No products in the cart.
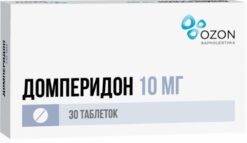
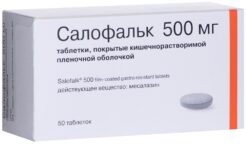
Raso, 10 mg 30 pcs.
€1.00
Out of stock
(E-mail when Stock is available)
EAN: 8901148233904
SKU: 265117
Categories: Medicine, Stomach, intestines, liver, Ulcer and gastritis
Description
Pharmacodynamics
Mechanism of action
Rabeprazole belongs to the class of antisecretory drugs which are chemically substituted benzimidazoles. Rabeprazole inhibits the activity of the enzyme H+/K+ATPase (“proton pump”), thus blocking the final stage of hydrochloric acid synthesis. This effect is dose-dependent and leads to inhibition of both basal and stimulated hydrochloric acid secretion regardless of the irritant.
Rabeprazole has no anticholinergic properties.
Antisecretory activity
After oral administration of 20 mg rabeprazole the antisecretory effect occurs within one hour. Inhibition of basal and stimulated hydrochloric acid secretion 23 h after the first dose of rabeprazole is 62% and 82%, respectively, and continues until 48 h. This duration of pharmacokinetic action is much longer than that predicted by the half-life (T1/2), which is approximately 1 h. This effect can be explained by the binding of the drug substance to the H+/K+ATPase of the gastric parietal cells. The magnitude of rabeprazole inhibitory effect on acid secretion reaches a plateau after three days of taking rabeprazole. On discontinuation of rabeprazole secretory activity is restored within 1-2 days.
Effect on serum gastrin concentration
At the beginning of therapy with rabeprazole serum gastrin concentration increases, which is a reflection of the inhibitory effect on hydrochloric acid secretion. Gastrin concentration usually returns to the initial level within 1-2 weeks after discontinuation of treatment.
Effect on enterochromaffin-like cells
A study of gastric fundus and intralesional biopsy specimens from more than 500 patients treated with rabeprazole or a comparison drug for up to 8 weeks showed no changes in the morphological structure of enterochromaffin-like (ECL) cells, gastritis severity, frequency of atrophic gastritis, intestinal metaplasia or prevalence of Helicobacter pylori infection.
In a study involving more than 400 patients receiving rabeprazole at a dose of 10 mg/day or 20 mg/day, lasting up to 1 year, the incidence of hyperplasia was low and comparable to that of patients receiving omeprazole at a dose of 20 mg/day. No cases of adenomatous changes or carcinoid tumors observed
in rats were reported.
Other effects
There is currently no evidence that rabeprazole causes systemic effects on the central nervous system (CNS), cardiovascular and respiratory systems. When administered orally in dose of 20 mg during 2 weeks rabeprazole has no effect on thyroid function, carbohydrate metabolism as well as on concentrations in blood of parathyroid hormone, cortisol, estrogen, testosterone, prolactin, secretin, glucagon, follicle stimulating hormone, luteinizing hormone, renin, aldosterone and somatotropin.
Pharmacokinetics
Absorption
Rabeprazole is rapidly absorbed from the intestine and its maximum plasma concentration (Cmax) is reached approximately 3.5 h after a dose of 20 mg. Changes in Cmax and values of area under the pharmacokinetic curve “concentration-time” (AUC) of rabeprazole are linear in the dose range from 10 to 40 mg. Absolute bioavailability after oral administration of 20 mg (compared with intravenous administration) is about 52%. In addition, bioavailability does not change with repeated administration of rabeprazole. Neither the time of the drug intake within a day, nor antacids affect absorption of rabeprazole. Taking rabeprazole with fatty food slows down absorption of rabeprazole by 4 hours or more, but neither Cmax nor degree of absorption changes.
Distribution
In humans the degree of binding of rabeprazole to plasma proteins is about 97%.
Metabolism
Rabeprazole is metabolized in the body in two ways. Much of it is metabolized systemically by a non-enzymatic route with the formation of thioether derivatives. Rabeprazole is also metabolized in the liver via cytochrome P450 to form sulfonic and desmethyl derivatives.
In healthy volunteers, the plasma elimination half-life is approximately 1 h (range 0.7 to 1.5 h) and total clearance is 3.8 ml/min/kg.
Elevation
After a single oral administration of 20 mg of 14C-labeled rabeprazole, about 90% of rabeprazole is excreted by the kidneys, mainly as a carboxylic acid thioester, its glucuronide, and as mercapturic acid derivatives. Unchanged rabeprazole is not detected in the urine. The remaining part of rabeprazole taken is excreted through the intestine. Total excretion is 99.8%.
Terminal stage of renal failure
In patients with stable renal failure in the terminal stage who require maintenance hemodialysis (creatinine clearance <5 ml/min/1.73 m2), the excretion of rabeprazole is similar to that of healthy volunteers. AUC and Cmax in these patients were approximately 35% lower than in healthy volunteers. The average T1/2 of rabeprazole was 0.82 h in healthy volunteers, 0.95 h in patients during hemodialysis and 3.6 h after hemodialysis. Clearance of rabeprazole in patients with kidney disease requiring hemodialysis was approximately twice as high as in healthy volunteers.
Chronic compensated cirrhosis
Patients with chronic compensated cirrhosis tolerated rabeprazole well at a dose of 20 mg once daily, although AUC doubled and Cmax increased by 50%, compared with healthy volunteers.
Elderly patients
The elimination of rabeprazole is somewhat delayed in elderly patients. After 7 days of taking rabeprazole at a dose of 20 mg once daily, the AUC was approximately twice as high and Cmax was increased by 60%, compared to young healthy volunteers; no evidence of rabeprazole cumulation was noted.
CYP2C19 polymorphism
In patients with delayed metabolism via CYP2C19 isoenzyme after 7 days of taking rabeprazole at a dose of 20 mg daily the AUC increased 1.9 times and half-life increased 1.6 times compared to the same parameters in “fast metabolizers”, while Cmax increased by 40%.
Indications
Indications
Symptoms of dyspepsia associated with increased acidity of gastric juice, including symptoms of gastroesophageal reflux disease (heartburn, sour belching).
Pharmacological effect
Pharmacological effect
Pharmacodynamics
Mechanism of action
Rabeprazole belongs to the class of antisecretory agents, which are chemically substituted benzimidazoles. Rabeprazole inhibits the activity of the enzyme H+/K+ATPase (“proton pump”), thereby blocking the final stage of hydrochloric acid synthesis. This effect is dose-dependent and leads to inhibition of both basal and stimulated secretion of hydrochloric acid, regardless of the stimulus.
Rabeprazole does not have anticholinergic properties.
Antisecretory activity
After oral administration of 20 mg of rabeprazole, the antisecretory effect occurs within an hour. The inhibition of basal and stimulated secretion of hydrochloric acid 23 hours after taking the first dose of rabeprazole is 62% and 82%, respectively, and lasts up to 48 hours. This duration of pharmacokinetic action is much longer than that predicted by the half-life (T1/2), which is approximately 1 hour. This effect can be explained by the binding of the drug to the H+/K+ATPase of gastric parietal cells. The magnitude of the inhibitory effect of rabeprazole on acid secretion reaches a plateau after three days of taking rabeprazole. When you stop taking it, secretory activity is restored within 1-2 days.
Effect on serum gastrin concentration
At the beginning of rabeprazole therapy, the concentration of gastrin in the blood serum increases, which is a reflection of the inhibitory effect on the secretion of hydrochloric acid. Gastrin concentrations return to baseline levels usually within 1-2 weeks after cessation of treatment.
Effect on enterochromaffin-like cells
A study of biopsies of the fundus and antrum of more than 500 patients treated with rabeprazole or a comparator for up to 8 weeks found no changes in the morphological structure of enterochromaffin-like (ECL) cells, the severity of gastritis, the incidence of atrophic gastritis, intestinal metaplasia, or the prevalence of Helicobacter pylori infection.
In a study of more than 400 patients receiving rabeprazole 10 mg/day or 20 mg/day for up to 1 year, the incidence of hyperplasia was low and comparable to that of patients receiving omeprazole 20 mg/day. There have been no cases of adenomatous changes or carcinoid tumors observed
in rats.
Other effects
There is currently no evidence that rabeprazole causes systemic effects on the central nervous system (CNS), cardiovascular or respiratory systems. When taken orally at a dose of 20 mg for 2 weeks, rabeprazole has no effect on thyroid function, carbohydrate metabolism, as well as on blood concentrations of parathyroid hormone, cortisol, estrogens, testosterone, prolactin, secretin, glucagon, follicle-stimulating hormone, luteinizing hormone, renin, aldosterone and somatotropin.
Pharmacokinetics
Absorption
Rabeprazole is rapidly absorbed from the intestine and its maximum plasma concentration (Cmax) is reached approximately 3.5 hours after administration of a 20 mg dose. The change in Cmax and area under the pharmacokinetic concentration-time curve (AUC) of rabeprazole are linear in the dose range from 10 to 40 mg. Absolute bioavailability after oral administration of 20 mg (compared to intravenous administration) is approximately 52%. In addition, bioavailability does not change with repeated dosing of rabeprazole. Neither the time of taking the drug during the day nor antacids affect the absorption of rabeprazole. Taking rabeprazole with a fatty meal slows down the absorption of rabeprazole by 4 hours or more, but neither the Cmax nor the extent of absorption changes.
Distribution
In humans, the binding rate of rabeprazole to plasma proteins is approximately 97%.
Metabolism
Rabeprazole is metabolized in the body in two ways. A significant part of it is metabolized systemically by a non-enzymatic route with the formation of thioester derivatives. Rabeprazole is also metabolized in the liver via cytochrome P450 to form sulfonic and desmethyl derivatives.
In healthy volunteers, the plasma half-life is approximately 1 hour (varies from 0.7 to 1.5 hours), and the total clearance is 3.8 ml/min/kg.
Removal
After a single oral dose of 20 mg of 14C-labeled rabeprazole, about 90% of rabeprazole is excreted by the kidneys, mainly in the form of carboxylic acid thioester, its glucuronide and in the form of mercapturic acid derivatives. Unchanged rabeprazole is not detected in urine. The remainder of the rabeprazole taken is excreted through the intestines. The total elimination is 99.8%.
End stage renal failure
In patients with stable end-stage renal disease who require maintenance hemodialysis (creatinine clearance <5 ml/min/1.73 m2), the elimination of rabeprazole is similar to that of healthy volunteers. AUC and Cmax in these patients were approximately 35% lower than in healthy volunteers. On average, T1/2 of rabeprazole was 0.82 hours in healthy volunteers, 0.95 hours in patients during hemodialysis and 3.6 hours after hemodialysis. The clearance of rabeprazole in patients with kidney disease requiring hemodialysis was approximately twice as high as in healthy volunteers.Chronic compensated cirrhosisPatients with chronic compensated liver cirrhosis tolerate rabeprazole 20 mg once daily, although AUC is doubled and Cmax is increased by 50% compared to healthy volunteers.
Elderly patients
In elderly patients, the elimination of rabeprazole is somewhat slower. After 7 days of rabeprazole 20 mg once daily in elderly subjects, AUC was approximately twice as high and Cmax was increased by 60% compared with young healthy volunteers; There were no signs of rabeprazole accumulation.
CYP2C19 polymorphism
In patients with slow metabolism via the CYP2C19 isoenzyme, after 7 days of taking rabeprazole at a dose of 20 mg per day, the AUC increases by 1.9 times and the half-life by 1.6 times, compared with the same parameters in “rapid metabolizers,” while Cmax increases by 40%.
Special instructions
Special instructions
The patient’s response to rabeprazole therapy does not exclude the presence of malignant neoplasms in the stomach.
Razo® tablets should not be chewed or crushed. The tablets should be swallowed whole. It has been established that neither time of day nor food intake affects the activity of rabeprazole.
In a special study in patients with mild or moderate hepatic impairment, the incidence of side effects of rabeprazole was not found to be significantly different from that in age- and sex-matched healthy individuals, but despite this, caution is recommended when first using rabeprazole in patients with severe hepatic impairment. The AUC of rabeprazole in patients with severe hepatic impairment is approximately two times higher than in healthy patients.
No dosage adjustment of rabeprazole is required for patients with impaired renal or hepatic function.
Hypomagnesemia
When treated with proton pump inhibitors for at least 3 months, cases of symptomatic or asymptomatic hypomagnesemia have been reported in rare cases. In most cases, these reports were received one year after therapy. Serious adverse events included tetany, arrhythmia, and seizures. Most patients required treatment for hypomagnesemia, including magnesium replacement and discontinuation of proton pump inhibitor therapy. In patients who will be receiving long-term treatment or who are taking proton pump inhibitors with drugs such as digoxin or drugs that can cause hypomagnesemia (eg, diuretics), healthcare providers should monitor magnesium levels before starting treatment with proton pump inhibitors and during treatment.
Patients should not take other acid-reducing agents, such as H2 blockers or proton pump inhibitors, at the same time as rabeprazole.
Bone fractures
Observational studies suggest that proton pump inhibitor therapy may increase the risk of osteoporosis-related fractures of the hip, wrist, or spine. The risk of fractures was increased in patients receiving high doses of PPIs for a long time (a year or more).
Concomitant use of rabeprazole with methotrexate
According to the literature, simultaneous use of PPIs with methotrexate (primarily in high doses) can lead to increased concentrations of methotrexate and/or its metabolite hydroxymethotrexate and increase the half-life, which can lead to methotrexate toxicity. If high doses of methotrexate are required, temporary discontinuation of PPI therapy may be considered.
Clostridium difficile
PPI therapy may lead to an increased risk of gastrointestinal infections such as Clostridium difficile.
Based on the pharmacodynamics of rabeprazole and its profile of undesirable effects, it is unlikely that rabeprazole affects the ability to drive vehicles and perform other activities that require concentration and speed of psychomotor reactions. However, if drowsiness or dizziness occurs, these activities should be avoided.
Active ingredient
Active ingredient
Rabeprazole
Composition
Composition
Each 10 mg enteric-coated tablet contains:
Active ingredient:
Rabeprazole sodium 10 mg
Excipients:
Mannitol,
Low-substituted hyprolose
Magnesium oxide heavy
Hypromellose (5cps)
Sodium lauryl sulfate
Talc
Magnesium stearate
Shell:
Zein
Triethyl citrate
Enteric coating:
Methacrylic acid and ethyl acrylate copolymer [1:1] (methacrylic acid copolymer (type C))
triethyl citrate
Talc
Shell:
Opadry pink 03B54475 (hypromellose 6 cP, titanium dioxide (E171), macrogol-400, red iron oxide dye (E172))
Composition of black ink for writing on a 10 mg tablet:
Shellac glaze 45%
Iron oxide dye black (E172)
Isopropyl alcohol
N-butanol
Propylene glycol
Ammonia solution concentrated 28%
Pregnancy
Pregnancy
There are no data on the safety of rabeprazole during pregnancy.
Reproduction studies in rats and rabbits showed no evidence of impaired fertility or fetal developmental defects associated with rabeprazole; however, in rats the drug crosses the placental barrier in small quantities. Razo® should not be used during pregnancy unless the expected beneficial effect for the mother outweighs the possible harm to the fetus.
It is not known whether rabeprazole passes into breast milk. Appropriate studies have not been conducted in lactating women. However, rabeprazole was found in the milk of lactating rats, so the drug should not be used by lactating women.
Contraindications
Contraindications
Hypersensitivity to rabeprazole, substituted benzimidazoles or to the auxiliary components of the drug;
pregnancy;
breastfeeding period;
children under 18 years of age.
Side Effects
Side Effects
Rabeprazole is usually well tolerated by patients. Side effects are generally mild or moderate and are transient.
The following side effects were observed when taking rabeprazole during clinical studies: headache, abdominal pain, diarrhea, flatulence, constipation, dry mouth, dizziness, rash, peripheral edema.
The frequency of side effects is presented in accordance with the following gradation:
very often (>1/10);
often (1/10 – 1/100);
uncommon (1/100 – 1/1000);
rarely (1/1000 – 1/10000);
very rare (<1/10000).
Immune system disorders
Rarely – acute systemic allergic reactions.
Disorders of the lymphatic system
Rarely – thrombocytopenia, neutropenia, leukopenia.
Metabolic and nutritional disorders
Rarely – hypomagnesemia.
Disorders of the hepatobiliary system
Rarely – increased activity of liver enzymes, hepatitis, jaundice, hepatic encephalopathy.
Renal and urinary tract disorders
Very rarely – interstitial nephritis.
Disorders of the skin and subcutaneous tissues
Rarely – bullous rashes, urticaria; very rarely – erythema multiforme, toxic epidermal necrolysis, Stevens-Johnson syndrome.
Musculoskeletal and connective tissue disorders
Rarely – myalgia, arthralgia.
Reproductive system disorders
Very rarely – gynecomastia.
No changes in laboratory parameters were observed while taking rabeprazole.
When taking proton pump inhibitors, the risk of bone fractures may increase (see section “Special Instructions”).
Interaction
Interaction
When used simultaneously with digoxin, an increase (from small to moderate) in the concentration of digoxin in the blood plasma is possible.
When used simultaneously with ketoconazole, its bioavailability decreases.
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C.
Keep out of the reach of children!
Shelf life
Shelf life
2 years (in cans), 3 years (in blisters).
Do not use after the expiration date stated on the package.
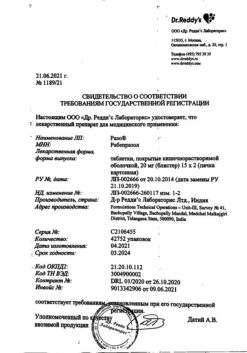
Manufacturer
Manufacturer
Dr. Reddy’s Laboratories Ltd, India
Additional information
| Shelf life | 2 years (in cans), 3 years (in blisters). Do not use after the expiration date stated on the package. |
|---|---|
| Conditions of storage | At the temperature not more than 25 ° C. Keep out of reach of children! |
| Manufacturer | Dr. Reddy's, India |
| Medication form | enteric-soluble film-coated tablets |
| Brand | Dr. Reddy's |
Other forms…
Related products
Buy Raso, 10 mg 30 pcs. with delivery to USA, UK, Europe and over 120 other countries.