No products in the cart.
Ramipril-SZ, tablets 5 mg 30 pcs
€6.31 €5.52
Description
A ACE inhibitor. It is a prodrug from which the active metabolite ramiprilat is formed in the body. It is believed that the mechanism of antihypertensive action is associated with competitive inhibition of ACE activity, which leads to a decrease in the rate of conversion of angiotensin I into angiotensin II, which is a powerful vasoconstrictor. The decrease in angiotensin II concentration results in a secondary increase in plasma renin activity by eliminating the negative feedback of renin release and directly reducing aldosterone secretion. Due to its vasodilator effect, it decreases RPO (post-load), congestion pressure in the pulmonary capillaries (preload) and resistance in the pulmonary vessels; it increases cardiac minute volume and exercise tolerance.
In patients with signs of chronic heart failure after myocardial infarction, ramipril reduces the risk of sudden death, progression of heart failure to severe/resistant failure, and reduces hospitalizations for heart failure.
Ramipril is known to significantly reduce the incidence of myocardial infarction, stroke and cardiovascular death in patients with increased cardiovascular risk due to vascular disease (CHD, previous stroke or peripheral vascular disease) or diabetes with at least one additional risk factor (microalbuminuria, arterial hypertension, high total cholesterol, low HDL, smoking). Reduces overall mortality and the need for revascularization procedures, slows the onset and progression of chronic heart failure. Both in patients with and without diabetes mellitus, ramipril significantly reduces the existing microalbuminuria and the risk of nephropathy. These effects are noted in patients with both elevated and normal BP.
The hypotensive effect of ramipril develops in approximately 1-2 h, peaks within 3-6 h, and lasts at least 24 h.
Pharmacokinetics
In oral administration, absorption is 50-60%; food does not affect the degree of absorption but slows absorption. Cmax is reached after 2-4 hours. It is metabolized in the liver with the formation of the active metabolite ramiprilat (6 times more active ACE inhibitor than ramipril), inactive diketopiperazine and glucuronidized.
All formed metabolites, except for ramiprilat, have no pharmacological activity. Binding to plasma proteins for ramipril is 73%, for ramiprilat – 56%. Bioavailability after oral administration of 2.5-5 mg of ramipril is 15-28%; for ramiprilat it is 45%. After daily administration of ramipril at a dose of 5 mg/day, steady plasma concentration of ramiprilat is reached by day 4.
The T1/2 for ramipril is 5.1 h; in the distribution and elimination phase, serum ramiprilat concentrations fall with a T1/2 of 3 h, followed by a transient phase with a T1/2 of 15 h, and a prolonged end phase with very low plasma ramiprilat concentrations and T1/2 of 4-5 days. T1/2 is increased in chronic renal failure.
The Vd of ramipril is 90 L, of ramiprilat is 500 L. The kidneys excreted 60%, through the intestine – 40% (mainly as metabolites). In renal dysfunction excretion of ramipril and its metabolites slows down in proportion to the decrease of CK; in liver dysfunction conversion to ramiprilat slows down; in heart failure concentration of ramiprilat is 1.5-1.8 times higher.
Indications
Indications
arterial hypertension;
chronic heart failure, incl. after acute myocardial infarction in patients with stable hemodynamics;
diabetic nephropathy and chronic diffuse kidney disease (non-diabetic nephropathy);
reducing the risk of myocardial infarction, stroke or coronary death in patients with coronary artery disease, with an increased risk of cardiovascular diseases, including patients who have had myocardial infarction, percutaneous transluminal coronary angioplasty, coronary artery bypass grafting (in clinically stable condition).
Pharmacological effect
Pharmacological effect
ACE inhibitor. It is a prodrug from which the active metabolite ramiprilat is formed in the body. It is believed that the mechanism of antihypertensive action is associated with competitive inhibition of ACE activity, which leads to a decrease in the rate of conversion of angiotensin I to angiotensin II, which is a powerful vasoconstrictor. As a result of a decrease in the concentration of angiotensin II, a secondary increase in plasma renin activity occurs due to the elimination of negative feedback during the release of renin and a direct decrease in aldosterone secretion. Thanks to its vasodilating effect, it reduces roundabout percentage (afterload), wedge pressure in the pulmonary capillaries (preload) and resistance in the pulmonary vessels; increases cardiac output and exercise tolerance.
In patients with signs of chronic heart failure after myocardial infarction, ramipril reduces the risk of sudden death, progression of heart failure to severe/resistant heart failure, and reduces the number of hospitalizations for heart failure.
Ramipril is known to significantly reduce the incidence of myocardial infarction, stroke and cardiovascular death in patients with increased cardiovascular risk due to vascular disease (coronary artery disease, previous stroke or peripheral vascular disease) or diabetes mellitus who have at least one additional risk factor (microalbuminuria, hypertension, increased total cholesterol, low HDL, smoking). Reduces overall mortality and the need for revascularization procedures, slows the onset and progression of chronic heart failure. In both patients with and without diabetes mellitus, ramipril significantly reduces existing microalbuminuria and the risk of developing nephropathy. These effects are observed in patients with both high and normal blood pressure.
The hypotensive effect of ramipril develops after approximately 1-2 hours, reaches a maximum within 3-6 hours, and lasts for at least 24 hours.
Pharmacokinetics
When taken orally, absorption is 50-60%; food does not affect the degree of absorption, but slows down absorption. Cmax is reached after 2-4 hours. It is metabolized in the liver to form the active metabolite ramiprilat (6 times more active in inhibiting ACE than ramipril), inactive diketopiperazine and glucuronidated.
All metabolites formed, with the exception of ramiprilat, have no pharmacological activity. Plasma protein binding for ramipril is 73%, ramiprilat is 56%. Bioavailability after oral administration of 2.5-5 mg of ramipril is 15-28%; for ramiprilat – 45%. After daily administration of ramipril at a dose of 5 mg/day, a steady-state concentration of ramiprilat in plasma is achieved by day 4.
T1/2 for ramipril – 5.1 hours; in the distribution and elimination phase, a drop in the concentration of ramiprilat in the blood serum occurs with T1/2 – 3 hours, followed by a transition phase with T1/2 – 15 hours, and a long final phase with very low concentrations of ramiprilat in plasma and T1/2 – 4-5 days. T1/2 increases in chronic renal failure.
Vd of ramipril – 90 l, ramiprilat – 500 l. 60% is excreted by the kidneys, 40% is excreted through the intestines (mainly in the form of metabolites). If renal function is impaired, the excretion of ramipril and its metabolites slows down in proportion to the decrease in CC; if liver function is impaired, the conversion to ramiprilat slows down; in heart failure, the concentration of ramiprilat increases by 1.5-1.8 times.
Special instructions
Special instructions
In patients with concomitant renal impairment, doses are selected individually in accordance with CC values. Before starting treatment, all patients must undergo a kidney function test.
During treatment with ramipril, renal function, blood electrolyte composition, levels of liver enzymes in the blood, as well as peripheral blood patterns are regularly monitored (especially in patients with diffuse connective tissue diseases, in patients receiving immunosuppressants, allopurinol).
Patients who have fluid and/or sodium deficiency must have their fluid and electrolyte imbalances corrected before starting treatment. During treatment with ramipril, hemodialysis should not be performed using polyacrylonitrile membranes (the risk of anaphylactic reactions is increased).
Active ingredient
Active ingredient
Ramipril
Composition
Composition
Active ingredient:
ramipril – 5 mg;
Excipients:
lactose monohydrate 143.5 mg,
magnesium stearate 1.5 mg.
Pregnancy
Pregnancy
Contraindicated for children under 18 years of age.
Contraindicated during pregnancy. Before starting treatment, you should make sure there is no pregnancy. If the patient becomes pregnant during treatment, it is necessary to replace drug therapy with ramipril with another therapy as soon as possible. Otherwise, there is a risk of fetal damage, especially in the first trimester of pregnancy.
Effect on the fetus: impaired development of the fetal kidneys, decreased blood pressure in the fetus and newborn, impaired renal function, hyperkalemia, cranial hypoplasia, oligohydramnios, limb contracture, cranial deformation, pulmonary hypoplasia.
FDA category of effect on the fetus is D.
Breastfeeding should be stopped during treatment.
Contraindications
Contraindications
severe renal and liver dysfunction, bilateral renal artery stenosis or stenosis of the artery of a single kidney;
condition after kidney transplantation;
primary hyperaldosteronism, hyperkalemia, aortic stenosis,
hypersensitivity to ramipril and other ACE inhibitors.
Side Effects
Side Effects
From the cardiovascular system and blood (hematopoiesis, hemostasis): hypotension (10.7%), incl. postural (2.2%), angina (2.9%), syncope (2.1%), heart failure (2%), myocardial infarction (1.7%), vertigo (1.5%), chest pain (1.1%), less than 1% – arrhythmia, palpitations, hemolytic anemia, myelodepression, pancytopenia, thrombocytopenia, eosinophilia, agranulocytosis; vasculitis
From the gastrointestinal tract: nausea (2.2%), vomiting (1.6%), diarrhea (1.1%), less than 1% – dry mouth or increased salivation, anorexia, dyspepsia, dysphagia, constipation, abdominal pain, gastroenteritis, pancreatitis, hepatitis, liver dysfunction (cholestatic jaundice, fulminant liver necrosis with fatal outcome), changes in the level of transaminases
From the nervous system and sensory organs: dizziness (4.1%), headache (1.2%), asthenia (0.3%), in less than 1% – cerebrovascular disorders, amnesia, drowsiness, convulsions, depression, sleep disorder, neuralgia, neuropathy, paresthesia, tremor, hearing loss, visual impairment.
From the respiratory system: nonproductive cough (7.6%), upper respiratory tract infections, in less than 1% – dyspnea, pharyngitis, sinusitis, rhinitis, tracheobronchitis, laryngitis, bronchospasm.
From the genitourinary system: impaired renal function (1.2%), in less than 1% – proteinuria, oliguria, edema; impotence.
From the skin: urticaria, prurigo, rash, erythema multiforme, photosensitivity.
Other: less than 1% – decreased body weight, anaphylactoid reactions, increased levels of urea nitrogen and creatinine, angioedema (0.3%), arthralgia/arthritis, myalgia, fever, increased titer of antinuclear antibodies, hyperkalemia, changes in enzyme activity, concentrations of bilirubin, uric acid, glucose.
Interaction
Interaction
With the simultaneous use of potassium-sparing diuretics (including spironolactone, triamterene, amiloride), potassium supplements, salt substitutes and dietary supplements containing potassium, hyperkalemia may develop (especially in patients with impaired renal function), because ACE inhibitors reduce the content of aldosterone, which leads to potassium retention in the body while limiting the excretion of potassium or its additional intake into the body.
When used simultaneously with NSAIDs, the hypotensive effect of ramipril may be reduced and renal function may be impaired.
When used simultaneously with loop or thiazide diuretics, the antihypertensive effect is enhanced. Severe arterial hypotension, especially after taking the first dose of a diuretic, appears to occur due to hypovolemia, which leads to a transient increase in the hypotensive effect of ramipril. There is a risk of developing hypokalemia. The risk of kidney dysfunction increases.
When used simultaneously with drugs that have a hypotensive effect, the hypotensive effect may be enhanced.
When used simultaneously with immunosuppressants, cystostatics, allopurinol, procainamide, the risk of developing leukopenia may increase.
When used simultaneously with insulin, hypoglycemic agents, sulfonylurea derivatives, and metformin, hypoglycemia may develop.
When used simultaneously with allopurinol, cystostatics, immunosuppressants, procainamide, the risk of developing leukopenia may increase.
When used simultaneously with lithium carbonate, it is possible to increase the concentration of lithium in the blood serum.
Overdose
Overdose
Symptoms: excessive peripheral vasodilation with the development of a pronounced decrease in blood pressure, shock; bradycardia, fluid and electrolyte disturbances, acute renal failure, stupor.
Treatment: gastric lavage, taking adsorbents, sodium sulfate (if possible within the first 30 minutes). In the case of a pronounced decrease in blood pressure, the administration of alpha1-adrenergic agonists (norepinephrine, dopamine) can be added to therapy to replenish circulating blood volume and restore electrolyte balance. In case of bradycardia refractory to drug treatment, installation of a temporary artificial pacemaker may be required. In case of overdose, it is necessary to monitor serum concentrations of creatinine and electrolytes.
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C
Shelf life
Shelf life
3 years.
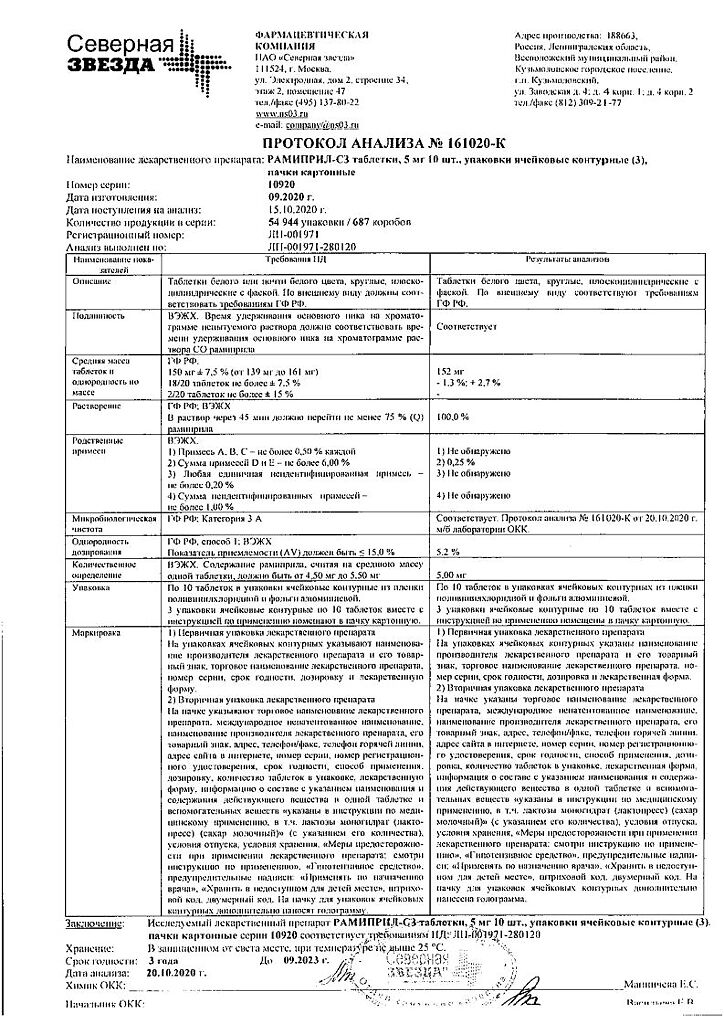
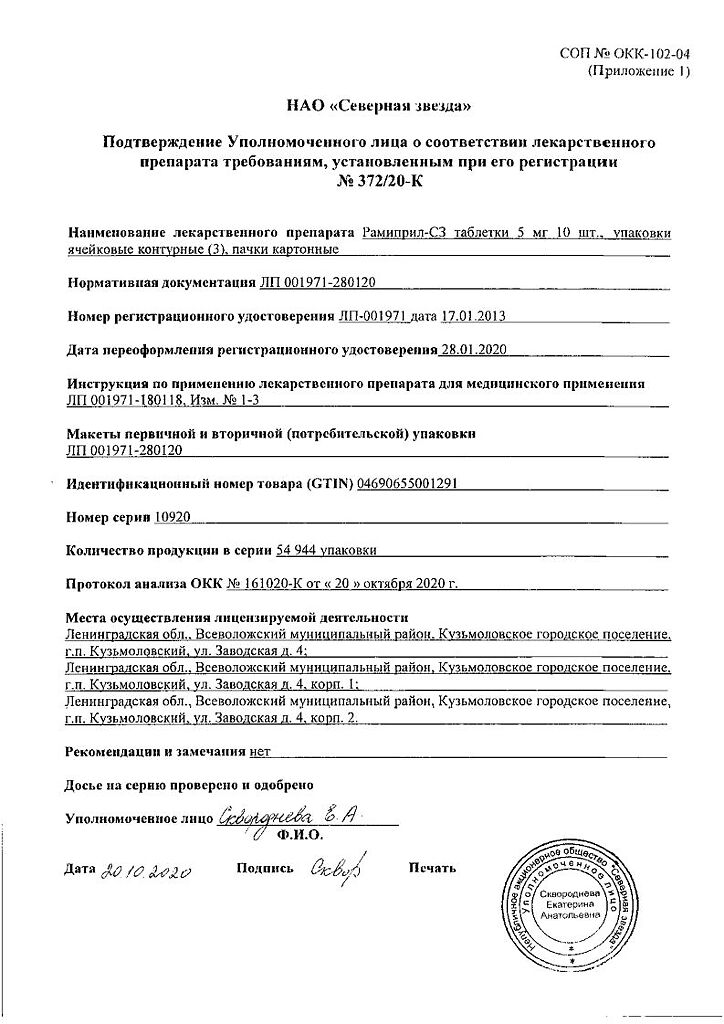
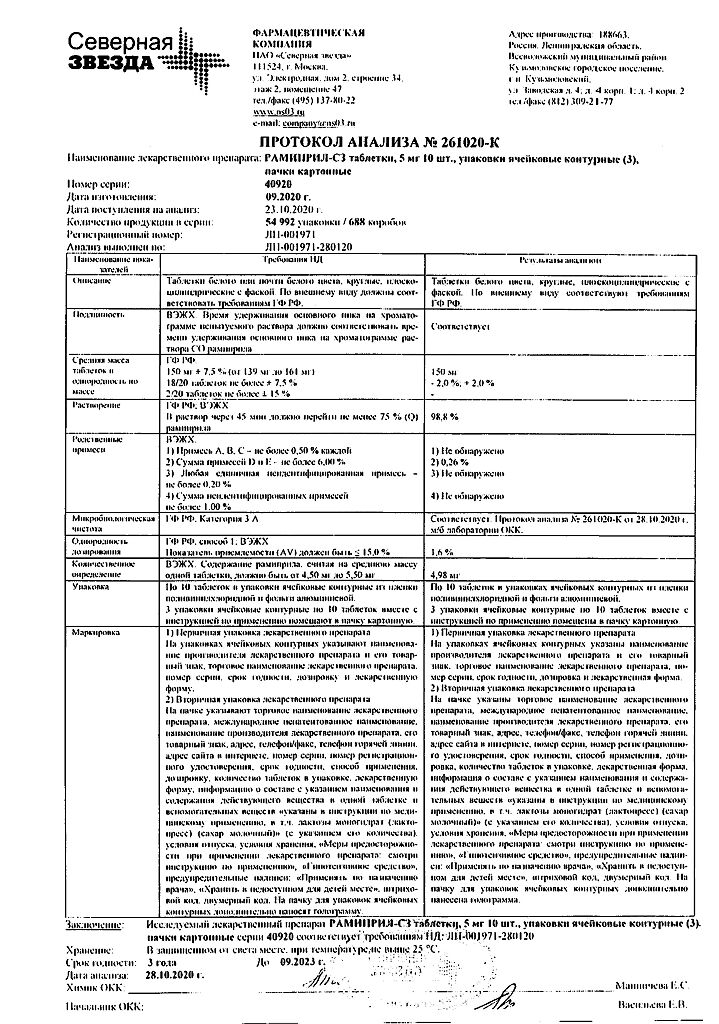
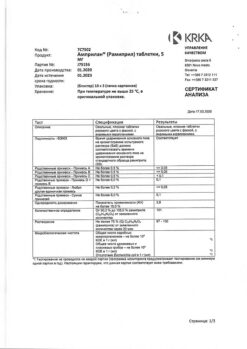
Manufacturer
Manufacturer
North Star NAO, Russia
Additional information
| Shelf life | 3 years. |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C |
| Manufacturer | North Star NAO, Russia |
| Medication form | pills |
| Brand | North Star NAO |
Other forms…
Related products
Buy Ramipril-SZ, tablets 5 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.