No products in the cart.
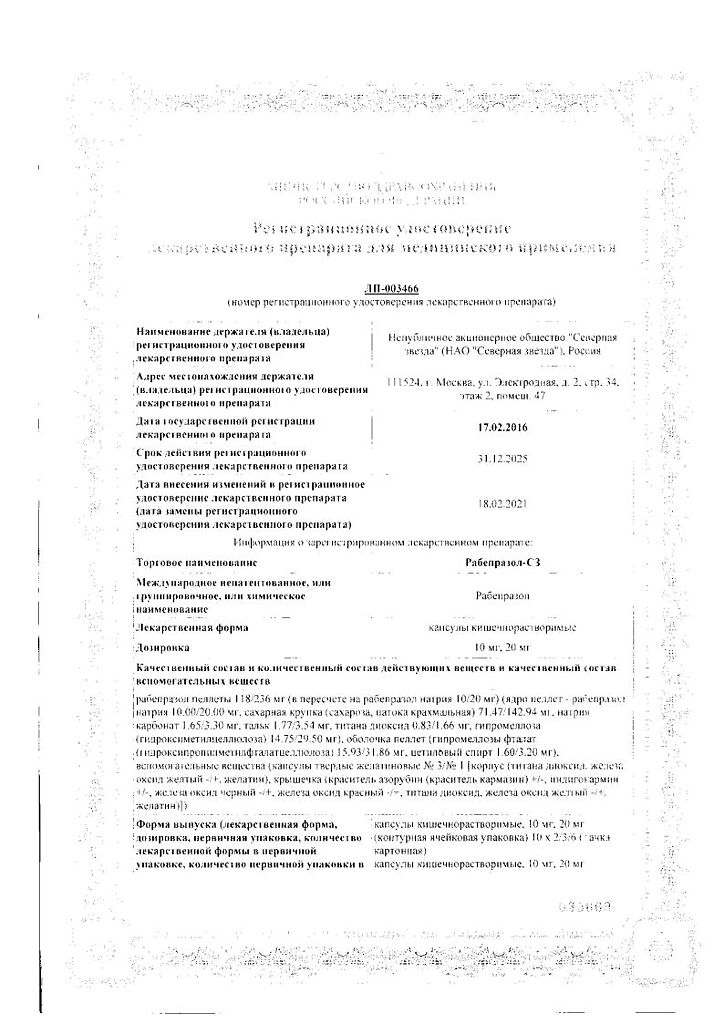
Rabeprazole-SZ, 10 mg 28 pcs
€6.49 €5.68
EAN: 4690655015441
SKU: 275778
Categories: Medicine, Stomach, intestines, liver, Ulcer and gastritis
Description
Pharmacotherapeutic group
A gastric gland secretion reducing agent – proton pump inhibitor
ATX code: [A02BC04]
Pharmacological properties
Pharmacodynamics
Rabeprazole belongs to the class of antisecretory agents, benzimidazole derivatives. Suppresses gastric juice secretion by specific inhibition of H+ /K+ -ATPase on the secretory surface of the parietal cells of the stomach. Blocks the final stage of hydrochloric acid secretion, reducing basal and stimulated secretion, regardless of the nature of the stimulus.
With high lipophilicity easily penetrates into the parietal cells of the stomach, concentrates in them, exerting cytoprotective effect and increasing the secretion of hydrocarbonate. Anti-secretory action after oral administration of 20 mg of rabeprazole, occurs within 1 hour and reaches a maximum after 2-4 hours; inhibition of basal and food-stimulated acid secretion after 23 hours after the first dose is 62 and 82%, respectively, and lasts up to 48 hours.
When discontinued, secretory activity is restored within 1-2 days. During the first 2-8 weeks of therapy with rabeprazole, plasma gastrin concentration increases, (which is a reflection of the inhibitory effect on hydrochloric acid secretion) and returns to initial levels 1-2 weeks after its withdrawal.
Rabeprazole has no anticholinergic properties, does not affect the central nervous system (CNS), cardiovascular and respiratory systems. No sustained changes in morphological structure of enterochromaffin-like cells, in severity of gastritis, in frequency of atrophic gastritis, intestinal metaplasia or spread of Helicobacter pylori infection were found during rabeprazole administration.
Pharmacokinetics
Absorption
Rabeprazole is rapidly absorbed from the gut, and its maximum plasma concentrations are reached approximately 3.5 h after a dose of 20 mg. Changes of maximum plasma concentrations (Cmax) and values of area under the curve “concentration-time” (AUC) of rabeprazole are linear in the dose range from 10 to 40 mg.
The absolute bioavailability after oral administration of 20 mg (compared to intravenous administration) is about 52%. Moreover, bioavailability does not change with repeated administration of rabeprazole. In healthy volunteers, the plasma elimination half-life is about 1 h (varying from 0.7 to 1.5 h) and total clearance is 3.8 ml/min/kg.
In patients with chronic liver damage, the AUC is doubled compared to healthy volunteers, indicating decreased first-pass metabolism, and the plasma elimination half-life is 2 to 3 times longer. Neither the time of intake of the drug during a day, nor antacids affect absorption of rabeprazole. Taking the drug with a fatty food slows down absorption of rabeprazole by 4 hours or more, but neither Cmax nor degree of absorption is changed.
Distribution
In humans the degree of binding of rabeprazole to plasma proteins is about 97%.
Metabolism and excretion
In healthy subjects
After a single oral dose of 20 mg of 14C-labeled rabeprazole, no unchanged drug was found in the urine. About 90% of rabeprazole is excreted in the urine primarily as two metabolites: mercapturic acid conjugate (M5) and carboxylic acid (M6), and in the form of two unknown metabolites identified in the toxicological analysis.
The remainder of rabeprazole taken is excreted in the feces. The total excretion is 99.8%. These data indicate small excretion of rabeprazole metabolites with bile. The main metabolite is thioether (M1). The only active metabolite is desmethyl (M3), but it was observed in low concentration only in one study participant after administration of 80 mg of rabeprazole.
Terminal renal failure
In patients with stable, terminal renal failure who require maintenance hemodialysis (creatinine clearance < 5 ml/min/1.73m2 ), excretion of rabeprazole is similar to that in healthy volunteers. The AUC and Cmax in these patients were approximately 35% lower than in healthy volunteers.
The mean half-life of rabeprazole was 0.82 h in healthy volunteers, 0.95 h in patients during hemodialysis and 3.6 h after hemodialysis. Clearance of the drug in patients with kidney disease requiring hemodialysis was approximately twice as high as in healthy volunteers.
Chronic compensated cirrhosis
Patients with chronic compensated cirrhosis tolerate rabeprazole at a dose of 20 mg once daily, although AUC is doubled and Cmax is increased by 50% compared to healthy volunteers of the respective sex.
Elderly patients
The elimination of rabeprazole is somewhat delayed in elderly patients. After 7 days of taking rabeprazole at 20 mg per day, the AUC was approximately twice as high and the Cmax was increased by 60% in elderly patients compared to young healthy volunteers. However, no evidence of rabeprazole cumulation was observed.
CYP2C19 polymorphism
In patients with delayed CYP2C19 metabolism, after 7 days of taking rabeprazole at a dose of 20 mg daily, the AUC increased 1.9-fold and the elimination half-life 1.6-fold compared to the same parameters in “fast metabolizers”, while the Cmax increased by 40%.
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
1 capsule contains:
The active ingredient:
rabeprazole pellets – 118 mg, 236 mg
calculated to rabeprazole sodium – 10 mg, 20 mg
[pellet core: Rabeprazole sodium – 10.00 mg, 20.00 mg, sugar grits (sucrose, starch treacle) – 71.47 mg, 142.94 mg, sodium carbonate – 1.65 mg, 3.30 mg, talc – 1.77 mg, 3.54 mg, titanium dioxide – 0.83 mg, 1.66 mg, hypromellose (hydroxymethylcellulose) – 14.75 mg, 29.50 mg;
Pellet shell:
Hypromellose phthalate (hydroxypropyl methylphthalate cellulose)- 15.93 mg, 31.86 mg, cetyl alcohol 1.60 mg, 3.20 mg].
Auxiliary substances:
Capsules hard gelatin #3 (dosage 10 mg):
corp:
titanium dioxide, 2.0%, gelatin, up to 100%;
cup:
dye azorubin (carmazine dye) – 0.6619%, indigo carmine – 0.0286%, titanium dioxide – 0.6666%, gelatin – up to 100%.
Capsules hard gelatin No. 1 (dosage 20 mg):
casing:
titanium dioxide – 1.0%, iron oxide yellow – 0.192% gelatin – up to 100%;
cup:
iron oxide black – 0.53%, iron oxide red – 0.93%, titanium dioxide – 0.3333%, iron oxide yellow – 0.20%, gelatin – up to 100%.
How to take, the dosage
How to take, the dosage
Capsules of Rabeprazole-SZ should be swallowed whole. It has been established that neither time of day nor food intake affect the activity of rabeprazole. In acute gastric ulcer and anastomosis ulcer it is recommended to take orally 10 mg or 20 mg once daily.
Cure usually occurs after 6 weeks of therapy, but in some cases the duration of treatment may be extended for an additional 6 weeks.
In case of duodenal ulcer in the acute stage it is recommended to take orally 20 mg once a day. In some cases the therapeutic effect occurs when taking 10 mg once a day. Treatment duration is from 2 to 4 weeks. If necessary, the duration of treatment may be increased for 4 more weeks.
In treatment of erosive gastroesophageal reflux disease (GERD) or reflux esophagitis, it is recommended to take orally 10 mg or 20 mg once daily. The duration of treatment is 4 to 8 weeks. If necessary, the duration of treatment may be increased for 8 more weeks.
In maintenance therapy of gastroesophageal reflux disease (GERD), it is recommended to take orally 10 mg or 20 mg once daily. The duration of treatment depends on the patient’s condition.
If after four weeks of treatment the symptoms do not disappear, the patient should be further investigated. Once symptoms have resolved, oral doses of 10 mg once daily should be taken on demand to prevent further onset of symptoms.
To treat Zollinger-Ellison syndrome and other conditions characterized by pathological hypercemia, the dose is adjusted individually.
The starting dose is 60 mg per day, and then the dose is increased to 100 mg per day on a single dose or 60 mg twice a day. For some patients, fractional dosing is preferable. Treatment should be continued as clinically necessary. In some patients with Zollinger-Ellison syndrome, the duration of treatment with rabeprazole was up to one year.
For eradication of Helicobacter pylori it is recommended to take orally 20 mg 2 times a day according to a certain scheme with an appropriate combination of antibiotics. The duration of treatment is 7 days.
Patients with renal and hepatic insufficiency No dose adjustment is required in patients with renal insufficiency. In patients with mild to moderate hepatic impairment the concentration of rabeprazole in blood is usually higher than in healthy volunteers.
Patients with severe hepatic impairment should be treated with caution when prescribing Rabeprazole-SZ. No dosage adjustment is required in elderly patients.
Children
The safety and efficacy of [eabeprazole 20 mg for short-term (up to 8 weeks) treatment of GERD in children aged 12 years and older has been confirmed by extrapolation of adequate and well-controlled studies supporting the efficacy of rabeprazole for adults and by safety and pharmacokinetics studies for pediatric patients. The recommended dose for children aged 12 years and older is 20 mg once daily for up to 8 weeks.
Interaction
Interaction
Delays excretion of some drugs metabolized in the liver by microsomal oxidation (diazepam, phenytoin, indirect anticoagulants).
The co-administration of rabeprazole with ketoconazole or itraconazole may lead to a significant decrease in plasma concentrations of antifungal drugs.
The co-administration of proton pump inhibitors (PPIs) with atanazavir is not recommended because the effects of atanazavir are significantly reduced. Rabeprazole inhibits the metabolism of cyclosporine.
Concomitant administration of PPIs and methotrexate suggests increased concentrations of the latter and/or its metabolite hydroxytrexate and increased elimination half-life.
Special Instructions
Special Instructions
Patient response to therapy with rabeprazole does not exclude the presence of malignant neoplasms in the stomach.
The Rabeprazole-SZ capsules should be swallowed whole. It has been found that neither the time of day nor food intake affects the activity of rabeprazole.
In a specific study in patients with mild to moderate liver dysfunction, no significant difference in the incidence of side effects of Rabeprazole-SZ was found compared to that in gender- and age-matched healthy subjects, but despite this, caution is recommended when first prescribing Rabeprazole-SZ in patients with severe liver dysfunction.
Patients with impaired renal or hepatic function do not require dose adjustment of Rabeprazol-SZ. The AUC of rabeprazole in patients with severe hepatic impairment is approximately twice as high as in healthy patients.
Hypomagnesemia
In treatment with PPIs for at least 3 months, cases of symptomatic or asymptomatic hypomagnesemia have rarely been reported. Most of these cases were reported one year after therapy.
Serious adverse events were tetany, arrhythmias, and seizures. Most patients required treatment for hypomagnesemia, which included magnesium replacement and withdrawal of PPI therapy. In patients who will receive long-term treatment or who take PPIs with drugs such as digoxin or drugs that can cause hypomagnesemia (such as diuretics), health care providers should monitor magnesium levels before starting PPI treatment and during treatment. Fractures
PPPI therapy may lead to an increased risk of osteoporosis-related fractures of the hip, wrist, or spine. The risk of fractures was increased in patients who received high-dose PPIs for a long time (one year or more).
The concomitant use of rabeprazole with methotrexate
According to the literature, concomitant use of PPIs with methotrexate (especially in high doses), can lead to increased concentration of methotrexate and/or its metabolite hydroxytetrexate and increase the elimination half-life, which may lead to methotrexate toxicity. If high doses of methotrexate are necessary, temporary discontinuation of PPI therapy may be considered.
Infections caused by Salmonella, Campylobacter and Clostridium difficile. PPI therapy may lead to an increased risk of gastrointestinal infections such as those caused by Salmonella, Campylobacter and Clostridium difficile.
The effect on the ability to drive and operate machinery.
Based on peculiarities of pharmacodynamics of rabeprazole and its profile of adverse effects, it is unlikely that Rabeprazole-SZ influences the ability to drive and operate machinery. However, in case of drowsiness, these activities should be avoided.
Synopsis
Synopsis
Solid gelatin capsules â 3, the body color white with a cap of dark red (for dosage of 10 mg); hard gelatin capsules â 1, the body color yellow with a cap of brown (for dosage of 20 mg).
The contents of the capsules are spherical pellets from almost white to white with a creamy or yellowish tint.
Contraindications
Contraindications
Side effects
Side effects
In clinical trials, the following adverse reactions have been reported when taking rabeprazole: headache, dizziness, asthenia, abdominal pain, diarrhea, flatulence, dry mouth, rash.
The adverse reactions are classified according to the WHO Classification:
Very common (>1/10);
Frequent (>1/100, < 1/10);
Infrequently (> 1/1000, < 1/100);
Rarely (> 1/10000, < 1/1000);
Very rare (< 1/10000);
Frequency unknown (impossible to determine based on available data). Immune system disorders: rare – acute systemic allergic reactions (including facial edema, hypotension, shortness of breath).
With the blood and lymphatic system: rare – thrombocytopenia, neutropenia, leukopenia.
As to metabolism and nutrition: rare – anorexia; frequency is unknown – hyponatremia, hypomagnesemia.
Nervous system: frequent – insomnia, headache, dizziness; infrequent – drowsiness, nervousness; rare – depression; frequency unknown – confusion.
An organ of vision: rarely – visual impairment.
Vascular disorders: frequency unknown – peripheral edema.
Respiratory system: frequent – cough, pharyngitis, rhinitis; infrequent – sinusitis, bronchitis.
The digestive system: often – abdominal pain, diarrhea, flatulence, nausea, vomiting, constipation; infrequently – dyspepsia, belching, dry mouth; rarely – stomatitis, gastritis, taste disorders.
Hepatobiliary system: rarely hepatitis, jaundice, hepatic encephalopathy.
River and urinary tract: infrequent – urinary tract infection; rarely – interstitial nephritis.
Skin and subcutaneous tissue disorders: rare – bullous rashes, urticaria; very rare – erythema multiforme, toxic epidermal necrolysis, Stevens-Johnson syndrome.
Muscular system disorders: frequently – back pain; infrequently – myalgia, arthralgia, leg cramps, fracture of hip, wrist or spine bones.
Reproductive system disorders: frequency unknown – gynecomastia. Laboratory and instrumental studies: rare – increase in “liver” transaminase activity, weight gain. Other: frequently – infections.
Overdose
Overdose
Symptoms
The evidence for intentional or accidental overdose is minimal.
Treatment
A specific antidote for rabeprazole is unknown. Rabeprazole binds well to plasma proteins and is therefore poorly excreted by dialysis. In case of overdose, symptomatic and supportive treatment is necessary.
Pregnancy use
Pregnancy use
There are no data on the safety of rabeprazole administration during pregnancy. Reproduction studies in rats and rabbits have not revealed any signs of fertility disorders or fetal development defects caused by rabeprazole; however, in rats, small amounts of the drug penetrate the placental barrier. Rabeprazole-SZ should not be used in pregnancy.
It is unknown whether rabeprazole is excreted with breast milk. Relevant studies on the use of the drug during breast-feeding have not been conducted. However, rabeprazole is found in the milk of lactating rats, and therefore Rabeprazole-SZ should not be used in women during breastfeeding.
Similarities
Similarities
Additional information
| Weight | 0.020 kg |
|---|---|
| Shelf life | 3 years. Do not use after the expiration date printed on the package. |
| Conditions of storage | In a dry, light-protected place at a temperature not exceeding 25 oC. |
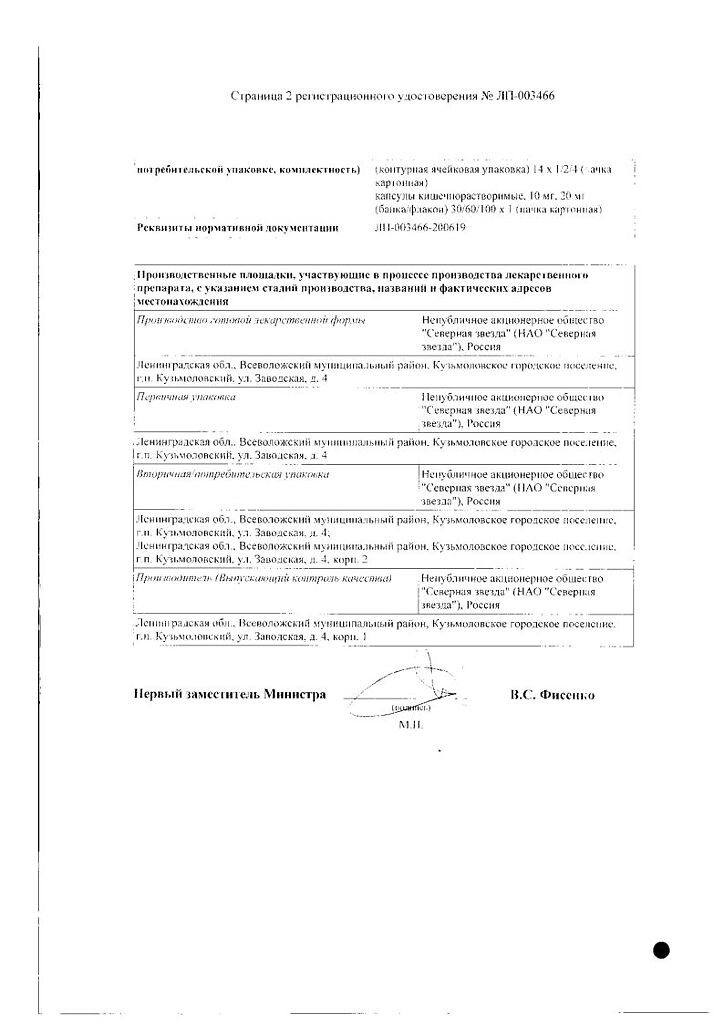
| Manufacturer | North Star NAO, Russia |
| Medication form | enteric capsules |
| Brand | North Star NAO |
Other forms…
Related products
Buy Rabeprazole-SZ, 10 mg 28 pcs with delivery to USA, UK, Europe and over 120 other countries.