No products in the cart.
Ramipril-Acrihin, tablets 2.5mg 30 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group: angiotensin-converting enzyme (ACE) inhibitor
ATX code: C09AA05
Pharmacological properties
Pharmacodynamics
The active metabolite of ramipril formed under the influence of “hepatic” enzymes – ramiprilat is a long-acting ACE inhibitor (synonyms ACE: kininase II, dipeptidylcarboxydipeptidase I), which is a peptidyl dipeptidase. ACE in blood plasma and tissues catalyzes the conversion of angiotensin I into angiotensin II, which has a vasoconstrictor effect, and the breakdown of bradykinin, which has a vasodilator effect.
Therefore, when ramipril is taken orally, angiotensin II formation is reduced and bradykinin accumulates, resulting in vasodilatation and a decrease in blood pressure (BP). Increase of kallikrein-kinin system activity in blood and tissues caused by ramipril with prostaglandin system activation and increase of prostaglandins synthesis, stimulating nitric oxide formation in endotheliocytes, determines its cardioprotective and endothelioprotective action. Angiotensin II stimulates production of aldosterone, therefore administration of ramipril leads to decrease of aldosterone secretion and increase of serum potassium ions content.
When the concentration of angiotensin II in blood decreases, its inhibitory effect on renin secretion by negative feedback is eliminated, resulting in increased plasma renin activity.
It is assumed that development of some adverse events (in particular “dry” cough) is also associated with increased bradykinin activity.
In patients with arterial hypertension, administration of ramipril leads to a decrease in BP in the supine and standing position, without a compensatory increase in heart rate (HR). Ramipril significantly reduces total peripheral vascular resistance (TPR) with little or no change in renal blood flow and glomerular filtration rate. Antihypertensive effect begins to develop 1-2 hours after oral administration of a single dose of the drug, reaching its maximum value after 3-6 hours and remaining within 24 hours. When ramipril is taken as a course, the antihypertensive effect may gradually increase, stabilizing usually by 3-4 weeks of regular drug intake and then remaining for a long time. Sudden discontinuation of the drug does not lead to a rapid and significant increase in BP (no “withdrawal” syndrome),
In patients with arterial hypertension, ramipril slows the development and progression of myocardial and vascular wall hypertrophy.
In patients with chronic heart failure, ramipril decreases PEEP (decreases afterload on the heart), increases venous system capacity and decreases left ventricular filling pressure, which consequently leads to a decrease in cardiac preload. In these patients, taking ramipril increases cardiac output, ejection fraction and improves exercise tolerance. In diabetic and nondiabetic nephropathy, ramipril slows the rate of progression of renal failure and time to the end stage of renal failure and thus reduces the need for hemodialysis or renal transplantation. In the initial stages of diabetic or nondiabetic nephropathy, ramipril reduces the incidence of albuminuria.
. In patients at high risk of cardiovascular disease due to vascular lesions (diagnosed coronary heart disease, history of peripheral arterial obliterative disease, history of stroke) or diabetes with at least one additional risk factor (microalbuminuria, arterial hypertension, increased concentration of total cholesterol (TC), decreased concentration of high-density lipoprotein cholesterol (HDL-C), smoking) the addition of ramipril to standard therapy significantly reduces the incidence of myocardial infarction, stroke and mortality from cardiovascular diseases. In addition, ramipril reduces overall mortality and the need for revascularization procedures and slows the onset or progression of chronic heart failure.
. In patients with heart failure and clinical manifestations that developed during the first days of acute myocardial infarction (days 2-9), ramipril started on days 3 to 10 of acute myocardial infarction reduced mortality (by 27%), risk of sudden death (by 30%), risk of progression of heart failure to severe (NYHA functional class III-IV)/resistant to therapy (by 23%), and likelihood of subsequent hospitalization due to development of heart failure (by 26%).
In the general patient population, as well as in patients with diabetes mellitus with both arterial hypertension and normal BP, ramipril significantly reduces the risk of nephropathy and microalbuminuria.
Pharmacokinetics
Ramipril is rapidly absorbed from the gastrointestinal tract after oral administration (50 to 60%). Simultaneous intake of food slows its absorption, but does not affect the completeness of absorption. Ramipril undergoes intensive presystemic metabolism/activation (mainly in the liver by hydrolysis), as a result of which its only active metabolite is formed – ramiprilat, which activity with respect to ACE inhibition is approximately 6 times higher than activity of ramipril. In addition, as a result of metabolism of ramipril, diketopiperazine is formed, which does not have pharmacological activity, which then undergo conjugation with glucuronic acid; ramiprilat is also glucuronized and metabolized to diketopiperazine acid.
All formed metabolites, except for ramiprilat, have no pharmacological activity.
The bioavailability of ramipril after oral administration ranges from 15% (for 2.5 mg dose) to 28% (for 5 mg dose). The bioavailability of the active metabolite, ramiprilate, after oral administration of 2.5 mg and 5 mg ramipril is approximately 45% (compared to its bioavailability after intravenous administration in the same doses).
After oral administration of ramipril, maximum plasma concentrations of ramipril and ramiprilate are reached after 1 and 2-4 hours, respectively. The decrease in plasma concentration of ramiprilat occurs in several phases: a distribution and excretion phase with a half-life (T1/2) of ramiprilat of approximately 3 hours, then an intermediate phase with a T1/2 of ramiprilat of approximately 15 hours, and a final phase with a very low plasma concentration of ramiprilat and a T1/2 of ramiprilat of approximately 4-5 days.
This end phase is due to the slow release of ramiprilat from strong binding to ACE receptors. Despite this prolonged end phase, when ramipril is taken daily at a single oral dose of 2.5 mg or more, the equilibrium plasma concentration of ramiprilat is reached after approximately 4 days of treatment. When using the drug in a course, the “effective” T1/2 is 13 to 17 hours depending on the dose.
The binding to plasma proteins is approximately 73% for ramipril and 56% for ramiprilat.
After intravenous administration, the volume of distribution of ramipril and ramiprilat is approximately 90 L and approximately 500 L, respectively.
After intravenous administration of radioactive isotope-labeled ramipril (10 mg), 39% of the radioactivity is excreted through the intestine and about 60% by the kidneys. After intravenous administration of ramipril, 50-60% of the dose is detected in the urine as ramipril and its metabolites. After intravenous administration of ramiprilat about 70% of the dose is detected in the urine as ramiprilat and its metabolites, in other words, when ramipril and ramiprilat are administered intravenously, a significant part of the dose is excreted through the intestine with the bile, bypassing the kidneys (50% and 30%, respectively). After oral administration of 5 mg of ramipril in patients with bile duct drainage, almost equal amounts of ramipril and its metabolites are excreted by the kidneys and through the intestine during the first 24 hours after administration.
About 80-90% of metabolites in urine and bile have been identified as ramipril and ramiprilate metabolites. Ramipril glucuronide and ramipril diketopiperazine account for approximately 10-20% of the total, and the urinary content of unmetabolized ramipril is approximately 2%.
In animal studies, ramipril has been shown to be excreted in maternal milk.
In impaired renal function with a creatinine clearance (CK) of less than 60 ml/min, excretion of ramiprilat and its metabolites by the kidneys is delayed. This leads to increased plasma concentration of ramiprilat, which decreases more slowly than in patients with normal renal function.
When taking ramipril at high doses (10 mg), impaired liver function leads to slower presystemic metabolism of ramipril to active ramiprilate and slower excretion of ramiprilate.
In healthy volunteers and in patients with arterial hypertension after two weeks of treatment with ramipril at a daily dose of 5 mg, there is no clinically significant accumulation of ramipril and ramiprilat.
In patients with chronic heart failure after two weeks of treatment with ramipril at a daily dose of 5 mg there is a 1.5-1.8-fold increase in plasma concentrations of ramiprilat and area under the pharmacokinetic curve “concentration-time” (AUC).
In healthy elderly volunteers (65-76 years), the pharmacokinetics of ramipril and ramiprilat are not significantly different from those of younger healthy volunteers.
Indications
Indications
Active ingredient
Active ingredient
How to take, the dosage
How to take, the dosage
Interaction
Interaction
Contraindicated combinations
The use of certain high-flow membranes with a negatively charged surface (e.g. polyacrylonitrile membranes) in hemodialysis or hemofiltration; the use of dextran sulfate in low-density lipoprotein apheresis.
The risk of severe anaphylactoid reactions. If the patient needs these procedures, other types of membranes should be used (in case of plasmapheresis and hemofiltration) or the patient should be transferred to other groups of hypotensive drugs.
The concomitant use of Ramipril and drugs containing aliskiren
The concomitant use of Ramipril and drugs containing aliskiren in patients with diabetes or moderate to severe renal impairment with a creatinine clearance of < 60 ml/min is contraindicated and not recommended in other patients (see See Sections “Contraindications”, “Caution”, “Special Precautions”).
The concomitant use of Ramipril and angiotensin II receptor antagonists (ARA II)
The concomitant use of the drug and ARA II in patients with diabetic nephropathy is contraindicated and not recommended in other patients (see “Contraindications”, “Caution”, “Special Precautions”).
Unrecommended combinations
With potassium salts, potassium-saving diuretics (e.g., amiloride, triamterene, spironolactone, eplerenone), other drugs that can increase serum potassium levels (including ARA II, tacrolimus, cyclosporine, trimethoprim, sulfamethoxazole as part of cotrimoxazole (a combined antibacterial drug containing sulfamethoxazole and trimethoprim)).
There may be an increase in serum potassium, sometimes significantly pronounced (with concomitant use requires close monitoring of serum potassium).
Combinations to be used with caution
With hypotensive drugs (e.g., diuretics) and other drugs that can reduce BP (nitrates, tricyclic antidepressants, agents for general and local anesthesia, baclofen, alfuzosin, doxazosin, prazosin, tamsulosin, terazosin) – potentiation of the antihypertensive effect; when combining with diuretics, serum sodium should be monitored regularly.
With sleeping pills, narcotic and analgesic drugs – possible more pronounced BP reduction.
With vasopressor sympathomimetics (epinephrine (adrenaline), isoproterenol, dobutamine, dopamine) – reduction of the antihypertensive effect of Ramipril, particularly close control of BP is recommended.
With allopurinol, procainamide, cytostatics, immunosuppressants, corticosteroids (glucocorticosteroids and mineralocorticosteroids) and other drugs that may affect hematological parameters – combined use increases the risk of hematological reactions.
With lithium salts – increased serum lithium concentration and increased cardio- and neurotoxic effects of lithium. Therefore, serum lithium content should be monitored.
With hypoglycemic agents (e.g., insulin, hypoglycemic agents for oral administration (sulfonylurea derivatives, biguanides) – due to a decrease in insulin resistance under the influence of ACE inhibitors, the hypoglycemic effect of these drugs may increase, up to the development of hypoglycemia. We recommend especially careful monitoring of blood glucose concentration at the beginning of their combined use with ACE inhibitors.
With type IV dipeptidyl peptidase inhibitors (DPP-IV) (glyptins) such as sitagliptin, saxagliptin, vildagliptin, linagliptin – in patients who took ACE inhibitors and glyptins simultaneously, there was an increased frequency of angioedema development.
With racecadotril (an enkephalinase inhibitor used to treat acute diarrhea) – an increased risk of angioedema.
With estramustine – increased risk of angioedema.
With mTOR inhibitors (mammalian Target of Rapamycin in mammalian cells) such as temsirolimus, sirolimus, everolimus – an increased incidence of angioedema was observed in patients who took ACE inhibitors and mTOR inhibitors simultaneously.
Combinations to consider
With nonsteroidal anti-inflammatory drugs (indomethacin, acetylsalicylic acid (more than 3 g/day) – the effects of ramipril, increased risk of renal dysfunction and increased serum potassium may be impaired.
With heparin, serum potassium may increase.
With sodium chloride – weakening of the antihypertensive effect of the drug and less effective treatment of symptoms of chronic heart failure.
With ethanol – increase the symptoms of vasodilation. The drug may increase the effect of ethanol on the body.
With estrogens – weakening of the antihypertensive effect of ramipril (fluid retention).
Desensitizing therapy in hypersensitivity to insect venoms – ACE inhibitors, including the drug Ramipril, increase the likelihood of severe anaphylactic or anaphylactoid reactions to insect venoms. It has been suggested that this effect may also occur with other allergens.
Special Instructions
Special Instructions
Hyponatremia and hypovolemia should be eliminated before initiating treatment with Ramipril. In patients who have previously taken diuretics, they should be discontinued or at least their dose should be reduced 2-3 days before starting Ramipril (in this case the state of patients with chronic heart failure should be carefully monitored due to the possibility of decompensation in patients with increased circulating blood volume).
After the first dose of the drug, as well as when increasing the dose and/or the dose of diuretics (especially loop diuretics), the patient should be closely monitored for at least 8 hours to ensure timely appropriate measures are taken in case of excessive BP decrease.
If Ramipril is used for the first time or at a high dose in patients with increased RAAS activity, their BP should be monitored carefully, especially at the beginning of treatment, as these patients have an increased risk of excessive BP reduction (see Caution).
In malignant arterial hypertension and heart failure, particularly in the acute stage of myocardial infarction, treatment with Ramipril should only be initiated in a hospital setting.
In patients with chronic heart failure, administration of the drug may lead to marked BP decrease, which in some cases is accompanied by oliguria or azotemia and rarely by development of acute renal failure.
Caution should be exercised when treating elderly patients because they may be particularly sensitive to ACE inhibitors, and monitoring of renal function parameters is recommended in the initial phase of treatment (see also section “Dosage and administration”).
In patients for whom decreased BP may pose some risk (e.g., patients with atherosclerotic narrowing of coronary or cerebral arteries), treatment should be initiated under close medical supervision.
Cautions should be taken during physical activity and/or hot weather because of the risk of increased sweating and dehydration with the development of arterial hypotension, due to decreased circulating blood volume and decreased sodium content in the blood.
Alcohol (ethanol) should not be consumed during treatment with Ramipril.
A transient excessive decrease in BP is not a contraindication to continue treatment after BP stabilization. If a significant decrease in BP develops again, the dose should be reduced or the drug should be discontinued.
The concomitant use of Ramipril with drugs containing aliskiren or with ARA II resulting in dual RAAS blockade is not recommended due to the risk of excessive BP decrease, development of hyperkalemia and impaired renal function compared to monotherapy. Simultaneous use of Ramipril with drugs containing aliskiren in patients with diabetes mellitus and/or moderate to severe renal impairment with creatinine clearance < 60 ml/min is contraindicated (see
Simultaneous use with APA II in patients with diabetic nephropathy is contraindicated (see “Contraindications” and “Interaction with other medicinal products”) and is not recommended in other patients.
In patients treated with ACE inhibitors, there have been cases of angioedema of the face, extremities, lips, tongue, pharynx, or larynx. If swelling of the face (lips, eyelids) or tongue, or impaired swallowing or breathing occurs, the patient should immediately stop taking the drug. Angioedema localized in the region of the tongue, pharynx or larynx (possible symptoms: impaired swallowing or breathing) may be life-threatening and requires urgent measures to control it: subcutaneous injection of 0.3-0.5 mg or intravenous drip injection of 0.1 mg of epinephrine (adrenaline) (under control of BP, HR and ECG) followed by glucocorticosteroids (IV, IV/m or oral); intravenous administration of antihistamines (H1 and H2-histamine receptor antagonists) is also recommended, and if C1-esterase inactivators are insufficient, the need for C1-esterase enzyme inhibitors in addition to epinephrine (adrenaline) may be considered.
The patient should be hospitalized and monitored until symptoms have resolved, but not less than 24 h.
Patients receiving ACE inhibitors have had cases of intestinal angioedema manifested by abdominal pain with or without nausea and vomiting; in some cases facial angioedema has also been observed. If patients present with these symptoms after treatment with ACE inhibitors, the possibility of intestinal angioedema should be considered in the differential diagnosis.
Treatment with desensitization to insect venom (e.g., bees, wasps) and simultaneous administration of ACE inhibitors can initiate anaphylactic and anaphylactoid reactions (e.g., BP decrease, shortness of breath, vomiting, allergic skin reactions), which can sometimes be life threatening. During treatment with ACE inhibitors, hypersensitivity reactions to insect venom (such as bees, wasps) develop faster and are more severe. If desensitization to insect venom is necessary, the ACE inhibitor should be temporarily replaced by the appropriate drug of another group.
Life-threatening, rapidly developing anaphylactoid reactions, sometimes up to shock, have been described with ACE inhibitors during hemodialysis or plasmafiltration using certain high-flow membranes (e.g. polyacrylonitrile membranes) (see also membrane manufacturer instructions). The combined use of Ramipril and these types of membranes, e.g. for emergency hemodialysis or hemofiltration, should be avoided. In this case, the use of other types of membranes or exclusion of ACE inhibitors is preferable. Similar reactions have been observed with low-density lipoprotein apheresis using dextran sulfate. Therefore, this method should not be used in patients receiving ACE inhibitors.
In patients with impaired liver function, the response to treatment with Ramipril may be either enhanced or impaired. In addition, in patients with severe cirrhosis with edema and/or ascites, significant activation of the RAAS is possible; therefore, special caution should be exercised when treating these patients (see also section “Dosage and administration”).
Before surgical intervention (including dental), the surgeon/anesthesiologist should be warned about taking ACE inhibitors.
It is recommended that neonates who have had intrauterine exposure to ACE inhibitors be closely monitored for arterial hypotension, oliguria, and hyperkalemia.
In oliguria, BP and renal perfusion should be maintained by administration of appropriate fluids and vasoconstrictors. These newborns are at risk of oliguria and neurological disorders, possibly due to decreased renal and cerebral blood flow due to the decrease in BP caused by ACE inhibitors.
Monitor laboratory parameters before and during treatment with Ramipril up to once a month during the first 3-6 months of treatment.
Management of renal function (determination of serum creatinine concentrations)
In treatment with ACE inhibitors, renal function monitoring is recommended in the first weeks of treatment and thereafter. Especially close monitoring is required in patients with acute and chronic heart failure, impaired renal function, after renal transplantation, patients with renovascular disease including patients with hemodynamically significant unilateral renal artery stenosis in patients with two kidneys (in these patients even a slight increase of serum creatinine concentration may be an indication of reduced renal function).
Control of electrolytes
The regular monitoring of serum potassium and sodium is recommended. Especially close monitoring of serum potassium is required in patients with impaired renal function, significant electrolyte-water balance disorders, and chronic heart failure.
Control of hematologic parameters (hemoglobin, number of leukocytes, erythrocytes, platelets, leukocytic formula)
Control of general blood counts is recommended to detect possible leukopenia. More regular monitoring is recommended at the beginning of treatment and in patients with impaired renal function, as well as in patients with connective tissue diseases or in patients receiving simultaneously other drugs which may alter the peripheral blood count (see section “Interaction with other medicinal products”). Control of leukocyte count is necessary for early detection of leukopenia, which is especially important in patients at high risk of its development, as well as at the first signs of infection. In case of detection of neutropenia (neutrophil count is less than 2000/μL), discontinuation of treatment with ACE inhibitors is required.
In case of symptoms associated with leukopenia (e.g., fever, enlarged lymph nodes, tonsillitis), immediate monitoring of peripheral blood counts is necessary. If there are signs of bleeding (tiny petechiae, reddish-brown rashes on skin and mucous membranes), peripheral blood platelet counts should also be monitored.
Determination of “hepatic” enzyme activity, bilirubin concentration in blood
If jaundice or significant increase in “hepatic” enzyme activity occurs, the drug should be stopped and the patient should be under medical monitoring.
When using the drug, caution should be exercised when driving motor vehicles and engaging in other potentially hazardous activities requiring increased concentration and rapid psychomotor reactions (dizziness is possible, especially after the initial dose of ACE inhibitor in patients taking diuretic drugs).
Contraindications
Contraindications
Side effects
Side effects
Overdose
Overdose
Pregnancy use
Pregnancy use
Similarities
Similarities
Additional information
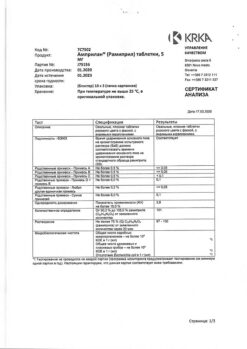
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | In the dark place at a temperature not exceeding 25 ° C. Keep out of reach of children. |
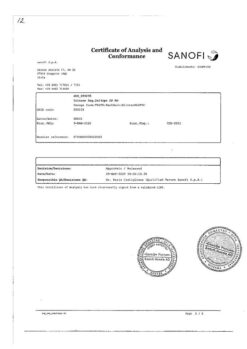
| Manufacturer | Akrihin HFC JSC, Russia |
| Medication form | pills |
| Brand | Akrihin HFC JSC |
Other forms…
Related products
Buy Ramipril-Acrihin, tablets 2.5mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.