Subtotal: €29.34
Otesla, 10 mg+20 mg+30 mg+30 mg 14 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Mechanism of action
Apremilast, is a small molecule – FDE-4 inhibitor, which acts inside the cell, modulating pro-inflammatory and anti-inflammatory mediators. FDE-4 is a specific FDE-cAMP, the dominant FDE in inflammatory cells. Inhibition of FDE-4 increases the amount of cAMP, which in turn leads to suppression of the inflammatory response by modulating the expression of TNF-α, IL-23, IL-17 and other inflammatory cytokines. cAMP also modulates the levels of some anti-inflammatory cytokines, such as IL-10. These pro- and anti-inflammatory mediators are involved in the pathogenesis of psoriasis and psoriatic arthritis (PsA).
Pharmacodynamic Effects
In clinical studies in PsA patients, apremilast significantly modulated but did not completely inhibit plasma proteins: IL-1α, IL-6, IL-8, monocyte chemoattract protein-1 (MXE-1), macrophage inflammatory protein-1β (MBB-1β), matrix metalloproteinase-3 (MMP-3) and TNF-α. After 40 weeks of treatment with apremilast, a decrease in IL-17 and IL-23 concentrations and an increase in plasma IL-10 concentrations were observed. In psoriasis patients, apremilast reduced focal epidermal thickening of affected skin areas, inflammatory cell infiltration and expression of proinflammatory genes including inducible nitric oxide synthase (iNOS), IL-12/IL-23p40, IL-17A, IL-22 and IL-8 genes.
Apremilast when administered in doses up to 50 mg twice daily does not prolong the QT interval in healthy subjects.
1493 patients with active PsA (≥3 swollen joints and ≥3 painful joints), despite prior therapy with low-molecular-weight or biological disease-modifying drugs (DMARDs) for at least 6 months, received oral placebo, apremilast 20 mg or apremilast 30 mg 2 times daily. Apremilast was used as monotherapy (34.8%) or in combination with stable doses of LMWH (65.2%). 76.4% of patients had previously received only low-molecular-weight BMLS, and 22.4% of patients had been previously treated with biological BMLS, among whom 7.8% found this therapy ineffective. The average duration of PsA was 5 years.
Apremilast therapy resulted in a significant improvement in PsA symptoms compared with placebo.
The effectiveness of apremilast treatment did not differ among patients receiving or not receiving concomitant BMLS, including methotrexate. The therapeutic effects of apremilast were more pronounced in patients who received BMLS or biological BMLS prior to apremilast therapy than in those who received placebo. There was a significant, statistically significant improvement in functional activity on apremilast therapy.
A total of 1257 patients with moderate to severe plaque psoriasis who were scheduled for phototherapy or systemic therapy were randomized to the placebo or apremilast group (oral, 30 mg twice daily). Approximately 30% of patients had not previously received phototherapy, standard systemic or biological drugs.
On the background of apremilast therapy, patients with moderate to severe psoriasis showed significant improvement compared with placebo. The efficacy of apremilast was manifested with respect to the complex of clinical manifestations of psoriasis, including itching, nail and scalp lesions, as well as quality of life.
The clinical effectiveness of apremilast was confirmed in various patient subgroups formed by initial demographic and clinical characteristics (including the duration of psoriasis and a history of PsA). The positive clinical effect of the drug was independent of the previous drug therapy of psoriasis and its results. Response to apremilast treatment was rapid and was expressed in a significant reduction of psoriasis symptoms already by the 2nd week of treatment, compared to placebo.
Indications
Psoriatic arthritis
Treatment of active psoriatic arthritis (PsA) in adults in monotherapy or in combination with disease-modifying anti-inflammatory drugs (DMARDs) in case of insufficient response or intolerance to previous DMARD therapy.
Psoriasis
Treatment of moderate to severe plaque psoriasis in adults with insufficient response to, contraindications to, or intolerance to basic anti-inflammatory therapy, including cyclosporine, methotrexate, or drugs used in conjunction with ultraviolet-A irradiation (PUVA).
Pharmacological effect
Mechanism of action
Apremilast is a small molecule PDE4 inhibitor that acts intracellularly to modulate pro-inflammatory and anti-inflammatory mediators. PDE-4 is a cAMP-specific PDE, the dominant PDE in inflammatory cells. When PDE-4 is inhibited, the amount of cAMP increases, which, in turn, leads to the suppression of the inflammatory response by modulating the expression of TNF-α, IL-23, IL-17 and other inflammatory cytokines. cAMP also modulates the levels of some anti-inflammatory cytokines, such as IL-10. These pro- and anti-inflammatory mediators are involved in the pathogenesis of psoriasis and psoriatic arthritis (PsA).
Pharmacodynamic effects
In clinical studies in patients with PsA, apremilast significantly modulated, but did not completely inhibit, the plasma proteins IL-1α, IL-6, IL-8, monocyte chemoattractor protein-1 (MXE-1), macrophage inflammatory protein-1β (MBB-1β), matrix metalloproteinase-3 (MMP-3), and TNF-α. After 40 weeks of treatment with apremilast, a decrease in the concentration of IL-17 and IL-23 and an increase in the concentration of IL-10 in the blood plasma were noted. In patients with psoriasis, apremilast reduced focal epidermal thickening of affected skin areas, inflammatory cell infiltration, and the expression of proinflammatory genes, including inducible nitric oxide synthase (iNOS), IL-12/IL-23p40, IL-17A, IL-22, and IL-8 genes.
Apremilast, when administered in doses up to 50 mg twice daily, does not prolong the QT interval in healthy subjects.
1493 patients with active PsA (≥3 swollen joints and ≥3 tender joints), despite prior treatment with small molecule or biologic disease-modifying drugs (BDMD) for at least 6 months, received oral placebo, apremilast 20 mg, or apremilast 30 mg twice daily. Apremilast was used as monotherapy (34.8%) or in combination with stable doses of low-molecular-weight drugs (65.2%). 76.4% of patients had previously received only low-molecular-weight BMDLs, and 22.4% of patients had previously been treated with biological BMDLs, among whom this therapy was ineffective in 7.8%. The average duration of PsA is 5 years.
Apremilast therapy resulted in a significant improvement in PsA symptoms compared with placebo.
The effectiveness of apremilast treatment did not differ in patients who were or were not simultaneously receiving BMDS, including methotrexate. In patients who took BMDMs or biologic BMDMs prior to apremilast therapy, the therapeutic effects of apremilast were greater than those who took placebo. During apremilast therapy, a significant, statistically significant improvement in functional activity was noted.
A total of 1257 patients with moderate to severe plaque psoriasis scheduled for phototherapy or systemic therapy were randomized to placebo or apremilast (oral, 30 mg twice daily). Approximately 30% of patients had not previously received phototherapy, standard systemic or biological drugs.
Patients with moderate to severe psoriasis showed significant improvement with apremilast compared to placebo. The effectiveness of apremilast was demonstrated in relation to a complex of clinical manifestations of psoriasis, including itching, damage to the nails and scalp, as well as quality of life.
The clinical efficacy of apremilast has been confirmed in various subgroups of patients based on baseline demographic and clinical characteristics (including duration of psoriasis and history of PsA). The positive clinical effect of the drug did not depend on previous drug therapy for psoriasis and its results. The response to apremilast treatment was rapid and was reflected in a significant reduction in psoriasis symptoms by the 2nd week of treatment, compared with placebo.
Special instructions
Patients with rare hereditary disorders such as galactose intolerance, congenital lactase deficiency or glucose-galactose malabsorption should not take this drug.
Psychiatric disorders: The use of apremilast is associated with an increased risk of developing psychiatric disorders such as insomnia and depression. Cases of suicidal thoughts and behavior, including suicide, have been observed in patients with and without a history of depression (see section “Side Effects”).
The risks and benefits of initiating and continuing apremilast therapy should be carefully assessed in patients who report a current or history of psychiatric disorders or who are planning to take other concomitant medications that may cause psychiatric disorders.
The patient and those caring for the patient should report to the prescriber any changes in the patient’s behavior or mood, as well as the appearance of suicidal thoughts. Severe renal failure: In patients with severe renal failure, the dose of Otesla should be reduced to
30 mg 1 time per day (see section “Pharmacokinetics” and “Dosage and Administration”). Patients with insufficient body weight: in patients with insufficient body weight at the beginning of therapy, it is necessary to regularly monitor body weight during treatment. In the event of unexplained or clinically significant weight loss, a thorough medical examination of the patient should be performed and discontinuation of treatment should be considered.
Effect on the ability to drive vehicles and use machines: apremilast does not affect or only slightly affects the ability to drive vehicles or operate machines.
Active ingredient
Apremilast
Composition
Active ingredient:
apremilast – 10/20/30 mg
Contraindications
Hypersensitivity to apremilast or other components included in the drug;
Pregnancy;
Breastfeeding period;
Children under 18 years of age (insufficient clinical experience);
Rare hereditary galactose intolerance, lactase deficiency, glucose-galactose malabsorption syndrome (the drug contains lactose).
With caution
In patients who have mental disorders or a history of such disorders, or if the patient is planning to take other concomitant medications that can cause mental disorders (see section “Special Instructions”).
In patients with severe renal failure (see section “Pharmacokinetics”, “Dosage and Administration”, “Special instructions”).
In patients with insufficient body weight (see section “Special instructions”).
Side Effects
The most common adverse drug reactions (ADRs) during phase III clinical trials were gastrointestinal disorders – diarrhea (15.7%) and nausea (13.9%). Most of these disorders were mild or moderate in severity, and only 0.3% of each of these ADRs were classified as severe. These ADRs occurred predominantly in the first 2 weeks of treatment and usually resolved within 4 weeks. Other common ADRs were upper respiratory tract infection (8.4%), headache (7.9%), and tension-type headache (7.2%). Overall, most ADRs were mild or moderate in severity.
Hypersensitivity reactions were rarely reported during clinical studies of apremilast. ADRs were reported during clinical trials of apremilast in psoriatic arthritis (1945 patients) and psoriasis (1184 patients). Infectious and parasitic diseases: bronchitis, upper respiratory tract infections, nasopharyngitis. Immune system disorders: hypersensitivity reactions. Metabolic and nutritional disorders: decreased appetite. Mental disorders: insomnia, depression. Nervous system disorders: migraine, tension headache, headache. Disorders of the respiratory system, chest and mediastinal organs: cough. Gastrointestinal disorders: diarrhea, nausea, vomiting, dyspepsia, frequent bowel movements, pain in the upper abdomen, gastroesophageal reflux, gastrointestinal bleeding. Skin and subcutaneous tissue disorders: skin rash. Musculoskeletal and connective tissue disorders: back pain. General disorders and administration site disorders: fatigue. Laboratory and instrumental data: loss of body weight.
Interaction
Combined use with a powerful inducer of the cytochrome P450 3A4 isoenzyme (CYP3A4), rifampicin, leads to a weakening of the systemic exposure of apremilast and a decrease in its effectiveness. Therefore, the combined use of potent inducers of the CYP3A4 isoenzyme (for example, rifampicin, phenobarbital, carbamazepine, phenytoin and St. John’s wort preparations) with apremilast is not recommended. With simultaneous repeated use of apremilast and rifampicin, the AUC and Cmax of apremilast are reduced by 72 and 43%, respectively. When apremilast is used in combination with strong inducers of the CYP3A4 isoenzyme (for example, rifampicin), the clinical response may be reduced. During clinical studies, apremilast was combined with topical therapies (corticosteroids, tar shampoo, salicylic acid preparations for treating the scalp) and with UV-B phototherapy.
No clinically significant drug interactions have been identified between ketoconazole and apremilast. Apremilast can be combined with strong CYP3A4 inhibitors such as ketoconazole.
No pharmacokinetic drug interactions were found between apremilast and methotrexate in patients with PsA. Apremilast can be combined with methotrexate.
No pharmacokinetic drug interactions have been observed between apremilast and oral contraceptives containing ethinyl estradiol and norgestimate. Apremilast can be combined with oral contraceptives.
Overdose
Apremilast was studied in healthy volunteers at a maximum daily dose of 100 mg (50 mg twice daily) for 4.5 days without evidence of dose-limiting toxicity. In case of overdose, monitoring for symptoms and signs of NDR is recommended. If necessary, symptomatic and supportive treatment is prescribed.
Storage conditions
Store at a temperature not exceeding 30°C. Keep out of the reach of children.
Shelf life
2 years.
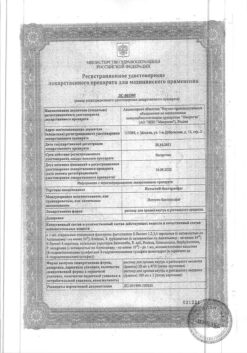
Manufacturer
Celgene International Sarles, Switzerland
| Shelf life | 2 years. |
|---|---|
| Conditions of storage | Store at a temperature not exceeding 30°C. Keep out of reach of children. |
| Manufacturer | Selgen International Sarl, Switzerland |
| Medication form | pills |
| Brand | Selgen International Sarl |
Related products
Buy Otesla, 10 mg+20 mg+30 mg+30 mg 14 pcs with delivery to USA, UK, Europe and over 120 other countries.