No products in the cart.
Plakvenil, 200 mg 60 pcs
€13.02 €10.85
Description
Plaquenil has:
- antiprotozoal action – inhibits the activity of protozoa that cause infectious diseases; this primarily concerns the causative agents of malaria, so the main action of the drug is anti-malarial;
- immunosuppressive action – suppresses the immune system overreaction, including allergy to the patient’s own tissues;
- inflammatory action – suppresses inflammatory reactions.
Plakvenil belongs to the group of antimalarial and immunosuppressive drugs from the group of 4-aminoquinoline derivatives. Its mechanism of action is not well studied, but it is thought to be associated with the following properties of this drug:
- Abstress of toxic free radicals produced during metabolism (antioxidant effect).
- Abstress of enzymes which cause breakdown of cartilage tissue.
- The ability to inhibit the synthesis of those types of cytokines (hormone-like proteins synthesized by cells to affect other cells) that activate immunity. This also helps to reduce autoimmune processes (destruction of the body’s own tissues by immune processes).
- Ability to suppress the activity of lymphocytes involved in immune reactions.
- Ability to suppress the formation of rheumatoid factor – immunoglobulins (antibodies) that perceive the body’s own tissues as foreign structures (antigens) and destroy them.
- The antimalarial properties of Plaquenil is to suppress the activity of causative agents of three-day malaria, four-day malaria, malaria-oval, as well as its sensitive forms of tropical malaria pathogens (most tropical malaria pathogens are not sensitive to Plaquenil).
After taking Plaquenil tablet its active substance is quickly and almost completely absorbed and enters the blood, and then it accumulates in high concentrations in various organs and tissues. The maximum concentration of the active substance in the blood plasma is reached within approximately 100 minutes.
The drug is broken down in the liver into active and inactive metabolic products (metabolites) and is excreted with the urine, but partially with the feces. The active substance Plakvenil penetrates the placenta and is excreted with the mother’s milk. The drug is excreted slowly, it disappears from the blood plasma not earlier than in a month.
Indications
Indications
Rheumatoid arthritis; systemic lupus erythematosus, malaria.
Active ingredient
Active ingredient
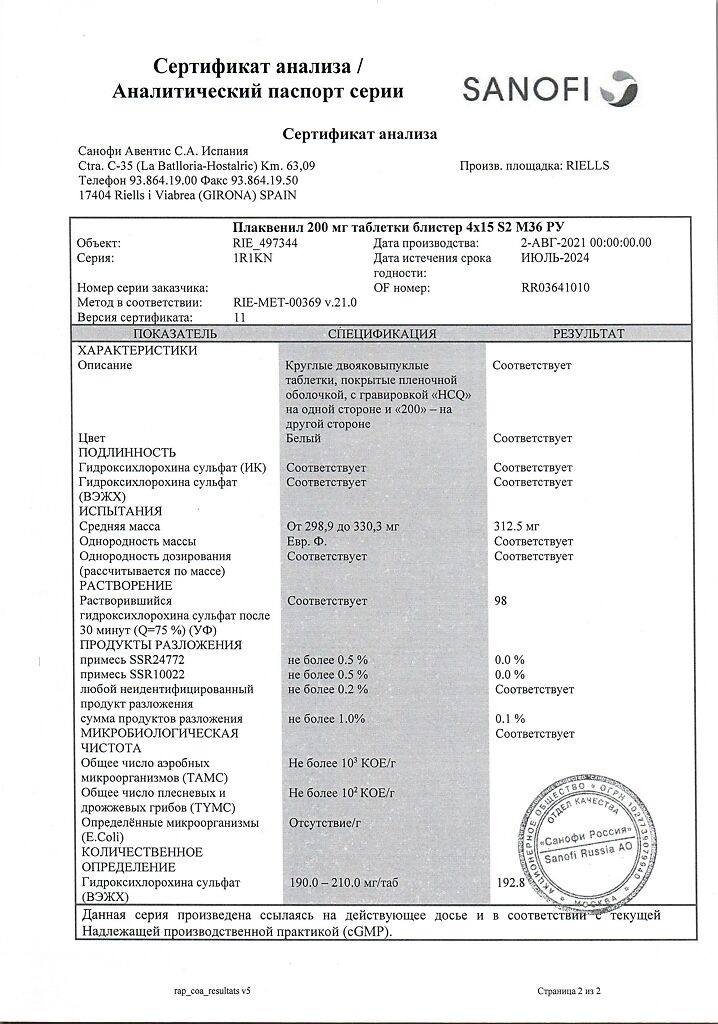
Composition
Composition
Active ingredient:
Hydroxychloroquine sulfate 200 mg;
Ancillary substances:
Lactose monohydrate,
povidone K25,
corn starch,
p> magnesium stearate,
opadray OY-L-28900 (hypromellose, macrogol 4000, titanium dioxide (E171), lactose monohydrate).
How to take, the dosage
How to take, the dosage
Note: All doses are given for hydroxychloroquine sulfate and are not equivalent to those for base.
Ingestion with meals or with a glass of milk.
The treatment of RA. Hydroxychloroquine has cumulative activity. For the manifestation of its therapeutic effect it is necessary to take the drug for several weeks, while the side effects may appear relatively early. The necessary therapeutic effect develops after several months of taking the drug. If there is no objective improvement in the patient’s condition within 6 months of taking hydroxychloroquine, the drug should be discontinued.
Adults (including the elderly) should take the minimum effective dose. They should not exceed 6.5 mg/kg/day (calculated by “ideal” body weight, not real body weight) and may be either 200 or 400 mg/day.
In patients able to take 400 mg daily
Initially, 400 mg daily, in multiple doses. When improvement is evident, the dose may be reduced to 200 mg. If the effect diminishes, the maintenance dose may be increased to 400 mg.
In children. The minimum effective dose should be used. The dose should not exceed 6.5 mg/kg (based on “ideal” body weight). Therefore, 200 mg tablets are not suitable for children with an “ideal” body weight of less than 31 kg.
The use of Plakvenil for combination therapy of RA. Plakvenil can be safely used in combination with GCS, salicylates, NSAIDs, methotrexate and other second-line therapeutic agents. After several weeks of use of Plaquenil, doses of GCS and salicylates may be reduced or the use of these drugs may be discontinued. Doses of GCS should be gradually reduced every 4-5 days: cortisone dose by no more than 5-15 mg, hydrocortisone dose by no more than 5-10 mg, prednisolone and prednisone doses by no more than 1-2.5 mg, methylprednisolone and triamcinolone doses by no more than 1-2 mg and dexamethasone doses by no more than 0.25-0.5 mg.
The treatment of SLE. The initial average dose in adults is 400 mg 1 or 2 times a day. It should be administered for several weeks or months, depending on the patient’s response. For long-term maintenance therapy, a lower dose of 200 to 400 mg is sufficient.
Treatment of malaria
Prevention of acute malaria attacks caused by P. malariae and sensitive strains of Plasmodium falciparum
Adults – 400 mg weekly on the same day of the week.
In children, the weekly dose is 6.5 mg/kg (the “ideal” body weight is taken for calculation), but regardless of body weight it should not exceed the dose for adults.
If conditions allow, prophylactic therapy should be started 2 weeks before entering the endemic zone. If this is not possible, an initial double (loading) dose may be prescribed: 800 mg in adults, 12.9 mg/kg of “ideal” body weight in children (but no more than 800 mg), divided into two doses with a 6-hour interval. Prophylactic treatment should be continued for 8 weeks after leaving the endemic zone.
Treatment of acute malaria attacks
For adults, the initial dose of 800 mg is followed by a dose of 400 mg at 6 or 8 hours, and then by 400 mg on 2 subsequent days (total of 2 g of hydroxychloroquine sulfate).
An alternative route of treatment: a single dose of 800 mg has also been shown to be effective.
Doses for adults can also be calculated by “ideal” body weight, similar to the calculation of doses in children (see below).
For children, a total dose of 32 mg/kg of “ideal” body weight (but no more than 2 g) is administered over 3 days as follows:
The first dose is 12.9 mg/kg (a single dose of no more than 800 mg); the second dose is 6.5 mg/kg (no more than 400 mg) 6 hours after the first; the third dose is 6.5 mg/kg (no more than 400 mg) 18 hours after the second dose;the fourth dose is 6.5 mg/kg (no more than 400 mg) 24 hours after the third dose.
Radical treatment of malaria caused by Plasmodium malariae and Plasmodium vivax
The radical treatment of malaria caused by Plasmodium malariae and Plasmodium vivax requires simultaneous administration of 8-aminoquinolone derivatives.
Interaction
Interaction
Digoxin. It has been reported that hydroxychloroquine can increase plasma concentrations of digoxin, therefore, to avoid the development of glycoside intoxication when taking these drugs simultaneously, the dose of digoxin should be reduced while monitoring its plasma concentrations.
Drugs used to treat diabetes mellitus. Since hydroxychloroquine may potentiate the effects of insulin and oral hypoglycemic agents, doses of these hypoglycemic drugs may need to be reduced when starting hydroxychloroquine.
Antacids. May decrease absorption of hydroxychloroquine. Therefore in concomitant use of antacids and hydroxychloroquine the interval between their administration should be at least 4 hours.
Hydroxychloroquine also has the following interactions with other drugs that have been described for chloroquine, but have not yet been observed with hydroxychloroquine.
The aminoglycosides. Potentiation of their direct blocking effect on neuromuscular transmission.
Cimetidine. Suppresses the metabolism of antimalarials, which may increase their plasma concentrations and increase the risk of their side effects, especially toxic.
Neostigmine and pyridostigmine. Antagonism of action.
Any human intradermal diploid cell rabies vaccine. Reduced antibody formation in response to primary immunization with human intradermal diploid cell rabies vaccine.
Special Instructions
Special Instructions
The toxic effects on the retina are largely dose-dependent. The incidence of retinopathy at doses up to 6.5 mg/kg of “ideal” body weight is small. Exceeding the recommended daily dose dramatically increases the risk of retinopathy and accelerates its occurrence.
Before starting a long-term course of treatment with the drug, both eyes should be thoroughly examined. The examination should include determination of visual acuity, fundus examination, and evaluation of color vision and visual fields. During therapy such examination should be performed at least once every 6 months.
The exam should be more frequent in the following situations:
If any visual impairment occurs (decreased visual acuity, change in color vision), the drug should be stopped immediately and the patient’s visual condition should be closely monitored, because retinal changes (and visual impairment) can progress even after the drug is stopped.
We recommend caution when prescribing hydroxychloroquine to patients with liver and kidney disease in which doses of the drug may need to be reduced, as well as due to the possibility of the drug affecting the function of these organs (in severe renal or liver function disorders the dose should be adjusted under control of plasma concentrations of hydroxychloroquine).
In patients receiving long-term treatment, periodic complete blood counts should be performed; if hematological abnormalities occur, hydroxychloroquine should be discontinued.
Children are particularly sensitive to the toxic effects of 4-aminoquinolines, so care should be taken to ensure that hydroxychloroquine is stored out of the reach of children.
All patients receiving the drug for a long time should be periodically examined by a neurologist regarding skeletal muscle function and severity of tendon reflexes. If muscle weakness occurs, the drug should be discontinued.
In malaria
. Plaquenil is ineffective against chloroquine-resistant strains of Plasmodium falciparum and inactive against extra-erythrocytic forms of Plasmodium vivax, Plasmodium malariae and Plasmodium ovale and therefore cannot prevent infection with these microorganisms when prescribed for the prevention of acute attacks of malaria, and cannot prevent relapse of disease caused by these pathogens.
The effect on the ability to drive and perform hazardous work.Patients should exercise caution when driving or performing work that requires extra attention, because hydroxychloroquine can impair accommodation and clarity of vision. If this condition does not go away on its own, the dose may be temporarily reduced.
Contraindications
Contraindications
Side effects
Side effects
Visually: retinopathy with pigmentation changes and visual field defects may develop, although rarely. In the early form, these phenomena are usually reversible after discontinuation of hydroxychloroquine. If the condition remains undiagnosed and retinal lesions continue to develop further, there may be a risk of progression even after discontinuation of the drug.
The retinal changes may initially be asymptomatic, or manifest as paracentral or pericentral scotomas, transient scotomas, and color vision disturbances.
Corneal changes, including edema and opacity, are possible. They may be asymptomatic or cause visual disturbances such as halos, blurred vision, or photophobia. These changes may reverse when treatment is stopped.
Extremely dose-dependent and reversible visual disturbances associated with accommodation disorders may also occur.
Skin disorders: sometimes there are skin rashes; pruritus, changes in pigmentation of the skin and mucous membranes, hair discoloration and alopecia have also been described. These changes usually disappear rapidly after discontinuation of treatment. The development of bullous rash has been reported, including very rare cases of erythema multiforme and Stevens-Johnson syndrome, photosensitivity and isolated cases of exfoliative dermatitis.
The very rare cases of acute generalized exanthematous pustulosis (OGEP) must be distinguished from psoriasis, although hydroxychloroquine can also provoke an exacerbation of psoriasis. OGEP may be accompanied by fever and hyperleukocytosis. After withdrawal of the drug, the outcome is usually favorable.
Gastrointestinal side: nausea, diarrhea, anorexia, abdominal pain and rarely vomiting. These symptoms usually go away immediately after reducing the dose or discontinuing the drug.
Hepatobiliary system disorders: with long-term use in high doses the development of hepatotoxic effect is possible. There are reports about single cases of liver dysfunction and several cases of sudden liver failure.
CNS disorders: infrequent dizziness, tinnitus, hearing loss, headache, irritability, emotional instability, psychosis, seizures, muscle weakness, ataxia.
Peripheral nervous system and muscle disorders: cases of skeletal muscle myopathy or neuromyopathy leading to progressive weakness and atrophy of proximal muscle groups have been reported. Myopathy may be reversible after drug withdrawal, but full recovery may take several months. Simultaneous weak sensory changes, suppression of tendon reflexes, and decreased nerve conduction may occur.
Cardiovascular system: there are rare reports of the development of cardiomyopathy.
Chronic cardiac toxicity may be suspected if conduction abnormalities (Gis bundle leg block/ AV conduction abnormality) or hypertrophy of both ventricles are detected. If the drug is withdrawn, reversal of these changes is possible.
Hematopoietic organs: rare cases of suppression of medullary hematopoiesis have been reported. Rare cases of anemia, including aplastic anemia, agranulocytosis, leukopenia and thrombocytopenia have been reported.
Hydroxychloroquine may provoke or cause exacerbation of porphyria.
Immune system disorders: urticaria, angioneurotic edema, bronchospasm.
Overdose
Overdose
A 4-Aminoquinolines overdose is especially dangerous in children, even 1-2 g of the drug can be fatal.
Symptoms: headache, visual disturbances, collapse, seizures, hypokalemia, rhythm and conduction disorders, followed by cardiac and respiratory arrest.
Treatment: because these effects can develop very quickly after taking a large dose of the drug, appropriate measures should be initiated immediately in these cases. Induction of vomiting or gastric lavage through a tube should be performed immediately. To slow absorption, administration of activated charcoal in a dose at least 5 times the dose taken. Parenteral administration of diazepam is reasonable (a decrease in cardiotoxicity of chloroquine against its background has been described).
If necessary, artificial lung ventilation and antishock therapy should be performed.
After symptoms of overdose have resolved, continued continuous medical observation for at least 6 h is required.
Pregnancy use
Pregnancy use
Hydroxychloroquine penetrates the placenta. Data are limited with regard to its use during pregnancy. It should be noted that 4-aminoquinolines in therapeutic doses may cause intrauterine damage to the CNS, including the auditory nerve (hearing and vestibular disorders, congenital deafness), retinal hemorrhages and abnormal retinal pigmentation.
Hydroxychloroquine should therefore be avoided during pregnancy unless the potential benefit to the mother outweighs the risk to the fetus.
The necessity of using the drug during breastfeeding should be carefully weighed, since it has been shown to be excreted in small amounts into the mother’s milk, and young children are particularly sensitive to the toxic effects of 4-aminoquinolines.
Similarities
Similarities
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C |
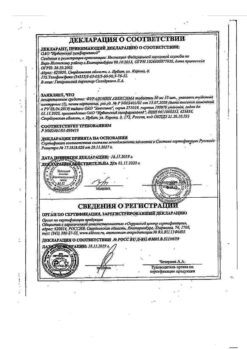
| Manufacturer | Sanofi-Aventis S.A., Spain |
| Medication form | pills |
| Brand | Sanofi-Aventis S.A. |
Related products
Buy Plakvenil, 200 mg 60 pcs with delivery to USA, UK, Europe and over 120 other countries.