No products in the cart.
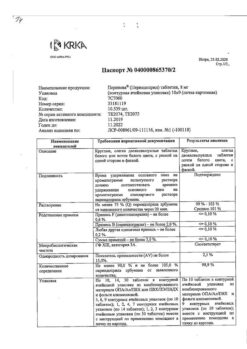
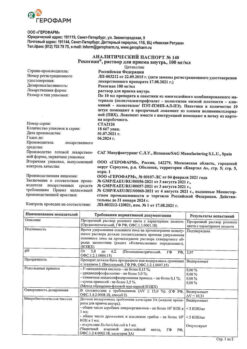
Perineva, tablets 4 mg 90 pcs
€13.81 €11.51
Description
Dyspnea, Prevention of heart attacks and strokes, Angina, Hypertension (high blood pressure), Heart failure, Cardialgia (heart pain), Edema
– Arterial hypertension.
– Chronic heart failure.
– Prevention of recurrent stroke (combined therapy with indapamide) in patients who have had a stroke or transient ischemic cerebral circulation disorder.
– Stable IBS: reduction in risk of cardiovascular complications in patients with stable IBS.
Indications
Indications
· Arterial hypertension.
· Chronic heart failure.
· Prevention of recurrent stroke (combination therapy with indapamide) in patients who have suffered a stroke or transient ischemic cerebrovascular accident.
· Stable coronary artery disease: reducing the risk of cardiovascular complications in patients with stable coronary artery disease.
Pharmacological effect
Pharmacological effect
angiotensin-converting enzyme (ACE) inhibitor
Special instructions
Special instructions
(see also sections “Interaction with other drugs”, “Special instructions”)
Bilateral renal artery stenosis, the presence of only one functioning kidney, renal failure, systemic connective tissue diseases (systemic lupus erythematosus, scleroderma, etc.), therapy with immunosuppressants, allopurinol, procainamide (risk of developing neutropenia, agranulocytosis), reduced circulating blood volume (CBV) (taking diuretics, salt-free diet, vomiting, diarrhea), angina pectoris, cerebrovascular diseases, renovascular hypertension, diabetes mellitus, CHF IV functional class according to the NYHA classification, simultaneous use of potassium-sparing diuretics, potassium preparations, potassium-containing table salt substitutes, lithium preparations, hyperkalemia, surgery/general anesthesia, hemodialysis using high-flow membranes, desensitizing therapy, low-density lipoprotein (LDL) apheresis, condition after kidney transplantation, aortic stenosis/mitral stenosis/hypertrophic obstructive cardiomyopathy (HOCM), use in black patients, congenital deficiency of glucose-6-phosphate dehydrogenase.
Perineva® should not be used in children and adolescents under 18 years of age, as there is no data on the effectiveness and safety of perindopril in patients in this age group.
In elderly patients, treatment should begin with a dose of 2 mg per day. If necessary, one month after the start of therapy, the dose can be increased to 4 mg per day, and then to a maximum dose of 8 mg per day, taking into account the state of renal function (see Table 1).
The maximum daily dose is 8 mg.
Kidney failure
In patients with renal failure, the dose of Perineva® should be adjusted taking into account creatinine clearance (CC).
Table 1. Dosage of Perineva® for renal failure
CC (ml/min)
Recommended dose
≥ 60
4 mg per day
? 30 and < 60
2 mg per day
? 15 and < 30
2 mg every other day
< 15 (hemodialysis patients*)
2 mg per day of dialysis
Active ingredient
Active ingredient
Perindopril
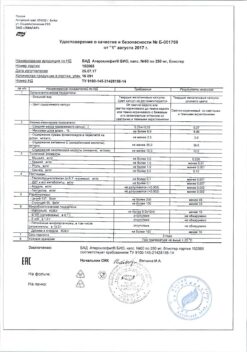
Composition
Composition
1 tablet 2 mg/4 mg/8 mg contains:
Active ingredient:
Perindopril erbumine 2,000 mg/4,000 mg/8,000 mg
Excipients:
Calcium chloride hexahydrate, lactose monohydrate, crospovidone, microcrystalline cellulose, colloidal silicon dioxide, magnesium stearate
Pregnancy
Pregnancy
Pregnancy
Perineva® is contraindicated for use during pregnancy (see section “Contraindications”).
If you are planning pregnancy or if it occurs while using Perineva®, you should immediately stop taking the drug and, if necessary, prescribe other antihypertensive therapy with a proven safety profile for use during pregnancy.
It is known that the effect of ACE inhibitors on the fetus in the second and third trimesters of pregnancy can lead to disruption of its development (decreased renal function, oligohydramnios, delayed ossification of the skull bones) and the development of complications in the newborn (renal failure, arterial hypotension, hyperkalemia).
If the patient received ACE inhibitors in the second or third trimester of pregnancy, it is recommended to conduct an ultrasound examination of the newborn to assess the condition of the skull bones and kidney function.
Breastfeeding period
It is not known whether perindopril passes into breast milk. In this regard, the use of Perineva® during breastfeeding is contraindicated.
If the use of Perineva® is necessary during breastfeeding, then breastfeeding should be discontinued.
Fertility
Preclinical studies have shown no effect of perindopril on reproductive function in rats of both sexes.
Contraindications
Contraindications
· Hypersensitivity to the active substance, other ACE inhibitors and excipients (see section “Composition”) included in the drug.
· Lactase deficiency, lactose intolerance, glucose-galactose deficiency syndrome (Perineva® contains lactose).
· Hereditary/idiopathic angioedema.
· History of angioedema (Quincke’s edema) associated with taking an ACE inhibitor.
· Significant bilateral renal artery stenosis or stenosis of the artery of a single functioning kidney.
· Concomitant use with aliskiren and drugs containing aliskiren in patients with diabetes mellitus and/or with moderate or severe renal impairment (GFR < 60 ml/min/1.73 m2 body surface area) (see sections “Special instructions”, “Interaction with other drugs”).
· Concomitant use with angiotensin II receptor antagonists (ARA II) in patients with diabetic nephropathy.
· Concomitant use with neutral endopeptidase inhibitors (for example, with drugs containing sacubitril) due to the high risk of developing angioedema.
· Extracorporeal treatments that bring blood into contact with negatively charged surfaces.
· Pregnancy (see section “Use during pregnancy and breastfeeding”).
· Breastfeeding period (see section “Use during pregnancy and breastfeeding”).
· Age under 18 years (efficacy and safety have not been established).
Side Effects
Side Effects
The safety profile of perindopril is consistent with the safety profile of ACE inhibitors.
The most common adverse events reported in clinical studies and observed with perindopril are: dizziness, headache, paresthesia, vertigo, visual disturbances, tinnitus, marked decrease in blood pressure, cough, shortness of breath, abdominal pain, constipation, diarrhea, taste disturbance, dyspepsia, nausea, vomiting, itching, skin rash, spasm muscles and asthenia.
Classification of the frequency of side effects recommended by the World Health Organization (WHO):
very common ≥ 1/10
often ≥ 1/100 to < 1/10
uncommon ≥ 1/1000 to < 1/100
rarely from ≥ 1/10000 to < 1/1000
very rare <1/10000
frequency unknown cannot be estimated from available data.
Blood and lymphatic system disorders:
uncommon*: eosinophilia;
very rare: decreased hemoglobin and hematocrit, thrombocytopenia, leukopenia/neutropenia, agranulocytosis, pancytopenia, hemolytic anemia in patients with congenital deficiency of glucose-6-phosphate dehydrogenase (see section “Special Instructions”).
Metabolic and nutritional disorders:
uncommon*: hypoglycemia (see sections “Interaction with other drugs”, “Special instructions”), hyperkalemia, reversible after discontinuation of the drug (see section “Special instructions”), hyponatremia.
Nervous system disorders:
often: paresthesia, headache, dizziness, vertigo;
uncommon: drowsiness*, fainting*;
very rarely: confusion.
Mental disorders:
uncommon: sleep disturbances, mood lability.
Visual disorders:
often: visual disturbances.
Hearing and labyrinth disorders:
often: tinnitus.
Cardiac disorders:
uncommon*: tachycardia, palpitations;
very rarely: heart rhythm disturbances, angina pectoris, myocardial infarction, possibly due to a pronounced decrease in blood pressure in high-risk patients (see section “Special Instructions”).
Vascular disorders:
often: marked decrease in blood pressure and associated symptoms;
uncommon*: vasculitis;
very rare: stroke, possibly due to a marked decrease in blood pressure in high-risk patients (see section “Special Instructions”);
frequency unknown: Raynaud’s syndrome.
Disorders of the respiratory system, chest and mediastinal organs:
often: cough, shortness of breath;
uncommon: bronchospasm;
very rarely: eosinophilic pneumonia, rhinitis.
Digestive system disorders:
often: constipation, nausea, vomiting, abdominal pain, taste disturbance, dyspepsia, diarrhea;
uncommon: dryness of the oral mucosa;
very rare: pancreatitis.
Disorders of the liver and biliary tract:
very rarely: hepatitis (cholestatic or cytolytic) (see section “Special instructions”).
Disorders of the skin and subcutaneous tissues:
often: skin itching, skin rash;
uncommon: angioedema of the face, lips, upper and lower extremities, mucous membranes, tongue, vocal folds and/or larynx, urticaria (see section “Special Instructions”), photosensitivity*, pemphigus*, increased sweating;
rarely: exacerbation of psoriasis*;
very rare: erythema multiforme.
Musculoskeletal and connective tissue disorders:
often: muscle spasm;
uncommon*: arthralgia, myalgia.
Renal and urinary tract disorders:
uncommon: renal failure;
very rare: acute renal failure (ARF).
Disorders of the genital organs and breast:
uncommon: erectile dysfunction.
General disorders and disorders at the injection site:
often: asthenia;
uncommon: chest pain*, peripheral edema*, weakness*, fever*, falls*.
Laboratory and instrumental data:
uncommon*: increased concentrations of urea and creatinine in blood plasma;
rarely: increased activity of liver transaminases and bilirubin concentration in the blood serum.
*Evaluation of the frequency of adverse reactions identified by spontaneous reports was based on data from the results of clinical studies.
Cases of syndrome of inappropriate antidiuretic hormone secretion (SIADH) have been reported with the use of other ACE inhibitors. The syndrome of inappropriate ADH secretion can be considered a very rare but possible complication associated with therapy with ACE inhibitors, including perindopril.
Adverse events noted in clinical studies
In the clinical study, only serious adverse events were recorded. Serious adverse events were observed in patients in the perindopril group and in patients in the placebo group. In the perindopril group, patients experienced a marked decrease in blood pressure, angioedema, and sudden cardiac arrest. The rate of perindopril discontinuation due to cough, severely decreased blood pressure, or other intolerance was higher in the perindopril group compared with the placebo group.
Interaction
Interaction
Concomitant use is contraindicated
The simultaneous use of ACE inhibitors with aliskiren and drugs containing aliskiren is contraindicated in patients with diabetes mellitus and/or with moderate or severe renal impairment (GFR less than 60 ml/min/1.73 m2 body surface area). The simultaneous use of ACE inhibitors with ARA II is contraindicated in patients with diabetic nephropathy. Extracorporeal methods of treatment.
Neutral endopeptidase inhibitors
An increased risk of angioedema has been reported when ACE inhibitors are co-administered with neutral endopeptidase inhibitors such as sacubitril and racecadotril (an enkephalinase inhibitor).
When ACE inhibitors are used simultaneously with drugs containing sacubitril (neprilysin inhibitor), the risk of developing angioedema increases, and therefore the simultaneous use of these drugs is contraindicated. ACE inhibitors should be prescribed no earlier than 36 hours after discontinuation of drugs containing sacubitril. Prescription of drugs containing sacubitril is contraindicated in patients receiving ACE inhibitors, as well as within 36 hours after discontinuation of ACE inhibitors.
Drugs that cause hyperkalemia
Certain drugs or drugs from other pharmacological classes may increase the risk of developing hyperkalemia: aliskiren and aliskiren-containing drugs, potassium salts, potassium-sparing diuretics, ACE inhibitors, ARB II, non-steroidal anti-inflammatory drugs (NSAIDs), heparin, immunosuppressants such as cyclosporine or tacrolimus, trimethoprim, co-trimoxazole (trimethoprim + sulfamethoxazole). Combining these drugs increases the risk of hyperkalemia.
Double blockade of the RAAS
It has been reported in the literature that in patients with established atherosclerotic disease, heart failure, or diabetes mellitus with end-organ damage, concomitant therapy with an ACE inhibitor and an ARB II is associated with a higher incidence of hypotension, syncope, hyperkalemia, or deterioration of renal function (including acute renal failure) compared with the use of only one drug that affects the RAAS. Concomitant use of ACE inhibitors with aliskiren and drugs containing aliskiren is not recommended in patients without diabetes mellitus and/or without moderate or severe renal impairment (and is contraindicated in patients with diabetes mellitus and/or with moderate or severe renal impairment (GFR less than 60 ml/min/1.73 m2 body surface area)). Concomitant use of ACE inhibitors with ARB II is not recommended in patients without diabetic nephropathy (and contraindicated in patients with diabetic nephropathy).
Concomitant use is not recommended
(see also section “Special instructions”)
Aliskiren
In patients without a history of diabetes mellitus and/or moderate renal impairment, there may be an increased risk of hyperkalemia, deterioration of renal function, and increased incidence of cardiovascular morbidity and mortality.
Extracorporeal treatments
Extracorporeal treatments that expose blood to negatively charged surfaces, such as dialysis or hemofiltration with certain high-flux membranes (eg, polyacrylonitrile membranes) and LDL apheresis with dextran sulfate, increase the risk of severe anaphylactoid reactions. If such treatment is required, consideration should be given to using a different type of dialysis membrane or a different class of antihypertensive agent.
Estramustine
Concomitant use may lead to an increased risk of developing angioedema.
Racecadotril (an enkephalinase inhibitor used to treat acute diarrhea)
With simultaneous use of ACE inhibitors with racecadotril, the risk of developing angioedema increases.
Cyclosporine
Concomitant use with ACE inhibitors may increase the risk of developing hyperkalemia. Monitoring of serum potassium levels is recommended.
Heparin
Hyperkalemia may occur when ACE inhibitors are used concomitantly with heparin. Monitoring of serum potassium levels is recommended.
Co-trimoxazole (trimethoprim + sulfamethoxazole)
Trimethoprim is known to act as a potassium-sparing diuretic (such as amiloride). Therefore, simultaneous use with perindopril is not recommended.
mTOR (mammalian Target of Rapamycin) inhibitors, e.g. temsirolimus, sirolimus, everolimus
In patients concomitantly using mTOR inhibitors, the risk of developing angioedema increases.
Potassium-sparing diuretics (such as triamterene, amiloride, spironolactone and its derivative eplerenone), potassium salts
Features of the use of spironolactone in heart failure – see the subsection “Potassium-sparing diuretics (eplerenone, spironolactone)” of this section.
Development of hyperkalemia (possibly fatal), especially with impaired renal function (additional effects associated with hyperkalemia).
The simultaneous use of perindopril with the above-mentioned drugs is not recommended (see section “Special instructions”). If, however, concomitant use is indicated, they should be used with caution and regular monitoring of serum potassium levels.
Lithium preparations
With the simultaneous use of lithium preparations and ACE inhibitors, a reversible increase in the content of lithium in the blood serum and associated toxic effects may be observed. The simultaneous use of perindopril and lithium preparations is not recommended. If such therapy is necessary, lithium levels in the blood plasma should be regularly monitored (see section “Special Instructions”).
Concomitant use requiring extreme caution
Hypoglycemic agents (insulin, hypoglycemic agents for oral administration)
The use of ACE inhibitors may enhance the hypoglycemic effect of insulin and oral hypoglycemic agents, leading to the development of hypoglycemia. As a rule, this is observed in the first weeks of simultaneous therapy and in patients with impaired renal function.
Baclofen
Enhances the antihypertensive effect of ACE inhibitors. Blood pressure levels should be carefully monitored and, if necessary, the dosage of antihypertensive drugs should be adjusted.
Potassium-sparing diuretics
In patients receiving diuretics, especially those that remove fluid and/or salts, a pronounced decrease in blood pressure may be observed at the beginning of perindopril therapy, the risk of which can be reduced by discontinuing the diuretic, replacing fluid or salt loss before starting perindopril therapy, as well as prescribing perindopril at a low dose with its further gradual increase.
In patients with arterial hypertension, the use of diuretics, especially those that remove fluid and/or salt, should either be discontinued before starting the ACE inhibitor (in this case, a potassium-sparing diuretic can be reintroduced later), or the ACE inhibitor should be prescribed at a low dose and then gradually increase it.
In patients with CHF, when using diuretics, an ACE inhibitor should be prescribed in a low dose, possibly after reducing the dose of a potassium-sparing diuretic used simultaneously. In all cases, renal function (serum creatinine concentration) should be monitored in the first weeks of using ACE inhibitors.
Potassium-sparing diuretics (eplerenone, spironolactone)
Use of eplerenone or spironolactone in doses from 12.5 mg to 50 mg per day and low doses of ACE inhibitors
In patients with CHF II-IV functional class according to the NYHA classification with a left ventricular ejection fraction <40%, previously treated with ACE inhibitors and loop diuretics, there is a risk of developing hyperkalemia (with possible death), especially if the recommendations for this combination of drugs are not followed.
Before using this combination of drugs, you must ensure that there is no hyperkalemia and renal dysfunction. It is recommended to regularly monitor the concentration of creatinine and potassium levels in the blood serum: weekly in the first month of treatment and monthly thereafter.
NSAIDs, including high doses of acetylsalicylic acid (more than 3 g/day)
Concomitant use of ACE inhibitors with NSAIDs (acetylsalicylic acid at a dose that has an anti-inflammatory effect, cyclooxygenase-2 [COX-2] inhibitors and non-selective NSAIDs) may lead to a decrease in the antihypertensive effect of ACE inhibitors. Concomitant use of ACE inhibitors and NSAIDs may lead to deterioration of renal function, including the development of acute renal failure, and an increase in serum potassium, especially in patients with reduced renal function. Caution should be exercised when using this combination, especially in elderly patients. Patients should receive adequate fluids. It is recommended to carefully monitor renal function both at the beginning and during treatment.
Tissue plasminogen activators
Observational studies have shown an increased incidence of angioedema in patients taking ACE inhibitors following the use of alteplase for thrombolytic therapy of ischemic stroke.
Concomitant use requiring caution
Antihypertensive drugs and vasodilators
The antihypertensive effect of perindopril may be enhanced when used simultaneously with other antihypertensive and vasodilating agents, including short- and long-acting nitrates.
Dipeptidyl peptidase type 4 (DPP-4) inhibitors – gliptins (eg, linagliptin, saxagliptin, sitagliptin, vildagliptin)
Concomitant use with ACE inhibitors may increase the risk of developing angioedema.
Tricyclic antidepressants, antipsychotics (neuroleptics) and general anesthetics
Concomitant use with ACE inhibitors may lead to increased antihypertensive effects (see section “Special Instructions”).
Sympathomimetics
Sympathomimetics may reduce the antihypertensive effect of ACE inhibitors.
Gold preparations
With the simultaneous use of ACE inhibitors, including perindopril, with a gold drug (sodium aurothiomalate intravenously), a symptom complex was described, including facial flushing, nausea, vomiting, and arterial hypotension.
Overdose
Overdose
Data on drug overdose are limited.
Symptoms
Marked decrease in blood pressure, shock, water and electrolyte imbalance, renal failure, hyperventilation, tachycardia, palpitations, bradycardia, dizziness, anxiety, cough.
Treatment
Emergency measures are limited to removing the drug from the body: gastric lavage and/or taking activated charcoal, followed by restoration of water and electrolyte balance.
If there is a pronounced decrease in blood pressure, the patient should be transferred to the “lying” position on his back with his legs elevated. If necessary, 0.9% sodium chloride solution should be administered intravenously (IV). If necessary, a solution of catecholamines can be administered intravenously. Perindoprilat, the active metabolite of perindopril, can be removed from the body by dialysis. If treatment-resistant bradycardia develops, implantation of a pacemaker may be required. It is necessary to constantly monitor indicators of basic vital functions of the body, creatinine concentration and electrolyte content in the blood serum.
Clinical pharmacology
Clinical pharmacology
Pharmacodynamics
Mechanism of action
Perindopril is an inhibitor of the enzyme that converts angiotensin I to angiotensin II. ACE (kininase II) is an exopeptidase that converts angiotensin I into the vasoconstrictor angiotensin II and breaks down bradykinin, which has a vasodilator effect, into an inactive heptapeptide. As a result, perindopril reduces the secretion of aldosterone.
Since ACE inactivates bradykinin, suppression of ACE is accompanied by an increase in the activity of both the circulating and tissue kallikrein-kinin system, while the prostaglandin system is also activated. It is possible that this effect is part of the mechanism of the antihypertensive effect of ACE inhibitors, as well as the mechanism of development of some side effects of drugs of this class (for example, cough). Perindopril has a therapeutic effect due to the active metabolite perindoprilat. Other metabolites do not have an inhibitory effect on ACE in vitro.
Clinical efficacy and safety
Arterial hypertension
Perindopril is effective in the treatment of arterial hypertension of any severity. With the use of perindopril, there is a decrease in both systolic and diastolic blood pressure (BP) in the patient’s “lying” and “standing” position.
Perindopril reduces total peripheral vascular resistance (TPVR), which leads to a decrease in blood pressure, while peripheral blood flow accelerates without changing heart rate (HR).
As a rule, perindopril leads to an increase in renal blood flow, while the glomerular filtration rate (GFR) does not change.
The antihypertensive effect of the drug reaches its maximum 4-6 hours after a single oral dose and persists for 24 hours. 24 hours after oral administration, pronounced (about 87-100%) residual ACE inhibition is observed. A decrease in blood pressure is achieved quite quickly. In patients with a positive response to treatment, normalization of blood pressure occurs within a month and is maintained without the development of tachycardia.
Cessation of treatment is not accompanied by the development of withdrawal syndrome.
Perindopril has a vasodilating effect, helps restore the elasticity of large arteries and the structure of the vascular wall of small arteries, and also reduces left ventricular hypertrophy.
The simultaneous use of thiazide diuretics increases the severity of the antihypertensive effect. In addition, the combination of an ACE inhibitor and a thiazide diuretic also reduces the risk of hypokalemia while taking diuretics.
Chronic heart failure (CHF)
Perindopril normalizes heart function by reducing preload and afterload.
In patients with CHF who received perindopril, a decrease in filling pressure in the left and right ventricles of the heart, a decrease in peripheral vascular resistance, an increase in cardiac output and an increase in the cardiac index were detected. Perindopril at a dose of 2 mg does not significantly reduce blood pressure in patients with CHF (functional class II-III according to the NYHA classification).
Cerebrovascular diseases
When taking perindopril at a dose of 4 mg, as well as in combination with indapamide, there is a reduction in the risk of developing a recurrent stroke (both ischemic and hemorrhagic), as well as an additional reduction in the risk:
· fatal or disabling strokes;
· major cardiovascular complications, including myocardial infarction, including death;
· stroke-related dementia;
· serious deterioration in cognitive function.
Stable coronary heart disease (CHD)
When using perindopril at a dose of 8 mg/day in patients with stable coronary artery disease, there is a significant reduction in the absolute risk of complications provided for by the main criterion of effectiveness (mortality from cardiovascular diseases, the incidence of non-fatal myocardial infarction and/or cardiac arrest followed by successful resuscitation).
Pharmacokinetics
Suction
When taken orally, perindopril is rapidly absorbed from the gastrointestinal tract, the maximum concentration (Cmax) in the blood plasma is reached after 1 hour. The half-life (T½) of perindopril from blood plasma is 1 hour.
Perindopril has no pharmacological activity. Approximately 27% of the total amount of absorbed perindopril enters the bloodstream in the form of the active metabolite perindoprilate. In addition to perindoprilate, 5 more metabolites are formed that do not have pharmacological activity. Cmax of perindoprilate in blood plasma is achieved 3-4 hours after oral administration.
Food intake slows down the conversion of perindopril to perindoprilat, thereby affecting bioavailability. Therefore, Perineva® should be taken orally once a day, in the morning, before meals.
A linear relationship has been demonstrated between the dose of perindopril and its exposure in blood plasma.
Distribution
The volume of distribution of free perindoprilate is approximately 0.2 l/kg. The association of perindoprilate with plasma proteins, mainly with ACE, is less than 30% and is dose-dependent.
Withdrawal
Perindoprilat is excreted by the kidneys. T½ of the free fraction is 3-5 hours. The “effective” T½ is approximately 17 hours, the equilibrium state in the blood plasma is achieved within 4 days.
Pharmacokinetics in certain groups of patients
The elimination of perindoprilate is slowed down in elderly patients, as well as in patients with heart and renal failure.
Dialysis clearance of perindoprilate is 70 ml/min.
In patients with liver cirrhosis, the hepatic clearance of perindopril is reduced by 2 times. However, the amount of perindoprilate formed does not decrease, and no dose adjustment of Perineva® is required (see sections “Dosage and Administration”, “Special Instructions”).
Storage conditions
Storage conditions
At a temperature not exceeding 25 ºС, in the original packaging.
Keep out of the reach of children.
Shelf life
Shelf life
3 years.
Do not use the drug after the expiration date.
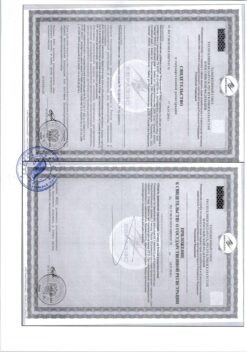
Manufacturer
Manufacturer
KRKA-RUS, Russia
Additional information
| Shelf life | 3 years. Do not use the drug after the expiration date. |
|---|---|
| Conditions of storage | At the temperature not more than 25 ºС, in the original package. Keep out of reach of children. |
| Manufacturer | KRKA-RUS, Russia |
| Medication form | pills |
| Brand | KRKA-RUS |
Other forms…
Related products
Buy Perineva, tablets 4 mg 90 pcs with delivery to USA, UK, Europe and over 120 other countries.