No products in the cart.
Pradaxa, 150 mg capsules 180 pcs
€272.01 €226.67
Description
PRADAXA – dabigatran etexilate is a low molecular weight prodrug that has no pharmacological activity. After oral administration, it is rapidly absorbed and is converted to dabigatran by esterase-catalyzed hydrolysis. Dabigatran is an active, competitive, reversible direct thrombin inhibitor and acts mainly in plasma.
Since thrombin (a serine protease) converts fibrinogen to fibrin during the coagulation cascade, inhibition of its activity prevents thrombus formation. Dabigatran inhibits free thrombin, fibrin-binding thrombin and thrombin-induced platelet aggregation.
In vivo and ex vivo animal studies using various models of thrombosis have demonstrated the antithrombotic efficacy and anticoagulant activity of dabigatran after intravenous administration and dabigatran etexilate after oral administration.
A close correlation between the concentration of dabigatran in plasma and the severity of anticoagulant effect was revealed. Dabigatran prolongs activated partial thromboplastin time (ATTB).
Indications
Indications
Prevention of venous thromboembolism in patients after orthopedic surgery.
Pharmacological effect
Pharmacological effect
PRADAXA – dabigatran etexilate is a low molecular weight prodrug that does not have pharmacological activity. After oral administration, it is rapidly absorbed and is converted into dabigatran by hydrolysis catalyzed by esterases. Dabigatran is an active, competitive, reversible direct thrombin inhibitor and acts primarily in plasma.
Since thrombin (serine protease) converts fibrinogen into fibrin during the coagulation cascade, inhibition of its activity prevents the formation of a blood clot. Dabigatran inhibits free thrombin, fibrin-binding thrombin, and thrombin-induced platelet aggregation.
In vivo and ex vivo animal studies using various thrombosis models have demonstrated the antithrombotic efficacy and anticoagulant activity of dabigatran after intravenous administration and dabigatran etexilate after oral administration.
A close correlation was found between the plasma concentration of dabigatran and the severity of the anticoagulant effect. Dabigatran prolongs the activated partial thromboplastin time (aPTT).
Special instructions
Special instructions
Risk of hemorrhage: Unfractionated heparin can be used to preserve the functioning of a central venous or arterial catheter.
Active ingredient
Active ingredient
Dabigatran etexilate
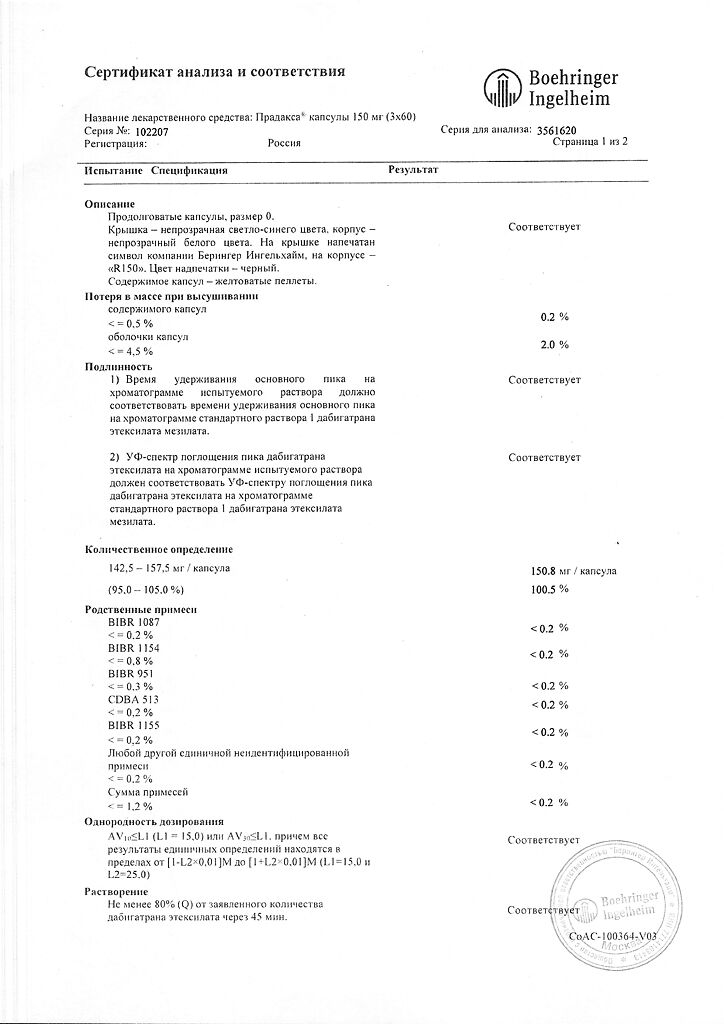
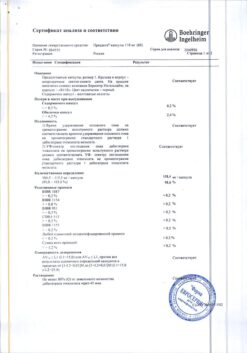
Composition
Composition
1 capsule:
Contraindications
Contraindications
Known hypersensitivity to dabigatran or dabigatran etexilate or to one of the excipients.
Patients with severe renal failure (creatinine clearance less than 30 ml/min).
Side Effects
Side Effects
Disorders of the hematopoietic and lymphatic system: anemia, thrombocytopenia.
Immune system disorders: hypersensitivity reactions, including urticaria, rash and itching, bronchospasm.
Nervous system disorders: intracranial bleeding.
Vascular disorders: hematoma, bleeding.
Respiratory, thoracic and mediastinal disorders: nosebleeds, hemoptysis.
Gastrointestinal disorders: gastrointestinal bleeding, rectal bleeding, hemorrhoidal bleeding, abdominal pain, diarrhea, dyspepsia, nausea, ulceration of the gastrointestinal mucosa, gastroesophagitis, gastroesophageal reflux disease, vomiting, dysphagia.
Disorders of the hepatobiliary system: increased activity of liver transaminases, impaired liver function, hyperbilirubinemia.
Changes in the skin and subcutaneous tissues: cutaneous hemorrhagic syndrome.
Musculoskeletal disorders, connective tissue and bone disorders: hemarthrosis.
Changes in the kidneys and urinary tract: urogenital bleeding, hematuria.
General disorders and changes at the injection site: bleeding from the injection site, bleeding from the catheter insertion site.
Damage, toxicity and complications from procedures: post-traumatic hematoma, bleeding from the surgical access site.
Vascular disorders: bleeding from the surgical wound.
General disorders and disorders at the injection site: spotting.
Damage, toxicity and complications of postoperative treatment: hematoma after wound treatment, bleeding after wound treatment, anemia in the postoperative period, discharge from the wound after procedures, secretion from the wound.
Surgical and therapeutic procedures: wound drainage, drainage after wound treatment.
Interaction
Interaction
Concomitant use of PRADAXA with drugs that affect hemostasis or the coagulation system, including vitamin K antagonists, may significantly increase the risk of bleeding.
Pharmacokinetic interactions
In vitro studies have not established an inducing or inhibitory effect of dabigatran on cytochrome P450. In in vivo studies in healthy volunteers, no interaction was observed between dabigatran etexilate and atorvastatin (CYP3A4 substrate) and diclofenac (CYP2C9 substrate).
Interactions with P-glycoprotein inhibitors/inducers:
The substrate for the transport molecule P-glycoprotein is dabigatran etexilate. The simultaneous use of P-glycoprotein inhibitors (amiodarone, verapamil, quinidine, ketoconazole for systemic use or clarithromycin) leads to an increase in the concentration of dabigatran in the blood plasma.
Concomitant use with P-glycoprotein inhibitors:
Dose selection in the case of using the listed P-glycoprotein inhibitors for the prevention of stroke, systemic thromboembolism and reduction of cardiovascular mortality in patients with atrial fibrillation is not required.
If used for the prevention of venous thromboembolism in patients after orthopedic surgery, see sections “Method of administration and dosage” and “Interaction with other drugs.”
Amiodarone. With simultaneous use of dabigatran etexilate with a single dose of amiodarone (600 mg) taken orally, the degree and rate of absorption of amiodarone and its active metabolite, desethylamiodarone, did not change. The AUC and Cmax values of dabigatran increased approximately 1.6-fold and 1.5-fold (60% and 50%), respectively.
In a study in patients with atrial fibrillation, dabigatran concentrations increased by no more than 14%, and no increased risk of bleeding was observed.
Dronedarone. After simultaneous use of dabigatran etexilate and dronedarone at a dose of 400 mg once,
The AUC0-∞ and Cmax of dabigatran increased by 2.1 and 1.9 times (by 114% and 87%), respectively, and after repeated use of dronedarone at a dose of 400 mg per day – by 2.4 and 2.3 (by 136% and 125%), respectively. After single and multiple doses of dronedarone, 2 hours after administration of dabigatran etexilate, AUC0-∞ increased by 1.3 and 1.6 times, respectively. Dronedarone had no effect on final T1/2 and renal clearance of dabigatran.
Verapamil. When dabigatran etexilate was co-administered with verapamil administered orally, the Cmax and AUC values of dabigatran increased depending on the time of administration and the dosage form of verapamil.
The greatest increase in the effect of dabigatran was observed with the first dose of immediate-release verapamil administered 1 hour before dosing with dabigatran etexilate (Cmax increased by 180% and AUC increased by 150%). This effect was progressively reduced when the sustained-release formulation of verapamil was used (Cmax increased by 90% and AUC increased by 70%), as well as when multiple doses of verapamil were used (Cmax increased by 60% and AUC increased by 50%), which may be explained by the induction of P-glycoprotein in the gastrointestinal tract with long-term use of verapamil.
When using verapamil 2 hours after taking dabigatran etexilate, no clinically significant interactions were observed (Cmax increased by 10% and AUC by 20%), since dabigatran is completely absorbed after 2 hours (see section “Dosage and Administration”).
In a study in patients with atrial fibrillation, dabigatran concentrations increased by no more than 21%, and no increased risk of bleeding was observed.
There are no data on the interaction of dabigatran etexilate with verapamil administered parenterally; no clinically significant interaction is expected.
Ketoconazole. Ketoconazole for systemic use after a single dose of 400 mg increases the AUC0-∞ and Cmax of dabigatran by approximately 2.4 times (by 138% and 135%), respectively, and after repeated administration of ketoconazole at a dose of 400 mg per day – by approximately 2.5 times (by 153% and 149%), respectively. Ketoconazole did not affect Tmax and final T1/2. The simultaneous use of PRADAXA and ketoconazole for systemic use is contraindicated.
Clarithromycin. When simultaneous use of clarithromycin at a dose of 500 mg 2 times a day with dabigatran etexilate, no clinically significant pharmacokinetic interaction was observed (Cmax increased by 15% and AUC by 19%).
Quinidine. The AUCτ,ss and Cmax,ss values of dabigatran when used 2 times a day in the case of simultaneous administration with quinidine at a dose of 200 mg every 2 hours until a total dose of 1000 mg were increased on average by 53% and 56%, respectively.
Concomitant use with P-glycoprotein substrates:
Digoxin. No pharmacokinetic interaction was observed with simultaneous use of dabigatran etexilate with digoxin, which is a P-glycoprotein substrate. Neither dabigatran nor the prodrug dabigatran etexilate are clinically significant P-gp inhibitors.
Concomitant use with P-glycoprotein inducers:
The simultaneous administration of PRADAXA and P-glycoprotein inducers should be avoided, since combined use leads to a decrease in the effect of dabigatran (see section “Special Instructions”).
Rifampicin. Pretreatment with the test inducer rifampicin at a dose of 600 mg per day for 7 days resulted in decreased exposure to dabigatran. After discontinuation of rifampicin, this inductive effect decreased; on day 7, the effect of dabigatran was close to the initial level. Over the next 7 days, no further increase in the bioavailability of dabigatran was observed.
It is expected that other P-glycoprotein inducers, such as St. John’s wort or carbamazepine, may also reduce plasma concentrations of dabigatran and should be used with caution.
Simultaneous use with antiplatelet agents
Acetylsalicylic acid (ASA). When studying the simultaneous use of dabigatran etexilate at a dose of 150 mg 2 times a day and acetylsalicylic acid (ASA) in patients with atrial fibrillation, it was found that the risk of bleeding may increase from 12% to 18% (using ASA at a dose of 81 mg) and up to 24% (using ASA at a dose of 325 mg). It has been shown that ASA or clopidogrel, used concomitantly with dabigatran etexilate at a dose of 110 mg or 150 mg 2 times a day, may increase the risk of major bleeding. Bleeding is also observed more often with the simultaneous use of warfarin with ASA or clopidogrel.
NSAIDs. NSAIDs (non-steroidal anti-inflammatory drugs) used for short-term analgesia after surgery did not increase the risk of bleeding when used simultaneously with dabigatran etexilate. Experience with long-term use of NSAIDs with a half-life of less than 12 hours with dabigatran etexilate is limited, and there is no evidence of an additional increase in the risk of bleeding.
Clopidogrel. It was found that the simultaneous use of dabigatran etexilate and clopidogrel does not lead to an additional increase in capillary bleeding time compared to clopidogrel monotherapy. In addition, it was shown that the AUCτ,ss and Cmax,ss values of dabigatran, as well as the blood coagulation parameters that were monitored to evaluate the effect of dabigatran (aPTT, ecarin clotting time or thrombin time (anti FIIa), as well as the degree of inhibition of platelet aggregation (the main indicator of the effect of clopidogrel) during combination therapy did not change compared with the corresponding indicators in monotherapy. When used “loading” dose of clopidogrel (300 or 600 mg), the AUCt,ss and Cmax,ss values of dabigatran increased by 30-40%.
Concomitant use with drugs that increase the pH of the stomach contents
Pantoprazole. When dabigatran etexilate and pantoprazole were co-administered, a 30% decrease in the AUC of dabigatran was observed. Pantoprazole and other proton pump inhibitors were used with dabigatran etexilate in clinical studies and no effect on bleeding risk or efficacy was observed.
Ranitidine. Ranitidine, when used concomitantly with dabigatran etexilate, did not have a significant effect on the degree of absorption of dabigatran.
The changes in the pharmacokinetic parameters of dabigatran identified during the population analysis under the influence of proton pump inhibitors and antacid drugs turned out to be clinically insignificant, since the severity of these changes was small (the decrease in bioavailability was not significant for antacids, but for proton pump inhibitors it was 14.6%). It was found that the simultaneous use of proton pump inhibitors is not accompanied by a decrease in the concentration of dabigatran and, on average, only slightly reduces the concentration of the drug in the blood plasma (by 11%). Therefore, concomitant use of proton pump inhibitors does not appear to lead to an increased incidence of stroke or systemic thromboembolism, especially when compared with warfarin, and therefore the decrease in dabigatran bioavailability caused by concomitant use of pantoprazole is probably not clinically significant.
Overdose
Overdose
An overdose when using the drug PRADAXA may be accompanied by hemorrhagic complications, which is due to the pharmacodynamic properties of the drug. If bleeding occurs, stop using the drug. Symptomatic treatment is indicated. There is no specific antidote.
Given the main route of elimination of dabigatran (renal), it is recommended to ensure adequate diuresis. Surgical hemostasis and replenishment of circulating blood volume (CBV) are performed. It is possible to use fresh whole blood or transfuse fresh frozen plasma. Since dabigatran has a low ability to bind to plasma proteins, the drug can be eliminated by hemodialysis, however, clinical experience with the use of dialysis in these situations is limited (see section “Pharmacokinetics”).
In case of an overdose of PRADAXA, it is possible to use concentrates of activated prothrombin complex or recombinant factor VIIa or concentrates of coagulation factors II, IX or X. There is experimental evidence to support the effectiveness of these agents in counteracting the anticoagulant effect of dabigatran, but no specific clinical studies have been conducted.
In the event of thrombocytopenia, or when using long-acting antiplatelet agents, the use of platelet mass may be considered.
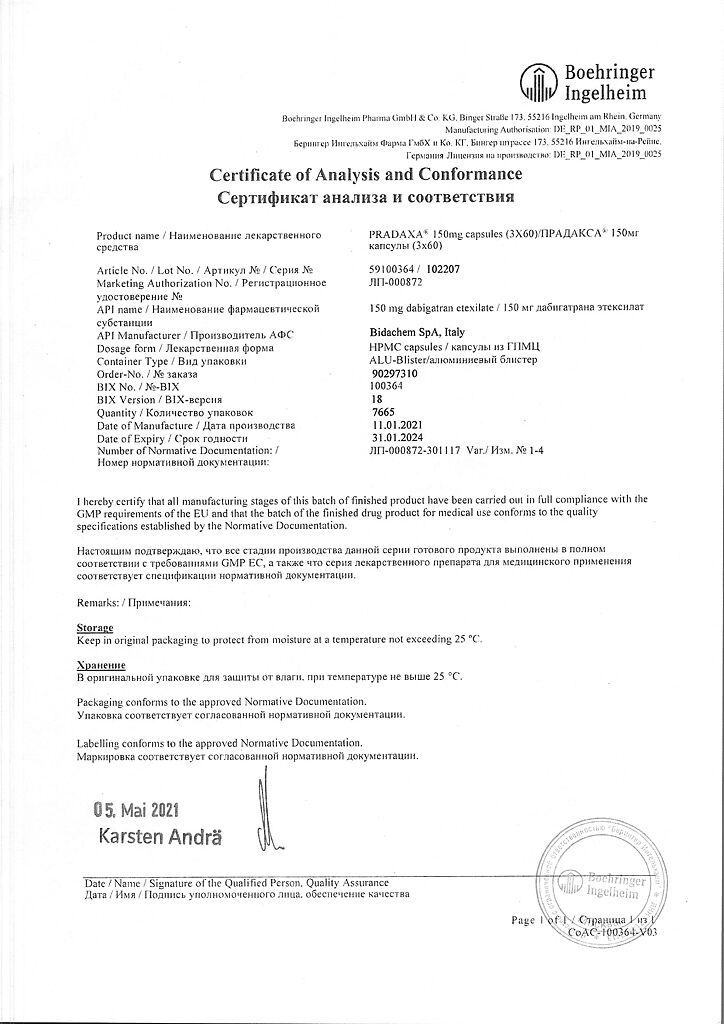
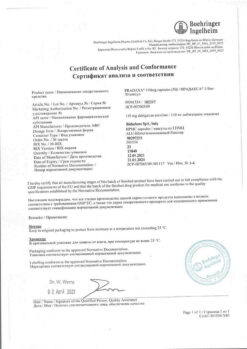
Storage conditions
Storage conditions
Store in a dry place, at a temperature not exceeding 25º C.
Shelf life
Shelf life
3 years.
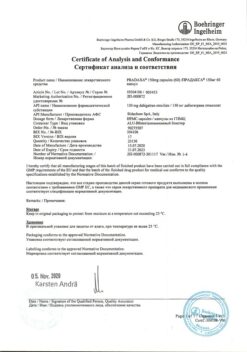
Manufacturer
Manufacturer
Boehringer Ingelheim Pharma GmbH & Co.KG, Germany
Additional information
| Shelf life | 3 years. |
|---|---|
| Conditions of storage | Store in a dry place at a temperature not exceeding 25º C. |
| Manufacturer | Boehringer Ingelheim Pharma GmbH & Co. |
| Medication form | capsules |
| Brand | #Н/Д |
Other forms…
Related products
Buy Pradaxa, 150 mg capsules 180 pcs with delivery to USA, UK, Europe and over 120 other countries.