral therapy, which can cause serious deterioration or worsening of symptoms. As a rule, such reactions are observed in the first weeks or months after starting antiretroviral therapy. The most significant examples are cytomegalovirus retinitis, generalized and/or focal mycobacterial infection, and pneumonia caused by Pneumocystis jiroveci (formerly Pneumocystis carinii). Any symptoms of inflammation must be identified and treatment prescribed if necessary.
Autoimmune diseases (eg, Graves’ disease) have been observed in the setting of immune reconstitution, but the timing of initial manifestations varies, and the disease may occur many months after the start of therapy. Lipodystrophy and metabolic disorders
Combination antiretroviral therapy is associated with redistribution of body fat (lipodystrophy) in HIV-infected patients, including depletion of peripheral and facial subcutaneous fat, accumulation in the intraperitoneal space, viscera, back of the neck (“buffalo hump”), and mammary hypertrophy. Combination antiretroviral therapy may cause metabolic abnormalities such as hypertriglyceridemia, hypercholesterolemia, insulin resistance, hyperglycemia and hyperlactatemia.
Osteonecrosis
Cases of osteonecrosis have been reported, especially in patients with common risk factors (corticosteroid use, alcohol consumption, acute immunosuppression, increased mass index), advanced HIV infection, or on long-term combination antiretroviral therapy. Patients should be advised to consult a doctor if they experience joint pain, joint stiffness, or difficulty moving.
Special patient groups
Liver disease: Efavirenz is contraindicated in patients with severe hepatic impairment (Child-Pugh class C) (see Contraindications section) and is not recommended in patients with moderate hepatic impairment as there are insufficient data at this time to determine whether dosage adjustments are necessary in such cases. Due to the extensive metabolism of efavirenz by the cytochrome P450 system and limited clinical experience with the use of efavirenz in patients with chronic liver disease, the drug should be administered with caution to patients with mild hepatic impairment (see section “Caution”). In this case, patients should be monitored for timely detection of dose-dependent adverse reactions, especially from the nervous system. Laboratory tests should also be performed at regular intervals to assess the condition of the liver.
The safety and effectiveness of efavirenz have not been established in patients with a history of significant liver impairment. Patients with chronic hepatitis B and C who are taking combination antiretroviral therapy (ART) are at risk of developing severe liver adverse reactions that can be fatal. Patients with a history of liver dysfunction, including chronic active hepatitis, have an increased incidence of liver dysfunction with combination ART and should be monitored according to a standard regimen. In patients with worsening liver disease or persistent elevations in serum transaminases greater than 5 times the upper limit of normal, the benefit of continued efavirenz therapy must be weighed against the potential risk of hepatotoxicity. In such patients, the advisability of interrupting or discontinuing ART should be considered.
When using other drugs with known hepatotoxicity simultaneously, it is recommended to monitor the activity of liver enzymes. Patients with hepatitis B or C should also follow the instructions for use of the prescribed drugs for the treatment of hepatitis B or C when prescribing combination antiviral therapy.
Renal impairment: The pharmacokinetics of efavirenz in patients with renal impairment have not been studied, however, due to the fact that less than 1% of the amount of efavirenz is excreted unchanged by the kidneys, impaired renal function should not have a significant effect on the elimination of efavirenz.
There is no experience of use in patients with severe renal failure, therefore, in this group of patients, when using the drug, monitoring is recommended to assess the safety of therapy.
Elderly patients: Since a small number of elderly patients were included in clinical studies, it is not possible to assume that the effect of the drug in elderly patients differs from that in younger patients (see section Pharmacokinetics).
Children: Efavirenz has not been studied in children younger than 3 years or weighing less than 13 kg. There is evidence that the pharmacokinetics of efavirenz may be altered in very young children.
Seizures: Seizures have been observed extremely rarely in patients receiving efavirenz, including in patients with a history of seizures. In patients receiving concomitant anticonvulsants with predominant metabolism in the liver, such as phenytoin, carbamazepine and phenobarbital, it is necessary to periodically monitor their plasma concentrations. Caution should be exercised when prescribing the drug to patients with a history of seizures (see sections “With caution” and “Side effects”).
Liver enzymes: In patients with a known or suspected history of hepatitis B or C and in patients taking medications associated with liver toxicity, regular monitoring of liver enzyme activity is recommended. In patients with persistent increases in serum transaminases above 5 times the upper limit of normal, the benefit of continuing efavirenz therapy must be weighed against the possible risk of hepatotoxicity (see Adverse Reactions section).
Cholesterol: in patients taking efavirenz, blood cholesterol concentrations should be monitored (see section “Side effects”).
Interaction with cannabinoid testing: Efavirenz does not bind to cannabinoid receptors, but there have been reports of false-positive urine cannabinoid testing results in uninfected volunteers receiving efavirenz. False-positive test results were observed only with the CEDIA DAU Multi-Level TIS assay, which is used for screening, and were not observed with other cannabinoid tests, including tests used to confirm positive results.
Impact on the ability to drive vehicles and machinery
No studies have been conducted to examine the effects on driving and device use. Efavirenz may cause dizziness, difficulty alerting, and/or insomnia. Patients should be warned that if they experience any of these symptoms, they should avoid driving and operating devices.
Active ingredient
Active ingredient
Efavirenz
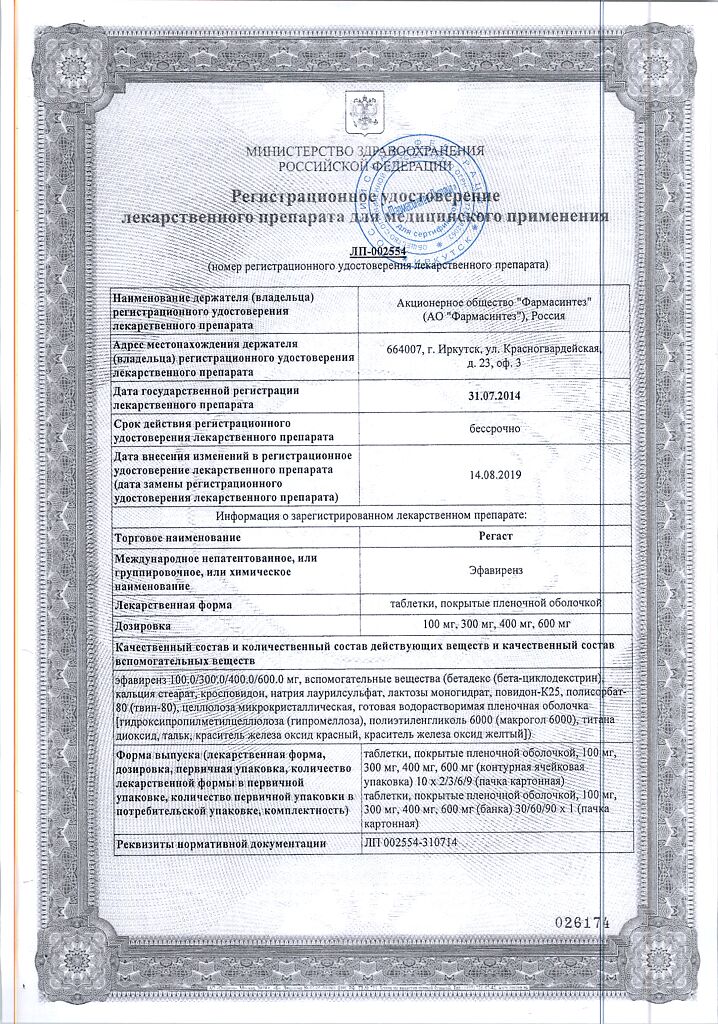
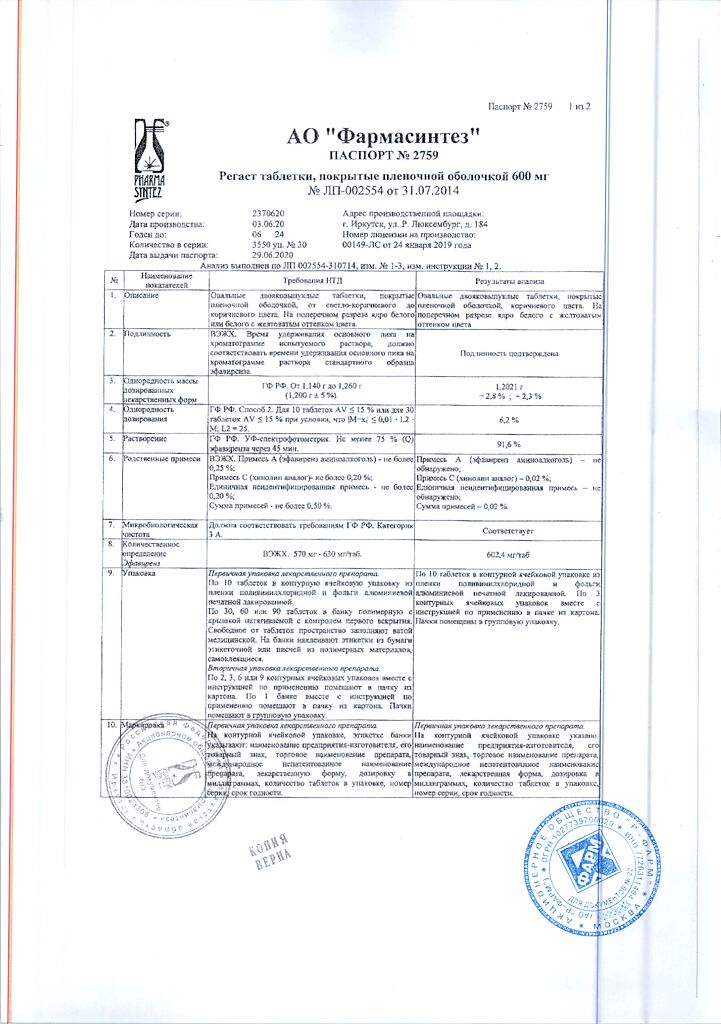
Composition
Composition
For 1 tablet:
active substance: Efavirenz 600 mg
excipients:
Core: betadex (beta-cyclodextrin) – 12.0 mg; calcium stearate – 6.0 mg; crospovidone – 72.0 mg; sodium lauryl sulfate – 21.0 mg; lactose monohydrate – 372.0 mg; povidone K 25 – 24.0 mg; polysorbate-80 (Tween-80) – 9.0 mg, microcrystalline cellulose – 54.0 mg.
Film shell: Ready-made water-soluble film shell – 30.0 mg (Shell composition: hydroxypropyl methylcellulose (hypromellose) – 74.2%, polyethylene glycol 6000 (Macrogol 6000) – 14.3%, titanium dioxide – 3.5%, talc – 2.3%, red iron oxide dye – 1.4%, dye iron oxide yellow – 4.3%).
Pregnancy
Pregnancy
There are no adequate and well-controlled studies of efavirenz in pregnant women. Efavirenz should not be used during pregnancy unless its use is necessary (the potential benefit to the mother outweighs the risk to the fetus and there are no other appropriate treatment alternatives). Women taking efavirenz should avoid becoming pregnant. In addition to oral or other hormonal contraceptives, other reliable methods of contraception should be used, including for 12 weeks after stopping treatment with efavirenz.
It is not known whether efavirenz is excreted in human breast milk. Because data from animal studies indicate that the drug may pass into breast milk, breastfeeding is not recommended for women taking efavirenz during lactation. Under any circumstances, HIV-infected mothers are not recommended to breastfeed to avoid HIV transmission.
Contraindications
Contraindications
hypersensitivity to any of the components of the drug;
lactase deficiency, lactose intolerance, glucose-galactose malabsorption;
severe liver failure (class C according to the Child-Pugh classification);
children under 3 years of age or weighing less than 13 kg;
simultaneous use with terfenadine, astemizole, cisapride, pimozide, bepridil, midazolam, triazolam and ergot alkaloids, since the competitive interaction of efavirenz with the CYP3A4 isoenzyme can lead to suppression of the metabolism of these drugs and the emergence of preconditions for the occurrence of serious and/or life-threatening adverse events (for example, cardiac arrhythmia, prolonged sedation or respiratory depression);
simultaneous use with saquinavir as the only protease inhibitor, other non-nucleoside reverse transcriptase inhibitors (see section “Interaction with other drugs”);
simultaneous use with drugs containing St. John’s wort (Hypericum perforatum), since this may reduce the concentration of efavirenz in the blood plasma and reduce its clinical effect.
With caution
patients with a history of psychiatric disorders are at increased risk of developing serious adverse mental events;
when prescribing efavirenz to patients with mild to moderate liver dysfunction (Class A and B according to the Child-Pugh classification);
when prescribing efavirenz to patients with convulsions (including a history) (see section “Special instructions”);
patients receiving concomitant anticonvulsants with predominantly hepatic metabolism, such as phenytoin, carbamazepine and phenobarbital (blood concentrations should be monitored periodically)
Side Effects
Side Effects
In general, efavirenz was well tolerated. Side effects possibly causally related to the use of the drug are presented below. The frequency of events is determined using the following assumption: very common (>1/10); often (>1/100, 1/1000, 1/10000, <1/1,000); very rare (< 1/10000).Immune system disorders: Uncommon: hypersensitivity reactions.Mental disorders: Common: pathological dreams, anxiety, depression, insomnia. Uncommon: tendency to affect, aggressiveness, confusion, euphoria, hallucinations, mania, paranoid behavior, psychosis, suicidal intent, suicide attempt. Rare: delirium, neurosis, death due to suicide.Nervous system disorders: Common: disorders of cerebellar coordination and balance, attention disorder, dizziness, headaches, drowsiness. Uncommon: anxiety agitation, amnesia, ataxia, incoordination, convulsions, impaired thinking, tremor.Endocrine system disorders: Uncommon: gynecomastia.Metabolic disorders: Common: hypertriglyceridemia. Uncommon: hypercholesterolemia.Visual disturbances: Uncommon: blurred vision.Hearing and labyrinthine disorders: Uncommon: vertigo, tinnitus.From the respiratory system: Rarely – shortness of breath.From the cardiovascular system: Rarely – palpitations.Gastrointestinal disorders: Common: abdominal pain, diarrhea, nausea, vomiting. Uncommon: pancreatitis, asymptomatic increase in serum amylase activity.Liver and biliary tract disorders: Common: increased activity of aspartate aminotransferase (AST), alanine aminotransferase (ALT) and gamma-glutamyltransferase (GGT). Uncommon: acute hepatitis. Rare: liver failure.From the musculoskeletal system: Uncommon: myalgia, arthralgia, myopathy, osteonecrosis.Skin and subcutaneous tissue disorders: Very common: rash. Often: skin itching. Uncommon: erythema multiforme exudative, Stevens-Johnson syndrome. Rare: photoallergic dermatitis.General disorders: Common: increased fatigue. Uncommon: asthenia, “flushes” of blood to the facial skin.Immune reconstitution syndromeIn HIV-infected patients with severe immunodeficiency when initiating combination antiretroviral therapy, the risk of inflammatory reactions to asymptomatic or residual opportunistic infections may increase. Autoimmune diseases (eg, Graves’ disease) have been observed in the setting of immune reconstitution, but the timing of initial manifestations varies, and the disease may occur many months after the start of therapy.Lipodystrophy and metabolic disordersCombination antiretroviral therapy is associated with redistribution of body fat (lipodystrophy) in HIV-infected patients, including depletion of peripheral and facial subcutaneous fat, accumulation in the intraperitoneal space, viscera, back of the neck (“buffalo hump”), and mammary hypertrophy. Combination antiretroviral therapy may cause metabolic abnormalities such as hypertriglyceridemia, hypercholesterolemia, insulin resistance, hyperglycemia and hyperlactatemia.Children and teenagersThe type and frequency of adverse events in children is generally similar to that in adults, with the exception of rash, which is more common and more severe in children than in adults. Prescribing appropriate H1-blockers to children before starting efavirenz therapy to prevent rash may be advisable.
Interaction
Interaction
Efavirenz in vivo is an inducer of the isoenzymes CYP3A4, CYP2B6 and UDP-GT1A1. Plasma concentrations of compounds that are substrates for these isoenzymes may be reduced when administered concomitantly with efavirenz. Efavirenz may be an inducer of the CYP2C19 and CYP2C9 isoenzymes, but inhibition of these isoenzymes has also been observed in vitro. The effect of simultaneous use of efavirenz with compounds that are substrates for these isoenzymes is not clear.
Exposure to efavirenz may be decreased when coadministered with certain drugs (eg, ritonavir) or foods (eg, grapefruit juice) that inhibit CYP3A4 or CYP2B6. Compounds or herbal preparations (for example, those containing Gingo Biloba extract, as well as St. John’s wort) that induce these isoenzymes may lead to a decrease in efavirenz plasma concentrations. Simultaneous use with drugs containing St. John’s wort is contraindicated. Concomitant use with Gingo Biloba extracts is not recommended.
Contraindicated combination therapy
Concomitant use of efavirenz with terfenadine, astemizole, cisapride, pimozide, bepridil, midazolam, triazolam, and ergot alkaloids (e.g., ergotamine, dihydroergotamine, ergonovine, or methylergonovine) is contraindicated because inhibition of their metabolism by efavirenz may cause serious, life-threatening effects. (see “Contraindications”).
St. John’s wort (Hypericum perforatum): the use of drugs/products containing St. John’s wort is contraindicated in patients taking efavirenz. Plasma concentrations of efavirenz may be reduced when administered concomitantly with St. John’s wort, as it causes the induction of enzymes and/or transport proteins responsible for drug metabolism. If the patient is already taking drugs/products containing St. John’s wort, the latter should be discontinued, the concentration of the virus in the blood and, if possible, the concentration of efavirenz in the blood should be checked. After discontinuation of drugs/products containing St. John’s wort, the concentration of efavirenz may increase and then a dose adjustment of efavirenz will be required. The effect of St. John’s wort, associated with enzyme induction, may persist for at least 2 weeks after its discontinuation (see “Contraindications”),
Other interactions
Interactions between efavirenz and HIV protease inhibitors, other antiretroviral drugs other than HIV protease inhibitors, and between efavirenz and non-antiretroviral drugs are listed in Table 2 below. An increase in the value of the indicator is indicated by an arrow “↑”, a decrease in the value – by an arrow “↓”, if the indicator remains unchanged – by an arrow “↔”. Where appropriate, 90% and 95% confidence intervals are presented in parentheses. Studies were generally conducted on healthy volunteers unless otherwise specifically stated.
Overdose
Overdose
Some patients who accidentally took efavirenz 600 mg twice daily experienced an increase in nervous system symptoms. One patient experienced involuntary muscle contractions.
In case of efavirenz overdose, treatment should consist of general supportive measures, including monitoring vital signs and monitoring the patient’s clinical condition. Activated carbon can be used to remove unabsorbed drug. There is no specific antidote for the treatment of efavirenz overdose. Because efavirenz is highly protein bound, it is unlikely that significant removal of the drug from the blood can be achieved by dialysis.
Storage conditions
Storage conditions
In the manufacturer’s original packaging at a temperature not exceeding 25 °C.
Keep out of the reach of children.
Shelf life
Shelf life
2 years. Do not use after the expiration date indicated on the package.
Manufacturer
Manufacturer
Pharmasintez JSC, Russia
Additional information
| Shelf life | 2 years. Do not use after the expiry date printed on the package. |
|---|---|
| Conditions of storage | In the original manufacturer's package at a temperature not exceeding 25 ° C. Keep out of reach of children. |
| Manufacturer | Pharmasintez JSC, Russia |
| Medication form | pills |
| Brand | Pharmasintez JSC |
Related products
Buy Regast, 600 mg 30 pcs. with delivery to USA, UK, Europe and over 120 other countries.