No products in the cart.
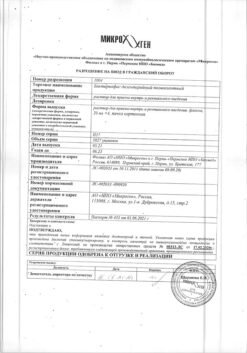
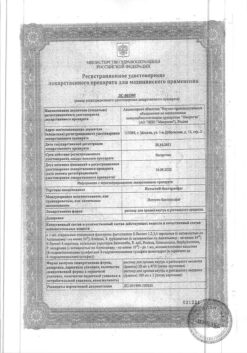
Prograf, 5 mg capsules 50 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Prograf is an immunosuppressant of the macrolide group. On molecular level tacrolimus effects are mediated by binding to cytosolic protein (FKBP12) which is responsible for intracellular accumulation of the drug.
The FKBP12-tacrolimus complex binds specifically and competitively to calcineurin and inhibits it, resulting in calcium-dependent inhibition of T-cell signal transduction pathways, thus preventing transcription of a discrete group of lymphokine genes.
Tacrolimus is a highly active immunosuppressive drug: suppresses the formation of cytotoxic lymphocytes, which are mainly responsible for transplant rejection, reduces T-cell activation, T-helper-dependent B-cell proliferation, and lymphokine formation (such as interleukins-2, -3 and γ-interferon) and interleukin-2 receptor expression.
Indications
Indications
Prevention and treatment of hepatic, renal and cardiac allograft rejection, including those resistant to standard immunosuppressive therapy regimens.
Active ingredient
Active ingredient
Composition
Composition
active ingredient:
tacrolimus 5 mg
How to take, the dosage
How to take, the dosage
It is recommended that the daily oral dose be divided into two doses (e.g., in the morning and in the evening). The capsules should be taken immediately after taking them out of the blister pack. The capsules should be swallowed with liquids (preferably water).
To achieve maximum absorption, the capsules should be taken on an empty stomach (on an empty stomach) or at least 1 hour or 2-3 hours after a meal.
No detectable effect of food on absorption of the drug in patients with a kidney transplant has been noted.
Interaction
Interaction
Pharmacokinetic interaction
Tacrolimus is largely metabolized by the hepatic microsomal cytochrome P450 isoenzyme 3A4 (CYP3A4). Concomitant use of drugs or herbal medicines that inhibit or induce CYP3A4 may affect the metabolism of tacrolimus and thereby decrease or increase tacrolimus blood levels.
Tacrolimus also has a broad and potent effect on CYP3A4 dependent metabolism; thus, co-administration of tacrolimus with drugs that are metabolized by CYP3A4 dependent pathways may affect the metabolism of these drugs (e.g. cortisone, testosterone).
Tacrolimus binds significantly to plasma proteins. Possible interactions with other drugs that have high affinity for blood proteins (e.g. NSAIDs, oral anticoagulants or oral antidiabetic drugs) should be considered.
Pharmacodynamic interaction
Concomitant use of tacrolimus with drugs that have nephrotoxic or neurotoxic effects may increase toxicity (e.g., aminoglycosides, gyrase inhibitors (type II DNA topoisomerase), vancomycin, co-trimoxazole, NSAIDs, ganciclovir or acyclovir).
Because treatment with tacrolimus may accompany the development of hyperkalemia or aggravate pre-existing hyperkalemia, should be avoided:
– excessive potassium intake;
– use of potassium-saving diuretics (e.g., amiloride, triamterene, or spironolactone).
Other interactions
Vaccines may have less efficacy when using tacrolimus, so administration of live attenuated vaccines should be avoided.
Clinically significant interactions
The following interaction of tacrolimus with concomitant therapies has been observed in clinical use. The underlying mechanism of interaction is known. Drugs marked with an asterisk will require a change in tacrolimus dosage in almost all patients. Other drugs listed below may require dose adjustments in individual cases.
The following drugs inhibit CYP3A4 and have been shown to increase tacrolimus blood levels:
-ketoconazole*, fluconazole*, itraconazole*, clotrimazole, voriconazole;*
– nifedipine, nicardipine;
– erythromycin*, clarithromycin, jozamycin;
– HIV protease inhibitors;
– danazole, ethinylestradiol;
– omeprazole;
– calcium channel antagonists such as diltiazem;
– nefazodone.
The following drugs induce CYP3A4 and have been shown to lower tacrolimus blood levels:
– rifampicin* (rifampin);
– phenytoin*;
– phenobarbital;
– St. John’s wort.
Tacrolimus increased blood levels of phenytoin.
Methylprednisolone was observed to both increase and decrease plasma levels of tacrolimus.
An increase in nephrotoxicity was observed after use of any of the following drugs in conjunction with tacrolimus:
– amphotericin B;
– ibuprofen.
The elimination half-life of cyclosporine has been shown to be increased with concomitant use with tacrolimus. In addition, synergistic/additive effects may develop. For these reasons, the combined use of cyclosporine and tacrolimus is not recommended when prescribing tacrolimus to patients who previously received cyclosporine.
Interaction with food
It has been noted that grapefruit juice increases tacrolimus blood levels due to inhibition of CYP3A4 activity.
Potential interactions
Substances that inhibit the cytochrome P450 3A system
Based on in vitro studies, the following substances may be considered as potential metabolic inhibitors: Bromocriptine, cortisone, dapsone, ergotamine, gestodene, lidocaine, mephenytoin, miconazole, midazolam, nilvadipine, poratidron, quinidine, tamoxifen, (triacetyl) oleandomycin and verapamil.
Substances that induce the cytochrome P450 3A system
Carbamazepine, methamizole and isoniazid induce cytochrome P450 3A.
Inhibition by tacrolimus of metabolism of other substances mediated by the cytochrome P450 3A system.
Since tacrolimus can affect the metabolism of steroid contraceptives, special attention should be paid to measures to protect against pregnancy.
In an alkaline environment, tacrolimus is not stable. Co-administration of Prograf® reconstituted infusion concentrate (5 mg/ml), with other drugs that significantly alkalize the solution (e.g., acyclovir and ganciclovir) should be avoided.
Special Instructions
Special Instructions
The following parameters should be routinely monitored during the initial period after transplantation: BP, ECG, neurological and ophthalmological status, fasting blood glucose levels, electrolytes (especially potassium), liver and renal function, clinical blood count parameters, coagulation indices and plasma protein determinations.
As with other immunosuppressive drugs, because of the potential risk of malignant changes in the skin, exposure to sunlight and UV radiation should be limited by protecting the skin with clothing and using creams with a high protection factor.
If accidentally injected into an artery or perivascularly, Prograf ® concentrate for infusion at 5 mg/ml may cause irritation in the area of injection.
Prograf® concentrate for preparation of 5 mg/ml infusion solution contains polyoxyethylated hydrogenated castor oil, which has been noted to cause anaphylactic reactions. The risk of developing an anaphylactic reaction can be reduced by administering reconstituted Prograf® concentrate for 5 mg/ml infusions at a low rate or by first administering an antihistamine drug.
Prograf®, 0.5; 1 and 5 mg capsules
Tacrolimus is not compatible with polyvinyl chloride (PVC). If the contents of the capsules must be inserted through a nasogastric tube, the latter must not contain PVC.
Prograf®, concentrate for preparation of infusion solution containing 5 mg/ml
Tacrolimus is absorbed by polyvinyl chloride plastic. Tubes, syringes and any other equipment used to prepare and administer Prograf® , infusion concentrate containing 5 mg/ml must not contain polyvinyl chloride.
Impact on driving and operating machinery
Tacrolimus may cause visual and neurological impairment. Patients who develop these abnormalities should not drive a car or operate machinery. These effects may be exacerbated if Prograf® is taken concomitantly with alcohol.
Contraindications
Contraindications
Known hypersensitivity to tacrolimus or other macrolides.
Known hypersensitivity to polyoxyethylated hydrogenated castor oil (HCO-60) or structurally related components.
Side effects
Side effects
Many of the adverse drug reactions stated below are reversible and/or reduced with dosage reduction. The incidence of adverse drug reactions is lower with oral administration than with intravenous administration. The reactions are listed below in descending order of frequency of development:
The cardiovascular system: very common – hypertension; common – hypotension, tachycardia, cardiac arrhythmias and conduction disturbances, thromboembolic and ischemic manifestations, angina pectoris, vascular disease; infrequent – abnormal ECG parameters, heart attack, heart failure, shock, myocardial hypertrophy, cardiac arrest.
Gastrointestinal and liver diseases: very common – diarrhea, nausea and/or vomiting; common – GI dysfunction (such as dyspepsia), abnormal liver enzyme levels, abdominal pain, constipation, changes in body weight and appetite, inflammation and ulcers in GI, jaundice, biliary tract and gallbladder disease; infrequent – ascites, bowel obstruction (ileus), liver tissue lesions, pancreatitis; rare – liver failure.
Blood and lymphatic system: frequently – anemia, leukopenia, thrombocytopenia, hemorrhage, leukocytosis, coagulation disorders; infrequently – insufficiency of hematopoietic system, including pancytopenia, thrombotic microangiopathy.
Kidney: very common – renal dysfunction (e.g., increased serum creatinine level); common – renal tissue damage, renal failure; infrequent – proteinuria.
Metabolism and electrolytes: very common – hyperglycemia, hyperkalemia, diabetes mellitus; common – hypomagnesemia, hyperlipidemia, hypophosphatemia, hypokalemia, hyperuricemia, hypocalcemia, acidosis, hyponatremia, hypovolemia, dehydration; infrequent – hypoproteinuria, hyperphosphatemia, increased amylase levels, hypoglycemia.
Muscular and skeletal system: frequently – seizures; infrequently – myasthenia gravis, joint diseases.
Nervous system/sensory system: very common – tremor, headache, insomnia; common – sensory disturbances (e.g. paresthesia), visual disturbances, confusion, depression, dizziness, agitation, neuropathy, seizures, discoordination, psychosis, anxiety, nervousness, sleep disturbances, impaired consciousness, emotional lability, hallucinations, hearing disturbances, thinking disorders, encephalopathy; infrequent – hypertension, eye disease, amnesia, cataracts, speech impairment, paralysis, coma, deafness; very rare – blindness.
Respiratory system: often – respiratory dysfunction (e.g., shortness of breath), pleural effusion; infrequently – atelectasia, bronchospasm.
The skin: often – itching, alopecia, rash, sweating, acne, photosensitivity; infrequent – hirsutism; rare – Lyell’s syndrome; very rare – Stevens-Johnson syndrome.
Mixed manifestations: very often – localized pain (e.g., arthralgia); often – fever, peripheral edema, asthenia, urinary disorders; infrequently – disorders of genitalia in women, including edema.
New diseases: patients receiving immunosuppressive therapy are in the group of increased risk of malignant tumors. Both benign and malignant tumors, including Epstein-Barr virus (EBV)-associated lymphoproliferative diseases and skin cancer, have been reported with tacrolimus use.
Hypersensitivity reactions: allergic and anaphylactic reactions.
Infections: in patients receiving tacrolimus, as well as during treatment with other immunosuppressive drugs, the risk of developing infectious diseases (viral, bacterial, fungal, protozoal) is increased. The course of previously diagnosed infectious diseases may worsen.
Overdose
Overdose
Clinical experience with overdose treatment is limited.
There have been several cases of accidental overdose of the drug with the following symptoms: tremor, headache, nausea, vomiting, infections, urticaria, lethargy, increased blood urea nitrogen levels, increased serum creatinine concentration, and increased alanine aminotransferase levels.
Pregnancy use
Pregnancy use
The results of preclinical studies and studies conducted in humans show that the drug may pass through the placenta.
As the safety of Prograf in pregnant women is not well established, the drug should not be prescribed unless the possible benefit of treatment justifies the potential risk to the fetus.
The results of preclinical and human studies show that tacrolimus is excreted with breast milk. Because adverse effects on newborns cannot be ruled out, women taking Prograf should not breastfeed.
Similarities
Similarities
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C, in the original package |
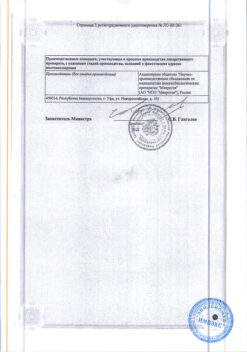
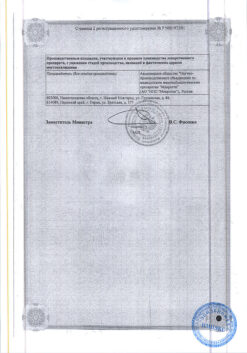
| Manufacturer | Astellas Ireland Co. |
| Medication form | capsules |
| Brand | #Н/Д |
Related products
Buy Prograf, 5 mg capsules 50 pcs with delivery to USA, UK, Europe and over 120 other countries.