No products in the cart.
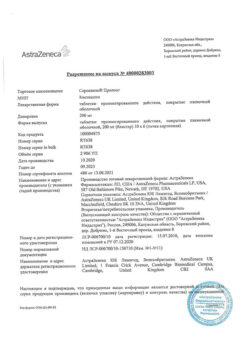
Quentiax, tablets 25 mg, 60 pcs.
€1.00
Out of stock
(E-mail when Stock is available)
Description
an antipsychotic (neuroleptic)
Indications
Indications
Quentiax® is indicated for the treatment of adults over 18 years of age with:
• schizophrenia;
• manic episodes in the structure of bipolar disorder;
• depressive episodes of moderate to severe severity in the structure of bipolar disorder.
The drug is not indicated for the prevention of manic and depressive episodes.
Pharmacological effect
Pharmacological effect
Pharmacodynamics
Mechanism of action
Quetiapine is an atypical antipsychotic drug. Quetiapine and its active metabolite N-desalkylquetiapine (norquetiapine) interact with a wide range of neurotransmitter receptors in the brain. Quetiapine and N-desalkylquetiapine exhibit high affinity for 5HT2-serotonin receptors and D1-, D2-dopamine receptors of the brain. Antagonism to these receptors, combined with higher selectivity for 5HT2-serotonin receptors than for D2-dopamine receptors, determines the main clinical antipsychotic properties of quetiapine and the low incidence of extrapyramidal adverse reactions. Quetiapine and norquetiapine do not show significant affinity for benzodiazepine receptors, but have high affinity for histamine and α1-adrenergic receptors and moderate affinity for α2-adrenergic receptors. In addition, quetiapine has no or low affinity for muscarinic receptors, while norquetiapine exhibits moderate to high affinity for several muscarinic receptor subtypes, which explains the drug’s anticholinergic (muscarinic) effects. Inhibition of the norepinephrine transporter and partial agonism of 5HT1A-serotonin receptors, exhibited by N-dealkylquetiapine, may determine the antidepressant effect of the drug.
Pharmacodynamic effects
Quetiapine is active in tests for antipsychotic activities such as conditioned avoidance. It also blocks the effects of dopamine agonists, assessed either in behavioral or electrophysiological studies, and increases concentrations of the dopamine metabolite, a neurochemical indicator of D2 receptor blockade. Results from studies of extrapyramidal symptoms (EPS) in preclinical studies have shown that quetiapine differs from standard antipsychotics and has an atypical profile. Quetiapine does not cause increased sensitivity of dopamine D2 receptors with long-term use. Quetiapine causes mild catalepsy at doses that effectively block D2 receptors. Quetiapine selectively acts on the limbic system, causing a depolarizing blockade of mesolimbic, but not nigrostriatal dopaminergic neurons. When administered short- or long-term, quetiapine had minimal potential to cause dystonia in haloperidol-sensitized or unmedicated capuchin monkeys.
Clinical effectiveness
Quetiapine is effective against both positive and negative symptoms of schizophrenia.
Quetiapine is effective as monotherapy for moderate to severe manic episodes. There are no data on long-term use of quetiapine for the prevention of subsequent manic and depressive episodes. Data on the use of quetiapine in combination with semisodium valproate or lithium for moderate to severe manic episodes are limited, but this combination therapy was generally well tolerated. In addition, quetiapine at doses of 300 mg and 600 mg is effective in patients with moderate to severe bipolar disorder I and II. At the same time, the effectiveness of quetiapine when taken at a dose of 300 mg and 600 mg per day is comparable. Quetiapine is effective in patients with schizophrenia and mania when taken twice daily, although the half-life of quetiapine is approximately 7 hours. The effect of quetiapine on 5HT2 and D2 receptors lasts up to 12 hours after taking the drug.
When taking quetiapine with dose titration in schizophrenia, the frequency of EPS and concomitant use of m-anticholinergics was comparable to that when taking placebo. When quetiapine was prescribed in fixed doses from 75 to 750 mg/day to patients with schizophrenia, the incidence of EPS and the need for concomitant use of m-anticholinergic drugs did not increase.
When quetiapine was used in doses up to 800 mg/day for the treatment of moderate to severe manic episodes, either as monotherapy or in combination with lithium or semisodium valproate, the incidence of EPS and concomitant use of m-anticholinergic drugs was comparable to that with placebo.
Pharmacokinetics
Suction
Quetiapine is well absorbed from the gastrointestinal tract. Food intake does not significantly affect bioavailability. The equilibrium molar concentration of the active metabolite N-desalkylquetiapine is 35% of that of quetiapine.
The pharmacokinetics of quetiapine is linear.
Distribution
Approximately 83% of quetiapine is bound to plasma proteins.
Metabolism
In vitro studies have shown that the CYP3A4 isoenzyme is a key isoenzyme in the metabolism of quetiapine, mediated by the cytochrome P450 system. N-desalkylquetiapine is formed and eliminated with the participation of the CYP3A4 isoenzyme.
Quetiapine and some of its metabolites (including N-desalkylquetiapine) have weak inhibitory activity against cytochrome P450 isoenzymes 1A2, 2C9, 2C19, 2D6 and 3A4, but only at concentrations 5-50 times higher than those observed at the commonly used effective dose of 300-800 mg/day. Based on the results of in vitro studies, it should not be expected that the simultaneous use of quetiapine with other drugs will lead to clinically significant inhibition of the metabolism of other drugs mediated by the cytochrome P450 system.
Removal
The half-life of quetiapine and N-desalkylquetiapine is approximately 7 and 12 hours, respectively.
Approximately 73% of quetiapine is excreted by the kidneys and 21% through the intestines. Quetiapine is actively metabolized in the liver; less than 5% of quetiapine is not metabolized and is excreted unchanged by the kidneys or through the intestines.
Pharmacokinetics in different patient groups
Floor
There are no differences in pharmacokinetic parameters between men and women.
Elderly patients
The average clearance of quetiapine in elderly patients is 30-50% less than in patients aged 18 to 65 years.
Renal dysfunction
The average plasma clearance of quetiapine is reduced by approximately 25% in patients with severe renal impairment (creatinine clearance less than 30 ml/min/1.73 m2), but individual clearance rates are within the range of values found in healthy volunteers.
Liver dysfunction
In patients with liver failure (compensated alcoholic cirrhosis), the average plasma clearance of quetiapine is reduced by approximately 25%. Since quetiapine is extensively metabolized in the liver, in patients with liver failure, plasma concentrations of quetiapine may increase, which requires dose adjustment.
Special instructions
Special instructions
Driving vehicles and working with machinery
The drug may cause drowsiness and other unwanted reactions that impair attention. Avoid driving or operating machinery while taking this drug until you know how this drug affects you.
Quentiax® contains lactose monohydrate
If you have an intolerance to certain sugars, consult your doctor before taking this drug.
Quentiax® contains sodium
This medicine contains less than 1 mmol (23 mg) sodium per tablet, which is essentially sodium-free.
Active ingredient
Active ingredient
Quetiapine
Composition
Composition
The active substance is quetiapine.
Quentiax®, 25 mg, film-coated tablets
Each tablet contains 25 mg of quetiapine.
Other ingredients (excipients) are: lactose monohydrate, calcium hydrogen phosphate dihydrate, microcrystalline cellulose, type 101, microcrystalline cellulose, type 102, povidone K-25, sodium carboxymethyl starch (type A), magnesium stearate, hypromellose, titanium dioxide (E171), macrogol-4000, iron oxide dye yellow (E172), iron oxide dye red (E172).
Quentiax®, 100 mg, film-coated tablets
Each tablet contains 100 mg of quetiapine.
Other ingredients (excipients) are: lactose monohydrate, calcium hydrogen phosphate dihydrate, microcrystalline cellulose, type 101, microcrystalline cellulose, type 102, povidone K-25, sodium carboxymethyl starch (type A), magnesium stearate, hypromellose, titanium dioxide (E171), macrogol-4000, iron oxide dye yellow (E172).
Quentiax®, 200 mg, film-coated tablets
Each tablet contains 200 mg of quetiapine.
Other ingredients (excipients) are: lactose monohydrate, calcium hydrogen phosphate dihydrate, microcrystalline cellulose, type 101, microcrystalline cellulose, type 102, povidone K-25, sodium carboxymethyl starch (type A), magnesium stearate, hypromellose, titanium dioxide (E171), macrogol-4000.
Quentiax®, 300 mg, film-coated tablets
Each tablet contains 300 mg of quetiapine.
Other ingredients (excipients) are: lactose monohydrate, calcium hydrogen phosphate dihydrate, microcrystalline cellulose, type 101, microcrystalline cellulose, type 102, povidone K-25, sodium carboxymethyl starch (type A), magnesium stearate, hypromellose, titanium dioxide (E171), macrogol-4000.
Pregnancy
Pregnancy
If you are pregnant or breastfeeding, think you may be pregnant, or are planning to become pregnant, talk to your doctor or pharmacist before taking this medicine.
Pregnancy
Do not take Quentiax® during pregnancy unless directed by your doctor. In newborns whose mothers took quetiapine in the last trimester of pregnancy, the following symptoms were observed, which may be signs of drug withdrawal syndrome: trembling, excessive tension (rigidity) or muscle weakness, drowsiness, agitation, breathing problems, difficulty feeding. If your child has any of these symptoms, contact your doctor.
Breastfeeding
The use of the drug during breastfeeding is contraindicated.
Contraindications
Contraindications
Do not take Quentiax® if:
you are allergic to quetiapine or any of the other ingredients of this medicine (listed in section 6 of the leaflet);
You are taking any of the following drugs that belong to the group of cytochrome P450 inhibitors:
some antifungal agents from the azole group;
erythromycin or clarithromycin (used to treat some infections);
nefazadone (used to treat depression);
human immunodeficiency virus (HIV) protease inhibitors;
You are breastfeeding;
You are under 18 years of age.
If any of the above applies to you (or you have any doubts), please tell your doctor.
Special instructions and precautions
Before starting to take Quentiax®, consult your doctor.
Be sure to tell your doctor if any of the following applies to you.
Thoughts about suicide (suicidal ideation) and worsening depression
If you are depressed, you may sometimes have thoughts about death or harming yourself. Such thoughts often arise at the very beginning of treatment. It takes time for the medications to start working, this period is usually about two weeks, but sometimes longer. These thoughts may become worse if you suddenly stop taking your medication.
If you have thoughts of harming or killing yourself, consult a doctor immediately. Tell a relative or close friend that you are depressed and ask them to read this leaflet. You can ask them to tell you if they think your signs of depression have become worse or if they are concerned about changes in your behavior.
Drowsiness
While taking the drug, drowsiness may develop. If you develop severe drowsiness, you may need to visit your doctor more often. In some cases, your doctor may decide to stop taking this drug.
Cardiovascular diseases
Warn your doctor if you have problems with the heart and (or) blood vessels (including the blood vessels of the brain), since while taking Quentiax®, your blood pressure may significantly decrease, which may result in dizziness, and this increases the risk of accidental injury due to a fall.
Sleep apnea syndrome (sleep apnea)
While taking Quentiax®, apnea syndrome may develop, so caution should be exercised when taking this drug. Tell your doctor if you have or have previously had this condition.
Seizures
Tell your doctor if you have previously had seizures. In this case, caution should be exercised when taking Quentiax®.
Movement disorders (extrapyramidal symptoms)
While taking Quentiax®, movement disorders may develop (see section “Possible adverse reactions”). Symptoms of movement disorders may manifest as a subjective feeling of inner restlessness, accompanied by mental distress and an inability to sit or stand still (akathisia).
Involuntary movements (tardive dyskinesia)
During treatment, symptoms such as involuntary movements of various muscles or muscle groups may appear. In this case, the doctor may decide to reduce the dose or discontinue the drug.
Neuroleptic malignant syndrome
While taking antipsychotic drugs, including Quentiax, neuroleptic malignant syndrome may develop, which can be manifested by increased body temperature, increased muscle tone, severe mood changes, and pain in various parts of the body. In this case, the doctor may decide to discontinue the drug.
Blood disorders
Tell your doctor if you have previously had a decrease in the number of white blood cells in your blood (leukopenia, neutropenia, agranulocytosis) while taking medications. While taking Quentiax®, it is also possible to develop a pronounced decrease in white blood cells (agranulocytosis). In this case, the doctor will regularly monitor you and monitor your blood counts.
Increased blood glucose levels (hyperglycemia)
When using antipsychotics, including Quentiax®, high blood glucose levels (hyperglycemia) may develop. Symptoms of hyperglycemia are: increased amount of urine excreted (polyuria), abnormally increased thirst (polydipsia), increased appetite (polyphagia) and weakness. If you have diabetes, this condition can make it worse. Your doctor will monitor your glucose and lipid levels and monitor your weight.
Heart disorders
Be sure to tell your doctor if you have or have had any heart problems (such as an abnormal heart rhythm (congenital long QT syndrome), weakening of the heart muscle (heart failure), changes in the heart muscle (cardiomyopathy, myocardial hypertrophy), inflammation of the heart muscle (myocarditis)) or if you are taking any medications that may affect the functioning of your heart.
Skin disorders
While taking Quentiax®, skin reactions may develop, which may include rash, blisters, itching, fever, and swollen lymph nodes (see section “Possible Adverse Reactions”). In this case, your doctor may decide to stop the drug.
Also, before you start taking the drug, be sure to tell your doctor if:
You have had problems related to alcohol or drug abuse;
You are an elderly person and have impaired brain function (dementia);
you have or have previously had a condition in which you cannot empty your bladder completely (urinary retention), or if you have an enlarged prostate gland (applies to men only);
you have impaired intestinal muscle movement (peristalsis) or a tendency to constipation;
you have increased intraocular pressure;
you have liver problems;
you have and/or previously had a swallowing disorder (dysphagia);
you are predisposed to blockage of veins by blood clots (venous thromboembolism);
you are predisposed to inflammation of the pancreas (pancreatitis) (for example, you drink alcohol excessively, you have been diagnosed with gallstones (cholelithiasis) or have an increase in the concentration of fats (lipids) in the blood).
Impact on screening test results
While taking quetiapine, false-positive results of screening tests for methadone and tricyclic antidepressants are possible. If this happens, your doctor will order a more specific test.
If any of the above apply to you, tell your doctor before you start taking Quentiax®.
Children and teenagers
Quentiax® is contraindicated in children and adolescents under 18 years of age.
Side Effects
Side Effects
Like all medicines, Quentiax® can cause side effects, although not everyone gets them.
Stop taking Quentiax® immediately and get medical help if you experience any of the following serious side effects:
Uncommon (may affect up to 1 in 100 people):
uncontrolled movements of the muscles of the face or tongue (tardive dyskinesia);
convulsions;
itching, rashes, weakness, blistering of the skin (hypersensitivity reactions).
Rare (may affect up to 1 in 1000 people):
a combination of increased temperature (fever), severe muscle stiffness and tension (tightness), sweating, depression of consciousness, increased blood pressure or increased heart rate are possible signs of neuroleptic malignant syndrome;
prolonged and painful erection (priapism);
intestinal obstruction.
Very rare (may affect up to 1 in 10,000 people):
severe skin reactions, accompanied by extensive skin rash, blisters on the skin and mucous membranes, fever, muscle and joint pain (Stevens-Johnson syndrome);
sudden swelling of the face, lips, tongue, or throat with difficulty breathing or swallowing (angioedema);
a sudden severe allergic reaction, accompanied by anxiety, difficulty breathing, dizziness, and a sharp decrease in blood pressure (anaphylactic reaction).
Frequency unknown (frequency cannot be determined from available data):
acute severe, life-threatening allergic disease with the formation of extensive blisters on the skin and damage to internal organs (toxic epidermal necrolysis);
Flu-like symptoms with rash, fever, swollen lymph nodes and changes in blood tests (including elevated levels of certain types of white blood cells (eosinophilia) and liver enzymes in the blood) are possible signs of a drug reaction with eosinophilia and systemic symptoms – DRESS syndrome.
Other possible adverse reactions
Very common (may affect more than 1 in 10 people):
headache;
dizziness;
drowsiness;
extrapyramidal symptoms – motor restlessness, need to move, inability to sit or stand without moving (akathisia), tremor, repetitive involuntary movements (dyskinesia), contractions of individual muscle groups (dystonia), anxiety, increased motor activity and mental excitability (psychomotor agitation) and muscle tension (muscle rigidity);
dry mouth;
weight gain;
insomnia, nausea, headache, diarrhea, vomiting, dizziness and irritability (possible signs of withdrawal syndrome) (see section “If you stop taking Quentiax®”);
changes in the blood: concentrations of lipids (triglycerides), cholesterol, decreased hemoglobin.
Common (may affect up to 1 in 10 people):
speech impairment (dysarthria);
unusual and nightmare dreams;
increased appetite;
blurred vision;
rapid heartbeat (tachycardia), palpitations;
dyspnea;
decreased blood pressure when standing up (orthostatic hypotension);
indigestion (dyspepsia), constipation, vomiting.
Uncommon (may affect up to 1 in 100 people):
restless legs syndrome, fainting, confusion;
slow heartbeat (bradycardia), changes in the electrocardiogram – prolongation of the QT interval;
runny nose (rhinitis);
difficulty swallowing (dysphagia);
urinary retention;
changes in blood test:
decreased platelet count (thrombocytopenia);
increased activity of aspartate aminotransferase (AST);
decrease in the concentration of free triiodothyronine (T3).
Rare (may affect up to 1 in 1000 people):
sleepwalking (somnambulism) and related phenomena;
impaired intestinal motility (ileus);
yellow tint of the skin and mucous membranes (jaundice);
secretion of milk from the mammary glands (galactorrhea);
decreased body temperature (hypothermia);
changes in blood test:
increased activity of creatine phosphokinase (CPK);
a marked decrease in leukocytes in the blood (agranulocytosis).
Very rare (may affect up to 1 in 10,000 people):
diabetes mellitus;
inflammation of the liver (hepatitis) (with or without jaundice);
muscle pain, weakness, dark urine (possible signs of rhabdomyolysis).
Frequency unknown (frequency cannot be determined from available data):
decrease in some white blood cells (neutropenia);
inflammatory reaction with rashes on the skin and, possibly, on the mucous membrane (erythema multiforme);
an acute allergic reaction, which manifests itself in the form of widespread rashes accompanied by redness of the skin (erythema) and fever (acute generalized exanthematous pustulosis);
inflammation of skin blood vessels (cutaneous vasculitis);
withdrawal syndrome in newborns (see section “Pregnancy, breastfeeding, fertility”).
The class of drugs that Quentiax belongs to can cause heart rhythm problems that can be serious and, in severe cases, fatal.
Some adverse reactions can only be detected by a blood test. These include changes in triglyceride, cholesterol, or glucose levels in the blood, changes in thyroid hormone concentrations, increased activity of certain enzymes, decreased numbers of certain types of blood cells, decreased red blood cell counts, decreased sodium levels, and increased levels of a hormone called prolactin. Elevated prolactin levels can lead to breast engorgement and unexpected milk production in both women and men, as well as menstrual irregularities in women.
Interaction
Interaction
Tell your doctor if you are taking, have recently taken, or may start taking any other medications.
Do not take Quentiax® if you are taking any of the following drugs:
some drugs that are used to treat infection caused by the human immunodeficiency virus (HIV infection);
drugs of the azole group (used in the treatment of fungal infections), for example, ketoconazole;
erythromycin or clarithromycin (used to treat certain infections);
nefazodone (used to treat depression).
The following drugs reduce the effect of Quentiax®:
phenytoin or carbamazepine (used to treat epilepsy);
thioridazine (another antipsychotic drug).
The following drugs have no effect on Quentiax®:
phenazone (to treat pain);
imipramine, fluoxetine (drugs to treat depression);
risperidone, haloperidol, lithium (other antipsychotic drugs);
cimetidine (a medicine to treat high stomach acidity);
valproic acid (used in the treatment of epilepsy).
Caution should be exercised when using Quentiax® simultaneously with the following drugs:
drugs that affect the heart, such as drugs that may cause electrolyte imbalance (low potassium or magnesium) or drugs that cause QT interval prolongation (on electrocardiogram), such as diuretics (water medications) or certain antibiotics (drugs to treat infections);
drugs that cause constipation;
drugs (called “anticholinergics”) that affect the functioning of nerve cells (used to treat certain diseases of various organs and systems).
Before stopping any medications, discuss this with your doctor first.
Use of Quentiax® with food, drinks and alcohol
Quentiax® can be taken with or without food.
Alcohol increases drowsiness, which may occur due to quetiapine. Do not take Quentiax® with alcohol.
Grapefruit juice may affect the effectiveness of quetiapine. Do not drink grapefruit juice if you are taking Quentiax®.
Action
Action
Quetiapine is an atypical antipsychotic drug that interacts with a wide range of specific brain receptors, which determines the main antipsychotic properties of quetiapine and the low incidence of adverse reactions from the neuromuscular system (extrapyramidal symptoms).
If there is no improvement or you feel worse, you should consult a doctor.
Storage conditions
Storage conditions
Keep the drug out of the reach of children and so that the child cannot see it.
Do not use the drug after the expiration date (shelf life) indicated on the package after the words “Best before:…”.
The expiration date is the last day of the given month.
Store at a temperature not exceeding 25 °C, in the original packaging (blister).
Do not throw the drug into the sewer (water supply). Ask your pharmacist how to dispose of (destroy) a drug that is no longer needed. These measures will protect the environment.
Manufacturer
Manufacturer
KRKA-RUS/KRKA, Russia
Additional information
| Shelf life | 5 years. Do not use the drug after the expiration date. |
|---|---|
| Conditions of storage | When manufacturing at KRKA-RUS, Russia: At the temperature not more than 25 ºС, in the original package (outline cell packing). When produced at KRKA, d.d., Novo mesto, Slovenia: At a temperature not higher than 25 ºC, in the original package (blister). Keep out of reach of children. |
| Manufacturer | KRKA dd Novo mesto, Slovenia |
| Medication form | pills |
| Brand | KRKA dd Novo mesto |
Other forms…
Related products
Buy Quentiax, tablets 25 mg, 60 pcs. with delivery to USA, UK, Europe and over 120 other countries.