No products in the cart.
Paxil, 20 mg 100 pcs
€33.84 €28.20
Out of stock
(E-mail when Stock is available)
Description
Paxil – antidepressant activity is due to specific inhibition of serotonin reuptake in brain neurons.
Pharmacodynamics
Paxil has low affinity for muscarinic cholinergic receptors, and animal studies have shown that the anticholinergic properties are weakly expressed. In-vitro studies have shown that paroxetine has weak affinity for alpha1-, alpha2– and beta-adrenoceptors, as well as to dopamine (D2), serotonin 5-NT1– and 5-NT2– and histamine (H1) receptors.
The absence of interaction with postsynaptic receptors in vivo is confirmed by the results of in vivo studies, which demonstrated that paroxetine has no ability to depress the CNS and cause arterial hypotension. It does not impair psychomotor functions and does not increase the CNS depressant effect of ethanol.
Like other selective serotonin reuptake inhibitors (SSRIs), paroxetine causes symptoms of overstimulation of 5-NT receptors when administered to animals that previously received MAO inhibitors or tryptophan.
Studies of behavior and EEG changes have demonstrated that paroxetine causes weak activating effects at doses greater than those required to inhibit serotonin reuptake. Its activating properties are not amphetamine-like in nature.
Animal studies have shown that paroxetine has no effect on the cardiovascular system.
In healthy individuals, paroxetine does not cause clinically significant changes in BP, HR and ECG.
Pharmacokinetics
In oral administration, it is well absorbed and metabolized by “first pass” through the liver. Due to “first pass” metabolism, a smaller amount of paroxetine enters the systemic bloodstream than is absorbed from the gastrointestinal tract. As the amount of paroxetine in the body increases with a single high-dose administration or with multiple conventional doses, there is partial saturation of the first-pass metabolic pathway and a decrease in the clearance of paroxetine from plasma. This results in a disproportionate increase in plasma paroxetine concentrations.
Hence, its pharmacokinetic parameters are unstable, resulting in nonlinear kinetics. It should be noted, however, that the nonlinearity is usually weak and is observed only in patients in whom low plasma levels of paroxetine are achieved at low doses of the drug. Equilibrium plasma concentrations are reached after 7-14 days.
Paroxetine is widely distributed in tissues, and pharmacokinetic calculations show that only 1% of all paroxetine present in the body remains in plasma. At therapeutic concentrations, approximately 95% of plasma paroxetine is bound to proteins. No correlation has been found between the plasma concentrations of paroxetine and its clinical effects (adverse reactions and efficacy). Paroxetine has been found to penetrate in small amounts into the breast milk of women, as well as into the embryos and fetuses of laboratory animals.
Biotransformed into inactive polar and conjugated products (oxidation and methylation processes). T1/2 varies, but is usually about one day (16-24 h). About 64% is excreted in the urine as metabolites, less than 2% unchanged; the remainder is excreted in the feces (probably entering it with bile) as metabolites, less than 1% unchanged. Excretion of metabolites is biphasic, including primary metabolism (first phase) and systemic elimination.
Indications
Indications
Depression of all types in adults, including reactive and severe depression, as well as depression accompanied by anxiety;
OCD in adults (including as a means of maintenance and preventive therapy), as well as in children and adolescents 7–17 years old;
panic disorder in adults, with and without agoraphobia (including as a means of maintenance and preventive therapy;
social phobia in adults (including as a means of maintenance and preventive therapy), as well as in children and adolescents aged 8–17 years;
generalized anxiety disorder in adults (including as a means of maintenance and preventive therapy);
post-traumatic stress disorder in adults.
Pharmacological effect
Pharmacological effect
Paxil – antidepressant activity is due to the specific inhibition of serotonin reuptake in brain neurons.
Pharmacodynamics
It has low affinity for muscarinic cholinergic receptors, and animal studies have shown that the anticholinergic properties are weak. In vitro studies have shown that paroxetine has weak affinity for alpha1, alpha2 and beta adrenergic receptors, as well as dopamine (D2), serotonin 5-HT1 and 5-HT2 and histamine (H1) receptors.
The lack of interaction with postsynaptic receptors in vitro is confirmed by the results of in vivo studies, which demonstrated that paroxetine lacks the ability to depress the central nervous system and cause arterial hypotension. Does not disrupt psychomotor functions and does not enhance the inhibitory effect of ethanol on the central nervous system.
Like other selective serotonin reuptake inhibitors (SSRIs), paroxetine causes symptoms of excessive stimulation of 5-HT receptors when administered to animals that have previously received MAO inhibitors or tryptophan.
Behavioral and EEG studies have demonstrated that paroxetine produces weak activating effects at doses greater than those required to inhibit serotonin reuptake. Its activating properties are not amphetamine-like in nature.
Animal studies have shown that paroxetine does not affect the cardiovascular system.
In healthy individuals, paroxetine does not cause clinically significant changes in blood pressure, heart rate and ECG.
Pharmacokinetics
When taken orally, it is well absorbed and undergoes “first pass” metabolism through the liver. Due to first-pass metabolism, less paroxetine enters the systemic circulation than is absorbed from the gastrointestinal tract. As the amount of paroxetine in the body increases, with a single dose of large doses or with multiple doses of usual doses, partial saturation of the first-pass metabolic pathway occurs and the clearance of paroxetine from plasma decreases. This results in a disproportionate increase in paroxetine plasma concentrations.
Therefore, its pharmacokinetic parameters are unstable, resulting in nonlinear kinetics. It should be noted, however, that nonlinearity is usually mild and is observed only in those patients who achieve low plasma levels of paroxetine while taking low doses of the drug. Equilibrium plasma concentration is achieved after 7–14 days.
Paroxetine is widely distributed in tissues, and pharmacokinetic calculations show that only 1% of the total amount of paroxetine present in the body remains in the plasma. At therapeutic concentrations, approximately 95% of paroxetine in plasma is protein bound. No correlation was found between paroxetine plasma concentrations and its clinical effect (adverse reactions and efficacy). It has been established that paroxetine passes into the breast milk of women in small quantities, as well as into the embryos and fetuses of laboratory animals.
Biotransforms into inactive polar and conjugated products (oxidation and methylation processes). T1/2 varies, but is usually about one day (16–24 hours). About 64% is excreted in the urine in the form of metabolites, less than 2% – unchanged; the remaining amount is excreted in the feces (probably entering it with bile) in the form of metabolites, less than 1% – unchanged. The elimination of metabolites is biphasic, including primary metabolism (first phase) and systemic elimination.
Special instructions
Special instructions
Cancel paroxetine. Withdrawal symptoms have been reported to include dizziness, sensory disturbances (including paresthesia and electric shock sensations), sleep disturbances (including vivid dreams), agitation and anxiety, nausea, tremors, confusion, sweating, headaches and diarrhea. These symptoms are usually mild or moderate, but in some patients they can be severe.
They usually occur in the first few days after stopping the drug, but in rare cases they occur in patients who accidentally missed just one dose. As a rule, these symptoms resolve spontaneously and disappear within 2 weeks, but in some patients they can last much longer (2-3 months or more).
As with other psychotropic drugs, abrupt withdrawal of paroxetine should be avoided. The following withdrawal regimen may be recommended: reducing the daily dose by 10 mg at weekly intervals; after reaching a dose of 20 mg/day (or 10 mg/day in children and adolescents), patients continue to take this dose for 1 week and only after that the drug is completely discontinued.
If withdrawal symptoms develop during dose reduction or after discontinuation of the drug, it is advisable to resume the previously prescribed dose. Subsequently, the doctor may continue to reduce the dose, but more slowly.
The occurrence of withdrawal symptoms does not mean that the drug is abused or addictive, as is the case with narcotics and psychotropic substances.
Symptoms that may occur when treatment with paroxetine is stopped in children and adolescents. Symptoms of paroxetine withdrawal (emotional lability, including suicidal thoughts, suicide attempts, mood changes and tearfulness, as well as nervousness, dizziness, nausea and abdominal pain) were recorded in 2% of patients during a dose reduction of paroxetine or after its complete discontinuation and occurred 2 times more often than in the placebo group.
Selected groups of patients.
Elderly patients. In elderly patients, paroxetine plasma concentrations may be increased, but the range of concentrations is similar to that in younger patients. In this category of patients, therapy should begin with the dose recommended for adults, which can be increased to 40 mg/day.
Patients with impaired renal or liver function. Paroxetine plasma concentrations are increased in patients with severe renal impairment (Cl creatinine less than 30 ml/min) and in patients with impaired liver function. Such patients should be prescribed doses of the drug that are at the lower end of the therapeutic dose range.
Children under 7 years old. The use of paroxetine is not recommended due to the lack of studies of the safety and effectiveness of the drug in this group of patients.
Children and adolescents 7–17 years old. In clinical trials, adverse events related to suicidality (suicide attempts and suicidal ideation) and hostility (primarily aggression, deviant behavior and anger) were observed more often in children and adolescents receiving paroxetine than in those patients in this age group who received placebo. There are currently no data on the long-term safety of paroxetine in children and adolescents regarding the effects of this drug on growth, maturation, cognitive and behavioral development.
Clinical impairment and suicide risk associated with mental disorders. In patients with depression, worsening symptoms of the disorder and/or the emergence of suicidal thoughts and behavior (suicidality) may occur regardless of whether they are receiving antidepressants. This risk persists until significant remission is achieved. There may be no improvement in the patient’s condition in the first weeks of treatment or more, so the patient must be closely monitored for timely detection of clinical exacerbation and suicidality, especially at the beginning of the course of treatment, as well as during periods of dose changes, whether increasing or decreasing them. Clinical experience with all antidepressants suggests that the risk of suicide may increase in the early stages of recovery.
Other mental disorders for which paroxetine is used may also be associated with an increased risk of suicidal behavior. In addition, these disorders may represent comorbid conditions associated with major depressive disorder. Therefore, when treating patients suffering from other mental disorders, the same precautions should be taken as when treating major depressive disorder.
Those at greatest risk for suicidal thoughts or suicide attempts are patients with a history of suicidal behavior or suicidal thoughts, young patients, and patients with severe suicidal thoughts before treatment, so all of them need to be given special attention during treatment.
Patients (and those caring for them) should be warned to monitor for worsening of their condition and/or the emergence of suicidal ideation/behavior or thoughts of self-harm and to seek immediate medical attention if these symptoms occur.
Akathisia. Occasionally, treatment with paroxetine or another SSRI drug is accompanied by the occurrence of akathisia, which is manifested by a feeling of internal restlessness and psychomotor agitation, when the patient cannot sit or stand quietly; With akathisia, the patient usually experiences subjective distress. The likelihood of akathisia occurring is highest in the first few weeks of treatment.
Serotonin syndrome/neuroleptic malignant syndrome. In rare cases, serotonin syndrome or neuroleptic malignant syndrome-like symptoms may occur during treatment with paroxetine, especially if paroxetine is used in combination with other serotonergic drugs and/or antipsychotics. These syndromes are potentially life-threatening and, if they occur, treatment with paroxetine should be discontinued (they are characterized by a combination of symptoms such as hyperthermia, muscle rigidity, myoclonus, autonomic disturbances with possible rapid changes in vital signs, changes in mental status, including confusion, irritability, extremely severe agitation, progressing to delirium and coma) and supportive symptomatic therapy should be initiated. Paroxetine should not be prescribed in combination with serotonin precursors such as L-tryptophan, oxytriptan due to the risk of developing serotonergic syndrome.
Mania and bipolar disorder. A major depressive episode may be the initial manifestation of bipolar disorder. It is generally accepted (although not proven in controlled clinical trials) that treating such an episode with an antidepressant alone may increase the likelihood of an accelerated development of a mixed/manic episode in patients at risk for bipolar disorder.
Before initiating antidepressant treatment, careful screening should be performed to assess the patient’s risk of bipolar disorder; Such screening should include a detailed psychiatric history, including a family history of suicide, bipolar disorder, and depression. Like all antidepressants, paroxetine is not registered for the treatment of bipolar depression. Paroxetine should be used with caution in patients with a history of mania.
MAO inhibitors. Treatment with paroxetine should be started cautiously, no earlier than 2 weeks after stopping therapy with MAO inhibitors; The dose of paroxetine should be increased gradually until the optimal therapeutic effect is achieved (see also “Contraindications”).
Impaired kidney or liver function. Caution is advised when treating patients with severe renal impairment and patients with impaired liver function with paroxetine.
Epilepsy. As with other antidepressants, paroxetine should be used with caution in patients with epilepsy.
Convulsive seizures. The incidence of seizures in patients taking paroxetine is less than 0.1%. If a seizure occurs, treatment with paroxetine should be discontinued.
Electroconvulsive therapy. There is limited experience with the concomitant use of paroxetine and electroconvulsive therapy.
Glaucoma. Like other SSRI drugs, paroxetine has occasionally been associated with mydriasis and should be used with caution in patients with angle-closure glaucoma.
Hyponatremia. Hyponatremia occurs rarely during treatment with paroxetine and occurs predominantly in elderly patients.
Bleeding. Bleeding into the skin and mucous membranes (including gastrointestinal bleeding) has been reported in patients treated with paroxetine. Therefore, paroxetine should be used with caution in patients who are concomitantly receiving drugs that increase the risk of bleeding, in patients with a known bleeding tendency, and in patients with diseases predisposing to bleeding.
Heart diseases. Normal precautions should be taken when treating patients with heart disease.
Clinical experience with paroxetine suggests that it does not impair cognitive and psychomotor function. However, as with treatment with any other psychotropic drugs, patients should be especially careful when driving a car and operating machinery.
Although paroxetine does not enhance the negative effects of alcohol on psychomotor functions, it is not recommended to use paroxetine and alcohol simultaneously.
Active ingredient
Active ingredient
Paroxetine
Composition
Composition
Active ingredient:
paroxetine hydrochloride hemihydrate 22.8 mg (equivalent to 20.0 mg paroxetine);
Excipients:
calcium dihydrogen phosphate dihydrate;
sodium carboxymethyl starch type A;
magnesium stearate;
Tablet shell:
Opadry white YS-1R-7003 (hypromellose, titanium dioxide, macrogol 400, polysorbate 80);
Pregnancy
Pregnancy
Pregnancy
Animal studies have not shown paroxetine to be teratogenic or selectively embryotoxic, and data from a small number of women who took paroxetine during pregnancy suggest no increased risk of congenital anomalies in the newborn. There are reports of preterm birth in women who received paroxetine or other SSRI drugs during pregnancy, but a cause-and-effect relationship between these drugs and preterm birth has not been established. Paroxetine should not be used during pregnancy unless the potential benefit outweighs the potential risk.
It is necessary to closely monitor the health of those newborns whose mothers took paroxetine in late pregnancy, since there are reports of complications in newborns exposed to paroxetine or other SSRI drugs in the third trimester of pregnancy.
It should be noted, however, that in this case, a cause-and-effect relationship between the mentioned complications and this drug therapy has not been established. Clinical complications reported included: respiratory distress, cyanosis, apnea, seizures, temperature instability, feeding difficulties, vomiting, hypoglycemia, hypertension, hypotension, hyperreflexia, tremor, shaking, irritability, lethargy, persistent crying, and somnolence. In some reports, symptoms have been described as neonatal manifestations of withdrawal syndrome. In most cases, the described complications occurred immediately after childbirth or shortly thereafter
Lactation
A small amount of paroxetine passes into breast milk. However, paroxetine should not be taken during breastfeeding unless the benefit to the mother outweighs the potential risk to the baby.
Contraindications
Contraindications
Hypersensitivity to paroxetine and the components of the drug.
Combined use of paroxetine with MAO inhibitors (paroxetine should not be used simultaneously with MAO inhibitors or within 2 weeks after their discontinuation; MAO inhibitors should not be prescribed within 2 weeks after stopping treatment with paroxetine).
Concomitant use with thioridazine (paroxetine should not be administered in combination with thioridazine because, like other drugs that inhibit the activity of the CYP2D6 cytochrome P450 enzyme, paroxetine may increase plasma concentrations of thioridazine).
Side Effects
Side Effects
Disorders of the blood and lymphatic system: sometimes – abnormal bleeding, mainly hemorrhage into the skin and mucous membranes (most often bruises); very rarely – thrombocytopenia.
Immune system disorders: very rarely – allergic reactions (including urticaria and angioedema).
Endocrine disorders: very rarely – syndrome of impaired ADH secretion.
Metabolic disorders: often – loss of appetite; rarely – hyponatremia (occurs mainly in elderly patients and may be caused by the syndrome of impaired ADH secretion).
Mental disorders: often – drowsiness, insomnia; sometimes – confusion, hallucinations; rarely – manic reactions. These symptoms may also be due to the disease itself.
Visual disturbances: often – blurred vision; very rarely – exacerbation of glaucoma.
Cardiac disorders: sometimes – sinus tachycardia.
Vascular disorders: sometimes – transient increase or decrease in blood pressure, incl. in patients with pre-existing hypertension or anxiety.
Respiratory, thoracic and mediastinal disorders: often – yawning.
Nervous system disorders: often – seizures.
Gastrointestinal disorders: very often – nausea; often – constipation, diarrhea, dry mouth; very rarely – gastrointestinal bleeding.
Hepatobiliary disorders: rarely – increased levels of liver enzymes; very rarely – hepatitis, sometimes accompanied by jaundice and/or liver failure.
Sometimes there is an increase in liver enzyme levels. Post-marketing reports of liver damage such as hepatitis, sometimes with jaundice, and/or liver failure are very rare. The question of the advisability of stopping treatment with paroxetine must be decided in cases where there is a prolonged increase in liver function tests.
Disorders of the skin and subcutaneous tissues: often – sweating; rarely – skin rashes; very rarely – photosensitivity reactions.
Renal and urinary tract disorders: rarely – urinary retention.
Disorders of the reproductive system and mammary glands: very often – sexual dysfunction; rarely – hyperprolactinemia/galactorrhea.
General disorders: often – asthenia; very rarely – peripheral edema.
Symptoms that occur when stopping treatment with paroxetine: often – dizziness, sensory disturbances, sleep disturbances, anxiety, headache; sometimes – agitation, nausea, tremor, confusion, sweating, diarrhea.
Interaction
Interaction
Serotonergic drugs. The use of paroxetine, like other drugs of the SSRI group, simultaneously with serotonergic drugs (including MAO inhibitors, L-tryptophan, triptans, tramadol, linezolid, other drugs of the SSRI group, lithium and herbal remedies containing St. John’s wort) may be accompanied by the development of effects due to serotonin. When using these drugs in combination with paroxetine, caution and close clinical monitoring should be performed.
Enzymes involved in drug metabolism. The metabolism and pharmacokinetics of paroxetine may be altered by induction or inhibition of enzymes that are involved in drug metabolism. When using paroxetine concomitantly with inhibitors of enzymes involved in drug metabolism, the advisability of using a dose of paroxetine that is in the lower part of the therapeutic dose range should be assessed.
The initial dose of paroxetine does not need to be adjusted if it is used concomitantly with a drug that is a known inducer of enzymes involved in drug metabolism (for example, carbamazepine, rifampicin, phenobarbital, phenytoin). Any subsequent dose adjustment of paroxetine should be determined by its clinical effects (tolerability and efficacy).
CYP3A4. An in vivo interaction study with simultaneous use of paroxetine and terfenadine, which is a substrate of the CYP3A4 enzyme, under steady-state conditions, showed that paroxetine does not affect the pharmacokinetics of terfenadine. In a similar in vivo interaction study, no effect of paroxetine on the pharmacokinetics of alprozalam was found and vice versa. Concomitant use of paroxetine with terfenadine, alprozalam and other drugs that serve as substrates for the CYP3A4 enzyme is unlikely to cause harm to the patient.
The ability of paroxetine to inhibit the CYP2D6 enzyme (see also “Contraindications”). Like other antidepressants, including other SSRI drugs, paroxetine inhibits the liver enzyme CYP2D6, which belongs to the cytochrome P450 system. Inhibition of the CYP2D6 enzyme may lead to increased plasma concentrations of concomitantly used drugs that are metabolized by this enzyme. These drugs include tricyclic antidepressants (eg, amitriptyline, nortriptyline, imipramine, and desipramine), phenothiazine antipsychotics, risperidone, some type 1C antiarrhythmics (eg, propafenone and flecainide), and metoprolol.
Procyclidine. Daily administration of paroxetine significantly increases plasma concentrations of procyclidine. If anticholinergic effects occur, the dose of procyclidine should be reduced.
Anticonvulsants: carbamazepine, phenytoin, sodium valproate. The simultaneous use of paroxetine and these drugs does not affect their pharmacokinetics and pharmacodynamics in patients with epilepsy.
Clinical studies have shown that the absorption and pharmacokinetics of paroxetine are independent or practically independent (that is, the existing dependence does not require dose changes) from food intake, antacids, digoxin, propranolol, and alcohol.
Overdose
Overdose
Symptoms: in addition to the symptoms described in the “Side Effects” section, vomiting, dilated pupils, fever, changes in blood pressure, involuntary muscle contractions, agitation, anxiety, and tachycardia are observed.
The patients’ condition usually returned to normal without serious consequences, even with single doses of up to 2000 mg. A number of reports have described symptoms such as coma and ECG changes; Deaths have been very rare, usually in situations where patients were taking paroxetine with other psychotropic drugs or with alcohol.
Treatment: general measures used in case of overdose of any antidepressants; if necessary, gastric lavage, administration of activated charcoal (20–30 mg every 4–6 hours during the first day after an overdose), maintenance therapy and frequent monitoring of basic physiological parameters.
There is no specific antidote for paroxetine.
Storage conditions
Storage conditions
In a dry place, at a temperature not exceeding 30 °C
Shelf life
Shelf life
3 years
Manufacturer
Manufacturer
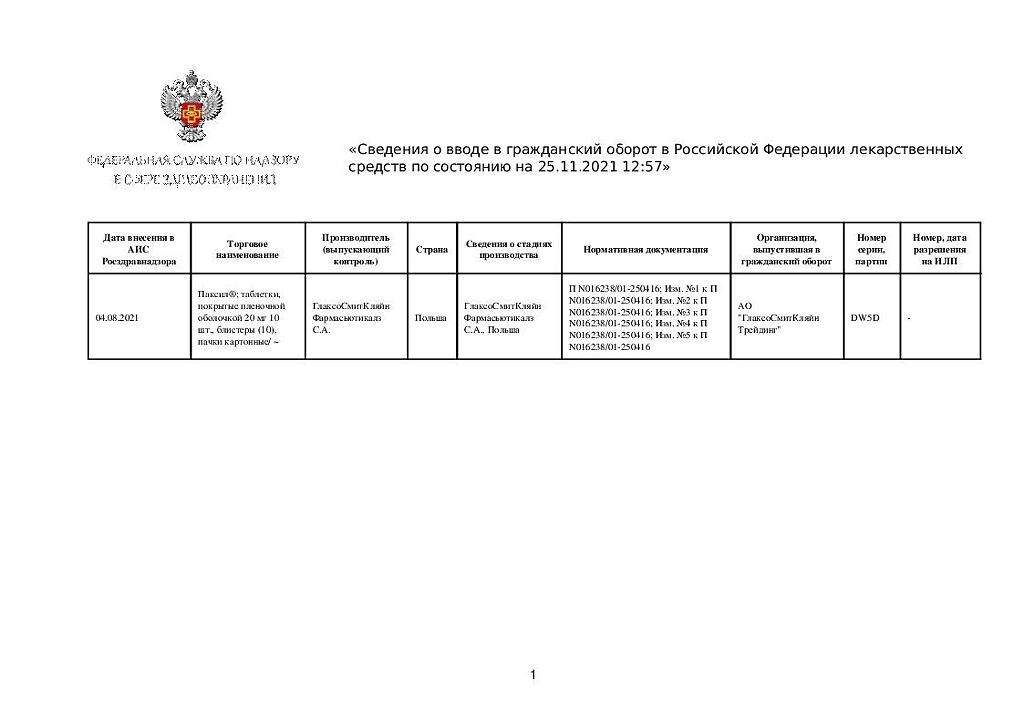
GlaxoSmithKline Pharmaceuticals S.A., Poland
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | In a dry place, at a temperature not exceeding 30 °C |
| Manufacturer | GlaxoSmithKline Pharmaceuticals S.A., Poland |
| Medication form | pills |
| Brand | GlaxoSmithKline Pharmaceuticals S.A. |
Other forms…
Related products
Buy Paxil, 20 mg 100 pcs with delivery to USA, UK, Europe and over 120 other countries.