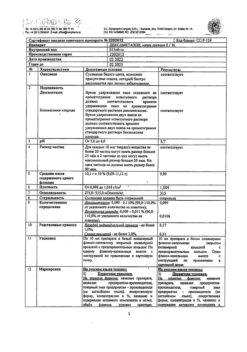
No products in the cart.
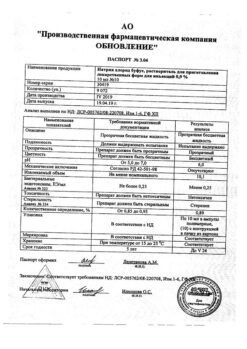
Prednisolone bufus, 30 mg/ml 1 ml 10 pcs
€4.81 €4.28
Description
Prednisolone is a synthetic glucocorticosteroid drug, a dehydrated hydrocortisone analog. It has anti-inflammatory, anti-allergic, immunosuppressive effect, increases sensitivity of beta-adrenoreceptors to endogenous catecholamines.
Interacts with cytoplasmic glucocorticosteroid receptors (GCS receptors are present in all tissues, especially in liver) to form a complex, inducing the formation of proteins (including enzymes regulating vital processes in cells).
Anti-inflammatory effect is associated with inhibition of release of inflammatory mediators by eosinophils and mast cells, induction of lipocortin formation and reduction of mast cells producing hyaluronic acid, reduction of capillary permeability, stabilization of cell membranes and organelle membranes (especially lysosomal).
Acts on all stages of the inflammatory process: inhibits the synthesis of prostaglandins at the level of arachidonic acid (Lipokortin inhibits phospholipase A2, inhibits the release of arachidonic acid and inhibits the synthesis of endoperoxins, leukotrienes, contributing to inflammation processes, allergies, etc.).); synthesis of “pro-inflammatory cytokines” (interleukin-1, tumor necrosis factor alpha, etc.); increases the resistance of cell membranes.The basic elements of the immune system are the following: > Immunodeficiency Virus (immunoenzyme), > Immunodeficiency Virus (immunoenzyme), > Immunoassay (immunoassay).
Immunosuppressive effect is caused by involution of lymphoid tissue, inhibition of lymphocyte proliferation (especially T-lymphocytes), suppression of B-lymphocyte migration and interaction between T- and B-lymphocytes, inhibition of cytokine release (interleukin-1, interleukin-2, gamma interferon) from lymphocytes and macrophages and reduction of antibody formation.
The anti-allergic action is caused by decrease of synthesis and secretion of allergy mediators, inhibition of histamine and other bioactive substances release from sensitized mast cells and basophils, reduction of circulating basophils number, decrease of T- and B-lymphocytes and mast cells quantity, suppression of lymphoid and connective tissue development, reduction of effector cells sensitivity to allergy mediators, suppression of antibodies formation, change of the body immune response.
In obstructive airways diseases the action is mainly caused by inhibition of inflammatory processes, prevention or reduction of bronchial mucous membrane edema severity, decrease of eosinophilic infiltration of submucous layer of bronchial epithelium and deposition of circulating immune complexes in bronchial mucosa, and also inhibition of mucous membrane erosion and desquamation. It increases sensitivity of small and medium caliber bronchial beta-adrenoreceptors to endogenous catecholamines and exogenous sympathomimetics, decreases mucus viscosity by reducing its production.
Inhibits the synthesis and secretion of adrenocorticotropic hormone (ACTH) and secondary to the synthesis of endogenous GCS.
Inhibits connective tissue reactions in the inflammatory process and reduces the possibility of scar tissue formation.
Effect on protein metabolism: reduces the number of globulins in the blood plasma, increases the synthesis of albumins in the liver and kidneys (with an increase in albumin/globulin ratio), reduces synthesis and increases the catabolism of protein in muscle tissue.
Effect on lipid metabolism: increases the synthesis of higher fatty acids and triglycerides; redistributes fat (mobilization from the subcutaneous tissue of the extremities and accumulation of fat mainly in the shoulder girdle, face, abdomen); leads to hypercholesterolemia.
Effect on carbohydrate metabolism: increases absorption of carbohydrates from the gastrointestinal tract (GIT), increases the activity of glucose-6-phosphatase (increased flow of glucose from the liver into the blood), increases the activity of phosphoenolpyruvate carboxylase and aminotransferase synthesis (activation of gluconeogenesis), promotes the development of hyperglycemia.
Effect on water-electrolyte metabolism: retains sodium and water in the body; stimulates potassium excretion (mineralocorticoid activity); reduces absorption of calcium from gastrointestinal tract; causes “washout” of calcium from bones and its increased renal excretion; reduces bone mineralization.
Pharmacokinetics
Absorption
Absorption during injection into thigh muscles is faster than gluteal muscles. Maximal concentration in plasma is reached after 0.5 hour after intravenous injection. With intramuscular administration maximum concentration is reached after 0.5-1 hours.
Distribution
Up to 90% of prednisolone is bound to plasma proteins: transcortin (corticosteroid-binding globulin) and albumin.
Metabolism
Prednisolone is metabolized primarily in the liver, partially in the kidneys and other tissues, mainly by conjugation with glucuronic and sulfuric acids. Metabolites are inactive.
Excretion
The elimination half-life of prednisolone from blood plasma is about 3 hours.
Excreted through the intestine and kidneys by glomerular filtration and is 80-90 % reabsorbed by the renal tubules. 20% of the dose is excreted unchanged by the kidneys.
Indications
Indications
Used for emergency treatment in conditions requiring a rapid increase in the concentration of glucocorticosteroids in the body:
shock conditions (burn, traumatic, surgical, toxic, cardiogenic) – in case of ineffectiveness of vasoconstrictors, plasma replacement drugs and other symptomatic therapy;
allergic reactions (acute severe forms), blood transfusion shock, anaphylactic shock, anaphylactoid reactions;
swelling of the brain (including due to a brain tumor or associated with surgery, radiation therapy or head trauma);
bronchial asthma (severe form), status asthmaticus;
systemic connective tissue diseases (systemic lupus erythematosus, rheumatoid arthritis);
acute adrenal insufficiency;
thyrotoxic crisis;
acute hepatitis, hepatic coma;
reduction of inflammatory phenomena and prevention of cicatricial contractions (in case of poisoning with cauterizing liquids).
Pharmacological effect
Pharmacological effect
Prednisolone is a synthetic glucocorticosteroid drug, a dehydrogenated analogue of hydrocortisone. It has anti-inflammatory, antiallergic, immunosuppressive effects, increases the sensitivity of beta-adrenergic receptors to endogenous catecholamines.
Interacts with cytoplasmic receptors of glucocorticosteroids (GCS) (GCS receptors are found in all tissues, especially in the liver) to form a complex that induces the formation of proteins (including enzymes that regulate vital processes in cells).
The anti-inflammatory effect is associated with inhibition of the release of inflammatory mediators by eosinophils and mast cells, induction of the formation of lipocortins and a decrease in the number of mast cells producing hyaluronic acid, with a decrease in capillary permeability, stabilization of cell membranes and organelle membranes (especially lysosomal).
Acts on all stages of the inflammatory process: inhibits the synthesis of prostaglandins at the level of arachidonic acid (lipocortin inhibits phospholipase A2, suppresses the release of arachidonic acid and inhibits the synthesis of endoperoxides, leukotrienes, which contribute to inflammation, allergies, etc.); synthesis of “pro-inflammatory cytokines” (interleukin-1, tumor necrosis factor alpha, etc.); increases the resistance of cell membranes to various damaging factors.
The immunosuppressive effect is caused by the involution of lymphoid tissue, inhibition of the proliferation of lymphocytes (especially T-lymphocytes), suppression of the migration of B-lymphocytes and the interaction of T- and B-lymphocytes, inhibition of the release of cytokines (interleukin-1, interleukin-2; interferon gamma) from lymphocytes and macrophages and a decrease in the formation of antibodies.
The antiallergic effect develops as a result of a decrease in the synthesis and secretion of allergy mediators, inhibition of the release of histamine and other biologically active substances from sensitized mast cells and basophils, a decrease in the number of circulating basophils, a decrease in the number of T- and B-lymphocytes, mast cells, suppression of the development of lymphoid and connective tissue, a decrease in the sensitivity of effector cells to allergy mediators, inhibition of antibody formation, changes in the immune response body.
In obstructive diseases of the respiratory tract, the effect is mainly due to inhibition of inflammatory processes, prevention or reduction of the severity of swelling of the bronchial mucous membranes, reduction of eosinophilic infiltration of the submucosal layer of the bronchial epithelium and deposition of circulating immune complexes in the bronchial mucosa, as well as inhibition of erosion and desquamation of the mucous membrane. Increases the sensitivity of beta-adrenergic receptors of small and medium caliber bronchi to endogenous catecholamines and exogenous sympathomimetics, reduces the viscosity of mucus by reducing its production.
Suppresses the synthesis and secretion of adrenocorticotropic hormone (ACTH) and secondarily the synthesis of endogenous GCS.
Inhibits connective tissue reactions during the inflammatory process and reduces the possibility of scar tissue formation.
Effect on protein metabolism: reduces the amount of globulins in the blood plasma; increases albumin synthesis in the liver and kidneys (with an increase in the albumin/globulin ratio); reduces synthesis and enhances protein catabolism in muscle tissue.
Effect on lipid metabolism: increases the synthesis of higher fatty acids and triglycerides; redistributes fat (mobilization from the subcutaneous tissue of the extremities and accumulation of fat mainly in the shoulder girdle, face, abdomen); leads to the development of hypercholesterolemia.
Effect on carbohydrate metabolism: increases the absorption of carbohydrates from the gastrointestinal tract (GIT); increases the activity of glucose-6-phosphatase (increasing the flow of glucose from the liver into the blood); increases the activity of phosphoenolpyruvate carboxylase and the synthesis of aminotransferases (activation of gluconeogenesis); promotes the development of hyperglycemia.
Effect on water-electrolyte metabolism: retains sodium and water in the body; stimulates potassium excretion (mineralocorticoid activity); reduces calcium absorption from the gastrointestinal tract; causes “leaching” of calcium from bones and increasing its renal excretion; reduces bone mineralization.
Pharmacokinetics
Absorption
Absorption when injected into the thigh muscles is faster than when injected into the gluteal muscles. When administered intravenously, the maximum concentration in blood plasma is achieved after 0.5 hours. When administered intramuscularly, the maximum concentration is achieved after 0.5-1 hour.
Distribution
Up to 90% of prednisolone is bound to plasma proteins: transcortin (corticosteroid binding globulin) and albumin.
Metabolism
Prednisolone is metabolized primarily in the liver, partially in the kidneys and other tissues, mainly by conjugation with glucuronic and sulfuric acids. Metabolites are inactive.
Removal
The half-life of prednisolone from blood plasma is about 3 hours.
It is excreted through the intestines and kidneys by glomerular filtration and is 80-90% reabsorbed by the renal tubules. 20% of the dose is excreted unchanged by the kidneys.
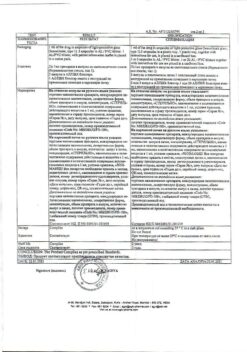
Special instructions
Special instructions
Prednisolone is contraindicated in patients with systemic fungal infections due to the risk of worsening the infection. The drug may in some cases be used for fungal infections treated with amphotericin B to reduce its side effects, but in these cases it can cause circulatory failure and hypertrophy of the left ventricular myocardium, as well as severe hypokalemia. Taking the drug with food can reduce gastrointestinal side effects.
Antacids have not been shown to be effective in preventing ulcers, gastrointestinal bleeding, or intestinal perforation. With long-term treatment, it may be necessary to limit sodium and increase potassium content, as well as increase protein content in food.
In the event of the development of steroid myopathy, if prednisolone therapy cannot be discontinued, replacing it with another GCS can alleviate the symptoms.
The risk of osteoporosis associated with long-term use of corticosteroids can be reduced by taking calcium and vitamin D or, if the patient’s condition allows, by performing appropriate physical exercise.
If psychosis or depression occurs, the dose should be reduced or discontinued if possible. If necessary, phenothiazines or lithium compounds can be used.
In order to alleviate some of the symptoms of GCS withdrawal syndrome (without suppressing the hypothalamic-pituitary-adrenal axis), acetylsalicylic acid or other NSAIDs can be prescribed.
Active ingredient
Active ingredient
Prednisolone
Composition
Composition
Active ingredient:
Prednisolone sodium phosphate – 40.32 mg
(in terms of prednisolone) – 30.00 mg
Excipients:
sodium hydrogen phosphate (disubstituted sodium phosphate) – 0.91 mg
disodium edetate dihydrate (trilon B) – 0.50 mg
sodium dihydrogen phosphate dihydrate
(sodium phosphate monosubstituted 2-water) – 0.34 mg
propylene glycol – 0.25 ml
water for injection – up to 1 ml
Pregnancy
Pregnancy
Prednisolone crosses the placenta. During pregnancy (especially in the first trimester) or in women planning pregnancy, the use of Prednisolone Bufus is indicated only if the expected therapeutic effect from the use of Prednisolone Bufus exceeds the risk of negative effects on the body of the mother and fetus. GCS should be prescribed during pregnancy only for absolute indications.
With long-term therapy during pregnancy, malformations (cleft palate) and fetal malnutrition are possible.
There is no information on the effect of GCS on the course and outcome of labor. Careful monitoring of children born to mothers who received fairly high doses of the drug during pregnancy is necessary.
Since corticosteroids pass into breast milk, if it is necessary to use the drug Prednisolone Bufus, breastfeeding the child should be avoided.
Contraindications
Contraindications
For short-term use for health reasons, the only contraindication is hypersensitivity to prednisolone or the components of the drug; systemic mycosis; epidural and intrathecal administration of the drug; cerebral edema due to traumatic brain injury; simultaneous use of live or attenuated vaccines with immunosuppressive doses of the drug; eye infection caused by the herpes simplex virus (due to the risk of corneal perforation); the use of the drug is not recommended in patients with acute or subacute myocardial infarction, since the spread of necrosis, slowdown in the formation of scar tissue and, as a result, rupture of the heart muscle are possible; in children during the period of growth, GCS should be used only for absolute indications and under especially careful supervision of the attending physician; breastfeeding period.
With caution
For gastrointestinal diseases: gastric and duodenal ulcers, esophagitis, gastritis, acute or latent peptic ulcers, recently created intestinal anastomosis, ulcerative colitis with the threat of perforation or abscess formation, diverticulitis.
For parasitic and infectious diseases of a viral, fungal or bacterial nature (currently or recently suffered, including recent contact with a patient) – herpes simplex, herpes zoster (viremic phase), chicken pox, measles; amebiasis, strongyloidiasis; active and latent tuberculosis. Use for severe infectious diseases is permissible only against the background of specific antimicrobial therapy.
In the pre- and post-vaccination period (a period of 8 weeks before and 2 weeks after vaccination), with lymphadenitis after BCG vaccination. For immunodeficiency conditions (including AIDS or HIV infections).
For diseases of the cardiovascular system: recent myocardial infarction, chronic heart failure in the stage of decompensation, arterial hypertension, hyperlipidemia.
For endocrine diseases: diabetes mellitus (including impaired glucose tolerance), hyperthyroidism, hypothyroidism, stage III–IV obesity).
In case of severe chronic renal and/or liver failure, nephrourolithiasis. For hypoalbuminemia and conditions predisposing to its occurrence (liver cirrhosis, nephrotic syndrome).
For systemic osteoporosis, myasthenia gravis, acute psychosis, poliomyelitis (except for the form of bulbar encephalitis), open- and closed-angle glaucoma.
In patients with current thromboembolic complications or who are predisposed to developing these complications.
With a history of severe affective disorders.
With convulsive syndrome.
During pregnancy.
In elderly patients, Prednisolone Bufus should be used with caution due to the increased risk of developing osteoporosis and arterial hypertension.
In children during the growth period, GCS should be used only for absolute indications and under the careful supervision of the attending physician.
Side Effects
Side Effects
With short-term use of prednisolone, like other corticosteroids, side effects are rarely observed. When using prednisolone for a long time, the following side effects may develop:
Disturbances of water and electrolyte metabolism: sodium and fluid retention in the body, hypokalemia, hypokalemic alkalosis.
From the cardiovascular system: increased blood pressure, circulatory failure.
From the musculoskeletal system: muscle weakness, steroid myopathy, loss of muscle mass, osteoporosis, compression fracture of the spine, aseptic necrosis of the heads of the femur and humerus, pathological fractures of long tubular bones.
From the gastrointestinal tract: steroid ulcer with possible perforation and bleeding, pancreatitis, flatulence, ulcerative esophagitis, indigestion, nausea, increased appetite.
From the skin: atrophic stripes, acne, delayed wound healing, thinning of the skin, petechiae and hematomas, erythema, increased sweating, allergic dermatitis, urticaria, angioedema.
From the nervous system and sensory organs: increased intracranial pressure with optic nerve congestion syndrome (pseudotumor of the brain – more often in children, usually after too rapid dose reduction, symptoms – headache, deterioration of visual acuity or double vision); convulsions, dizziness, headache, sleep disturbance, posterior subcapsular cataract, increased intraocular pressure, glaucoma; exophthalmos.
Endocrine status: secondary adrenal and hypothalamic-pituitary insufficiency (especially during stressful situations such as illness, injury, surgery); Cushing’s syndrome; growth suppression in children; menstrual irregularities; decreased tolerance to carbohydrates; manifestation of latent diabetes mellitus and increased need for insulin or oral antidiabetic drugs in patients with diabetes mellitus, hirsutism.
From the side of metabolism: negative nitrogen balance as a result of protein catabolism, hyperglycemia, glycosuria.
Mental disorders: symptoms simulating schizophrenia, mania or delirium (most often appear during the first two weeks of treatment). Women and patients with lupus erythematosus are most susceptible to mental disorders.
Other: anaphylactic reactions and hypersensitivity reactions, obliterating endarteritis, weight gain, masking the symptoms of infectious diseases, fainting.
Interaction
Interaction
Cardiac glycosides: increased risk of cardiac arrhythmias and glycoside toxicity associated with hypokalemia.
Barbiturates, antiepileptic drugs (phenytoin, carbamazepine), rifampicin, glutethimide accelerate the metabolism of GCS (by inducing microsomal enzymes) and weaken their effect.
Antihistamines weaken the effect of prednisolone.
Amphotericin B, carbonic anhydrase inhibitors: hypokalemia, left ventricular myocardial hypertrophy, circulatory failure.
Paracetamol: hypernatremia, peripheral edema, increased calcium excretion, risk of hypocalcemia and osteoporosis. Increased risk of paracetamol hepatotoxicity.
Anabolic steroids, androgens: increased risk of developing peripheral edema, acne; use with caution, especially in cases of liver and heart disease.
Oral contraceptives containing estrogens: an increase in the concentration of globulins that bind glucocorticosteroids in the blood serum, a slowdown in metabolism, an increase in T1/2, an increase in the effect of prednisolone.
Anticholinergic drugs (mainly atropine) – increase intraocular pressure.
Anticoagulants (coumarin derivatives, indanedione, heparin), streptokinase, urokinase: decreased, and in some patients increased, effectiveness; the dose should be determined based on the PT; increased risk of ulcer formation and bleeding from the gastrointestinal tract.
Tricyclic antidepressants may increase psychiatric disorders associated with prednisolone. They should not be prescribed for the treatment of these disorders.
Oral antidiabetic drugs, insulin: weakening of the hypoglycemic effect, increasing the concentration of glucose in the blood. It is possible to adjust the dose of antidiabetic drugs.
Antithyroid drugs, thyroid hormones – changes in thyroid function (the dose of these drugs may be adjusted or discontinued).
Diuretics: weakening of the effect of diuretics (potassium-sparing), hypokalemia.
Laxatives: decreased effect, hypokalemia.
Ephedrine can accelerate the metabolism of GCS (prednisolone dose adjustment is possible).
Immunosuppressive drugs: increased risk of infection, lymphoma and other lymphoproliferative diseases.
Isoniazid: decrease in the concentration of isoniazid in the blood plasma, mainly in individuals with rapid acetylation (dose changes are possible).
Mexiletine: acceleration of the metabolism of mexiletine and reduction of its concentration in the blood serum.
Drugs that block neuromuscular conduction (depolarizing muscle relaxants): Hypocalcemia associated with the use of prednisolone may increase synaptic blockade, leading to an increase in the duration of neuromuscular blockade.
NSAIDs, acetylsalicylic acid, alcohol: weakened effect, increased risk of developing peptic ulcers and bleeding from the gastrointestinal tract.
Drugs and food containing sodium: peripheral edema, arterial hypertension (it may be necessary to reduce sodium intake from food and medications high in sodium; sometimes the use of GCS requires additional sodium).
Vaccines containing live viruses: during the period of use of immunosuppressive doses of GCS, viral replication and the development of viral diseases are possible; decreased antibody production (simultaneous use is not recommended).
Other vaccines: increased risk of neurological complications and decreased antibody production.
Folic acid: increased need for this drug.
Overdose
Overdose
The risk of overdose increases with long-term use of prednisolone, especially in large doses.
Symptoms: increased blood pressure, peripheral edema, increased undesirable effects described above.
Treatment: You should temporarily stop taking the drug or reduce the dose.
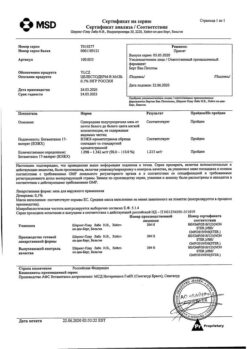
Shelf life
Shelf life
3 years.
Manufacturer
Manufacturer
Update of PFC JSC, Russia
Additional information
| Shelf life | 3 years. |
|---|---|
| Manufacturer | Update PFC AO, Russia |
| Medication form | solution |
| Brand | Update PFC AO |
Other forms…
Related products
Buy Prednisolone bufus, 30 mg/ml 1 ml 10 pcs with delivery to USA, UK, Europe and over 120 other countries.