No products in the cart.
Physiotensis, 0.2 mg 28 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Moxonidine is a hypotensive agent with a central mechanism of action. In brain stem structures (rostral layer of lateral ventricles) moxonidine selectively stimulates imidazoline-sensitive receptors participating in tonic and reflex regulation of sympathetic nervous system. Stimulation of imidazoline receptors decreases peripheral sympathetic activity and blood pressure (BP).
Moxonidine differs from other sympatholytic hypotensive agents in its lower affinity for a2-adrenoreceptors, which explains the lower likelihood of developing sedation and dry mouth.
The administration of moxonidine leads to a decrease in systemic vascular resistance and BP. The hypotensive effect of moxonidine has been confirmed in double-blind, placebo-controlled, randomized trials.
Moxonidine improves insulin sensitivity index by 21% (compared to placebo) in patients with obesity, insulin resistance and moderate arterial hypertension.
Pharmacokinetics
Intake:
After oral administration, moxonidine is rapidly and almost completely absorbed in the upper gastrointestinal tract. Absolute bioavailability is approximately 88%. Time of reaching maximum concentration is about 1 hour. Food intake has no effect on the pharmacokinetics of the drug.
Distribution
The binding to plasma proteins is 7.2%.
Metabolism
The main metabolite is dehydrated moxonidine. The pharmacodynamic activity of dehydrated moxonidine is about 10% compared to moxonidine.
Elimation
The half-life (T1/2) of moxonidine and the metabolite is 2.5 and 5 hours, respectively. Within 24 hours more than 90% of moxonidine is excreted by the kidneys (about 78% unchanged and 13% as dehydroromoxonidine, other metabolites in the urine do not exceed 8% of the dose taken). Less than 1% of the dose is excreted through the intestine.
Pharmacokinetics in patients with arterial hypertension:
In comparison with healthy volunteers, patients with arterial hypertension show no changes in pharmacokinetics of moxonidine.
Pharmacokinetics in the elderly
Clinically insignificant changes in pharmacokinetic parameters of moxonidine have been noted in elderly patients, probably due to decreased metabolic rate and/or slightly higher bioavailability.
Pharmacokinetics in children
Moxonidine is not recommended for use in persons younger than 18 years of age; therefore, no pharmacokinetic studies have been performed in this group.
Pharmacokinetics in renal failure
The excretion of moxonidine is highly correlated with creatinine clearance (CK). In patients with moderate renal insufficiency (CK between 30-60 ml/min), equilibrium plasma concentrations and final T1/2 are approximately 2 and 1.5 times higher than in those with normal renal function (CK greater than 90 ml/min). In patients with severe renal insufficiency (CKD less than 30 ml/min), equilibrium plasma concentrations and final T1/2 are 3 times higher than in patients with normal renal function. Administration of repeated doses of moxonidine results in predictable cumulation in patients with moderate to severe renal impairment.
In patients with terminal renal failure (KC less than 10 ml/min) on hemodialysis, equilibrium plasma concentrations and final T1/2 are, respectively, 6 and 4 times higher than in patients with normal renal function. In all groups, the maximum plasma concentration of moxonidine is 1.5 to 2 times higher. In patients with impaired renal function the dosage should be selected individually. Moxonidine is slightly excreted during hemodialysis.
Indications
Indications
Arterial hypertension.
Pharmacological effect
Pharmacological effect
Moxonidine is an antihypertensive drug with a central mechanism of action. In the brain stem structures (rostral layer of the lateral ventricles), moxonidine selectively stimulates imidazoline-sensitive receptors that take part in the tonic and reflex regulation of the sympathetic nervous system. Stimulation of imidazoline receptors reduces peripheral sympathetic activity and blood pressure (BP).
Moxonidine differs from other sympatholytic antihypertensive drugs in its lower affinity for α2-adrenergic receptors, which explains the lower likelihood of developing sedation and dry mouth.
Taking moxonidine leads to a decrease in systemic vascular resistance and blood pressure. The hypotensive effect of moxonidine has been confirmed in double-blind, placebo-controlled, randomized studies.
Moxonidine improves the insulin sensitivity index by 21% (compared to placebo) in patients with obesity, insulin resistance and moderate hypertension.
Pharmacokinetics
Suction:
After oral administration, moxonidine is rapidly and almost completely absorbed from the upper gastrointestinal tract. Absolute bioavailability is approximately 88%. The time to reach maximum concentration is about 1 hour. Food intake does not affect the pharmacokinetics of the drug.
Distribution
The binding to plasma proteins is 7.2%.
Metabolism
The main metabolite is dehydrogenated moxonidine. The pharmacodynamic activity of dehydrogenated moxonidine is about 10% compared to moxonidine.
Removal
The half-life (T1/2) of moxonidine and metabolite is 2.5 and 5 hours, respectively. Within 24 hours, over 90% of moxonidine is excreted by the kidneys (about 78% unchanged and 13% as dehydriromoxonidine, other metabolites in the urine do not exceed 8% of the dose taken). Less than 1% of the dose is excreted through the intestines.
Pharmacokinetics in patients with arterial hypertension:
Compared with healthy volunteers, patients with arterial hypertension show no changes in the pharmacokinetics of moxonidine.
Pharmacokinetics in old age
Clinically insignificant changes in the pharmacokinetic parameters of moxonidine were noted in elderly patients, probably due to a decrease in the intensity of its metabolism and/or slightly higher bioavailability.
Pharmacokinetics in children
Moxonidine is not recommended for use in persons under 18 years of age, and therefore no pharmacokinetic studies have been conducted in this group.
Pharmacokinetics in renal failure
Moxonidine excretion is significantly correlated with creatinine clearance (CC). In patients with moderate renal failure (creatinine clearance in the range of 30-60 ml/min.), equilibrium plasma concentrations and final T1/2 are approximately 2 and 1.5 times higher than in individuals with normal renal function (creatinine clearance more than 90 ml/min.). In patients with severe renal failure (creatinine clearance less than 30 ml/min.), steady-state plasma concentrations and final T1/2 are 3 times higher than in patients with normal renal function. The administration of multiple doses of moxonidine leads to predictable accumulation in the body of patients with moderate and severe renal failure.
In patients with end-stage renal failure (creatinine clearance less than 10 ml/min) on hemodialysis, steady-state plasma concentrations and final T1/2 are 6 and 4 times higher, respectively, than in patients with normal renal function. In all groups, the maximum concentration of moxonidine in blood plasma was 1.5 – 2 times higher. In patients with impaired renal function, the dosage should be adjusted individually. Moxonidine is excreted to a small extent during hemodialysis.
Special instructions
Special instructions
If it is necessary to cancel simultaneously taken beta-blockers and the drug Physiotens, first cancel the beta-blockers and, only after a few days, Physiotens®.
During treatment, regular monitoring of blood pressure, heart rate and ECG is necessary. You should stop taking Physiotens gradually.
Influence on the ability to drive a car and control machines and mechanisms
Studies of the effect of the drug on the ability to drive a car and other mechanisms have not been conducted.
There are reports of drowsiness and dizziness during treatment with moxonidine. This should be taken into account when performing the above steps.
Active ingredient
Active ingredient
Moxonidine
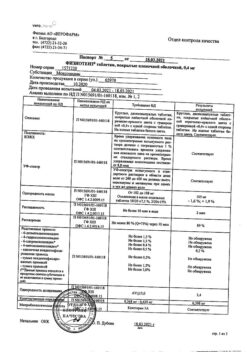
Composition
Composition
Active substance:
Moxonidine 0.2 mg.
Excipients:
lactose monohydrate – 95.80 mg,
povidone – 0.70 mg,
crospovidone – 3.00 mg,
magnesium stearate – 0.30 mg.
Shell: hypromellose – 1.30 mg, ethylcellulose – 1.20 mg, macrogol – 0.25 mg, talc – 0.9975 mg, red iron oxide dye (E 172) – 0.0025 mg, titanium dioxide (E 171) – 1.25 mg.
Pregnancy
Pregnancy
Pregnancy: There are no clinical data on the use of the drug Physiotens® in pregnant women. In animal studies, the embryotoxic effect of the drug was established. Physiotens® should be prescribed to pregnant women only after a careful assessment of the risk-benefit ratio, when the benefit to the mother outweighs the potential risk to the fetus.
Breastfeeding: Moxonidine passes into breast milk and should therefore not be administered during breastfeeding. If it is necessary to use the drug Physiotens® during lactation, breastfeeding must be stopped.
Contraindications
Contraindications
Hypersensitivity to the active substance and other components of the drug; sick sinus syndrome, severe bradycardia (resting heart rate (HR) less than 50 beats/min).
Hereditary galactose intolerance, lactase deficiency or glucose-galactose malabsorption.
Due to the lack of data on safety and effectiveness, it is not recommended to prescribe moxonidine to persons under 18 years of age.
With caution: severe and terminal renal failure; patients on hemodialysis; due to lack of experience in use – severe liver failure (more than 9 points according to the Child-Pug classification).
Side Effects
Side Effects
From the central nervous system: Often (1-10%): headache, dizziness, drowsiness. Uncommon (<1%): insomnia.
From the cardiovascular system: Rarely (<0.1%): excessive decrease in blood pressure, orthostatic hypotension.
From the gastrointestinal tract: Often (1-10%): dry mouth. Uncommon (<1%): nausea.
From the skin and subcutaneous tissue: Uncommon (<1%): skin rash, itching. Very rare (<0.01%): angioedema.
General: Often (1-10%): asthenia.
The most common side effects in patients taking moxonidine are dry mouth, headache, dizziness, asthenia and drowsiness. These symptoms often improve after the first weeks of therapy.
Interaction
Interaction
Moxonidine can be prescribed with thiazide diuretics, slow calcium channel blockers and other antihypertensive drugs. The combined use of moxonidine with these and other antihypertensive drugs leads to an additive effect.
When prescribing moxonidine with hydrochlorothiazide, glibenclamide or digoxin, no pharmacokinetic interaction was detected.
Tricyclic antidepressants may reduce the effectiveness of centrally acting antihypertensive drugs, and therefore their use together with moxonidine is not recommended.
Moxonidine may moderately improve impaired cognitive function in patients receiving lorazepam.
Prescribing moxonidine together with benzodiazepines may be accompanied by an increase in the sedative effect of the latter.
When moxonidine is prescribed together with moclobemide, there is no pharmacodynamic interaction.
Overdose
Overdose
There have been reports of several cases of non-fatal overdose when doses up to 19.6 mg were used simultaneously.
Symptoms:
headache, sedation, drowsiness, marked decrease in blood pressure, dizziness, fatigue, asthenia, bradycardia, dry mouth, vomiting and pain in the epigastric region. A short-term increase in blood pressure, tachycardia, and hyperglycemia are also potentially possible.
Treatment:
There is no specific antidote. In case of a decrease in blood pressure, it is recommended to restore circulating blood volume by administering fluids and administering dopamine.
Bradycardia can be relieved with atropine.
Alpha-adrenergic antagonists may reduce or eliminate the paradoxical hypertensive effects of moxonidine overdose.
Shelf life
Shelf life
1 year
Manufacturer
Manufacturer
Nobel Almaty Pharmaceutical Factory JSC, Kazakhstan
Additional information
| Shelf life | 1 year |
|---|---|
| Manufacturer | Nobel Almaty Pharmaceutical Factory JSC, Kazakhstan |
| Medication form | pills |
| Brand | Nobel Almaty Pharmaceutical Factory JSC |
Other forms…
Related products
Buy Physiotensis, 0.2 mg 28 pcs with delivery to USA, UK, Europe and over 120 other countries.