No products in the cart.
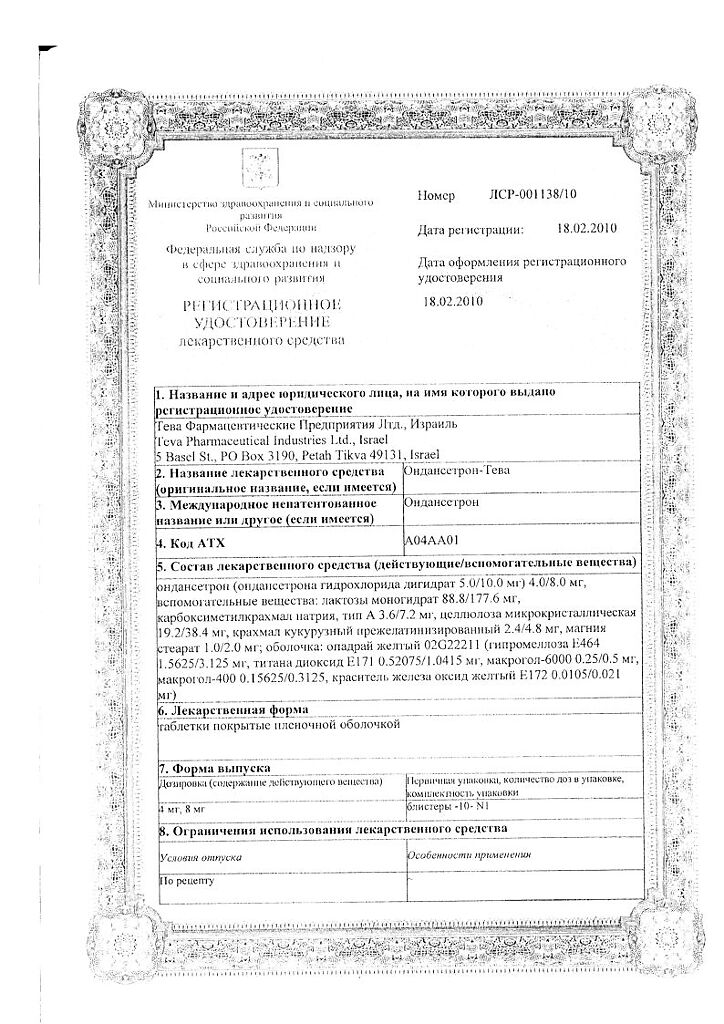
Ondansetron-Teva, 8 mg 10 pcs
€13.08 €10.90
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group: antileting agent – serotonin receptor antagonist
Kode ATX: A04AA01
Pharmacological properties.
Pharmacodynamics
Mechanism of action
Ondansetron is a potent highly selective 5NT3 receptor antagonist. The mechanism for suppressing nausea and vomiting is not precisely known. Radiation therapy and the use of cytostatic drugs may release serotonin (5NT) in the small intestine, causing the gag reflex through activation of 5NT3 receptors and excitation of vagus nerve afferent fiber endings. Ondansetron blocks initiation of this reflex.
Activation of afferent vagus nerve endings, in turn, can cause release of 5NT in the posterior floor of the fourth ventricle (area postrema) and trigger the central mechanism of the gag reflex. Thus, ondansetron suppression of nausea and vomiting caused by cytostatic chemotherapy and radiation therapy appears to be due to its antagonistic effect on 5NT3 receptor neurons located both in the peripheral and central nervous system.
The mechanisms of action of the drug in relief of postoperative nausea and vomiting have not been established, but in general they correspond to those in relief of nausea and vomiting induced by chemotherapy and radiotherapy.
Ondansetron has no effect on plasma prolactin concentrations.
Pharmacokinetics
Pharmacokinetic parameters of ondansetron do not change with repeated use.
Intake
Ondansetron is completely absorbed in the gastrointestinal tract after oral administration and is metabolized during “first passage” through the liver. Maximum plasma concentrations are reached approximately 1.5 hours after administration.
When Ondansetron-Teva is administered orally in doses greater than 8 mg, the increase in blood levels of Ondansetron is greater than proportional to its metabolism during “first passage” through the liver, which may decrease its metabolism during administration of high oral doses. The average bioavailability in healthy male volunteers after taking a single 8 mg tablet was approximately 55-60%.
Bioavailability is slightly increased when the drug is taken concomitantly with food, but does not change when taken with antacids.
Distribution
The protein-binding capacity of ondansetron is low (70-76%).
The distribution of ondansetron by oral, intramuscular and intravenous administration in adults is similar, with an equilibrium distribution of about 140 liters.
Metabolism
Ondansetron is eliminated from the systemic blood stream by metabolism in the liver with the participation of various enzyme systems. The absence of the CYP2D6 isoenzyme (sparteine-debrisoquine type polymorphism) has no effect on the pharmacokinetics of ondansetron.
Elimation
Ondansetron is eliminated from the systemic bloodstream primarily by metabolism in the liver. Less than 5% of the administered dose is excreted unchanged by the kidneys.
The distribution of ondansetron by oral administration, intramuscular or intravenous injection is similar to the elimination half-life and is about 3 hours.
Special patient groups
Gender
Pharmacokinetics of ondansetron depend on the gender of patients. Women have a higher rate, degree of absorption and lower systemic clearance, volume of distribution (values corrected for body weight) than men.
Children (ages 1 month to 18 years)
In children 1 to 4 months of age (n = 19) who underwent surgery, weight-adjusted clearance was approximately 30% slower than in patients aged 5 to 24 months (n = 22), but comparable to that in patients aged 3 to 12 years. The elimination half-life averaged 6.7 h in the 1 to 4-month-old patient group compared with 2.9 h in the 5 to 24-month and 3 to 12-year-old age groups. The differences in pharmacokinetic parameters are partially explained by the higher percentage of body fluid in newborns and infants and by the higher volume of distribution of water-soluble drugs such as ondansetron in patients aged 1 to 4 months.
In children aged 3 to 12 years who underwent elective surgery under general anesthesia, the absolute clearance and volume of distribution of ondansetron were decreased compared with those in adults. Both parameters increased linearly as a function of body weight, and in patients under 12 years of age these values approached those of adults. When the values of clearance and volume of distribution were corrected by body weight, these parameters were close in different age groups. Dose calculations based on body weight compensate for age-related changes and systemic exposure to ondansetron in children.
Based on population pharmacokinetic analysis, the AUC (area under the pharmacokinetic concentration-time curve) after oral and intravenous administration of ondansetron in children and adolescents was comparable to that in adults, except for infants aged 1 to 4 months. The volume of distribution was age-dependent and lower in adults compared with values in children.
The lirence of ondansetron depended on the patient’s body weight but was independent of age, except in infants aged 1 to 4 months. It is difficult to conclude definitively whether the decrease in ondansetron clearance in infants aged 1 to 4 months was related to their age or whether this decrease had natural variability, given the small number of patients studied in this age group. Because patients younger than 6 months of age would receive only one dose of the drug if postoperative nausea and vomiting occurred, it is likely that the decrease in clearance would not be clinically significant.
Elderly Patients
Based on data obtained ondansetron plasma concentrations as well as the results of exposure-dependent clinical response modeling, a more pronounced effect on the QTcF interval in patients aged ≥75 years is expected than in younger patients. Special intravenous dose recommendations are provided for patients aged over 65 years and over 75 years (see “Administration and Doses”).
Patients with impaired renal function
In patients with moderate renal impairment (creatinine clearance 15-60 mL/min), systemic clearance and volume of distribution are reduced after intravenous administration of ondansetron, resulting in a small clinically insignificant increase in the elimination half-life (5.4 hours). Studies in patients with severe renal impairment who require regular hemodialysis (studies were conducted between dialysis sessions) have shown no change in the pharmacokinetics of ondansetron after its intravenous administration.
Patients with impaired liver function
.In patients with severe hepatic impairment, systemic clearance of ondansetron is dramatically reduced with an increase in half-life to 15-32 hours and oral bioavailability reaches 100% due to reduced presystemic metabolism.
Indications
Indications
Prevention and treatment of nausea and vomiting caused by cytostatic chemotherapy and radiation therapy in adults.
The prevention and treatment of nausea and vomiting caused by cytostatic chemotherapy in children.
Prevention of postoperative nausea and vomiting in adults.
Active ingredient
Active ingredient
Composition
Composition
How to take, the dosage
How to take, the dosage
The drug is intended to be taken orally.
Prevention and treatment of nausea and vomiting caused by cytostatic chemotherapy and radiotherapy in adults
The choice of dosing regimen is determined by the emetogenicity of anticancer therapy.The choice of dosing regimen is determined by the emetogenicity of antitumor therapy and may vary depending on the dose and combinations of chemotherapy and radiation therapy regimens used.
The recommended dose is 8 mg ondansetron 1-2 hours before cytostatic chemotherapy or radiation therapy followed by 8 mg orally every 12 hours for no more than 5 days.
In high-emetogenic chemotherapy, the single dose of oral ondansetron is 24 mg concomitantly with oral dexamethasone at a dose of 12 mg 1-2 hours before chemotherapy.
In the first 24 hours after chemotherapy or radiation therapy, the oral dosage of Ondansetron-Teva may continue for no more than 5 days. The recommended dose of Ondansetron-Teva is 8 mg twice daily.
Patient Special Groups
Elderly Patients
.There is no need to adjust the dose and frequency of Ondansetron-Teva in oral dosage form for elderly patients.
Patients with impaired renal function
The daily dose, dosing frequency or route of administration of ondansetron does not require adjustment.
Patients with hepatic impairment
In patients with moderate to severe hepatic impairment, ondansetron clearance is significantly reduced and the elimination half-life is significantly prolonged.
The daily dose of ondansetron in these patients should not exceed 8 mg.
Patients with slow sparteine-debrisoquine metabolism
In patients with slow sparteine-debrisoquine metabolism, the half-life of ondansetron is unchanged. Consequently, when such patients are reintroduced with ondansetron, its plasma concentration will not differ from that in the general population. Therefore, no adjustment of the daily dose or dosing frequency of ondansetron is necessary in this case.
Prevention and treatment of nausea and vomiting caused by cytostatic chemotherapy in children (3 to 17 years inclusive)
The dose of Ondansetron-Teva in children is calculated based on surface area or body weight.
Dose calculation based on body surface area
.Ondansetron-Teva, intravenous and intramuscular solution may be given as a single intravenous injection at a dose of 5 mg/m2 (max. 8 mg) immediately before chemotherapy (see the instructions for medical use of the drug. Instructions for medical use of the drug Ondansetron-Teva, solution for intravenous and intramuscular injection) with subsequent oral administration of the drug after 12 hours. Oral administration of Ondansetron-Teva may be continued for another 5 days after the course of chemotherapy. When using the drug in this age group the doses used in adults should not be exceeded.
Gel surface area
Day 1
Day 2-6
⥠0.6 m2 and ⤠1.2 m2
5 mg/m2 intravenously, then
4 mg ondansetron after 12 h
4 mg ondansetron
every 12 h
> 1.2 m2
5 mg/m2 intravenously or 8 mg
intravenously, then
8 mg of ondansetron after 12 h
8 mg ondansetron
every 12 h
Dose calculation table based on body surface area in children aged 3 to
17 years for the prevention and treatment of nausea and vomiting caused by chemotherapy
/td>
Dose calculation based on body weight
Ondansetron-Teva, intravenous and intramuscular solution should be administered once intravenously immediately before the start of chemotherapy (see Instructions for Medical Use for details). Instructions for medical use of Ondansetron-Teva, solution for intravenous and intramuscular injection) with subsequent oral administration of Ondansetron-Teva 12 hours after the start of therapy. Oral administration of Ondansetron-Teva may be continued for another 5 days after chemotherapy. When using the drug in patients in this age category, the doses used in adults should not be exceeded.
Dose calculation table based on body weight in children aged 3 to 17 years inclusive for prevention and treatment of chemotherapy-induced nausea and vomiting
Body weight
Day 1
Day 2-6
> 10 kg
Up to 3 doses of 0.15mg/kg intravenously, every 4 h
4 mg ondansetron every 12 h
Prevention of postoperative nausea and vomiting in adults
In order to prevent nausea and vomiting in the postoperative period, we recommend taking 16 mg of Ondansetron-Teva orally 1 hour before anesthesia.
To treat postoperative nausea and vomiting, Ondansetron-Teva is used in the dosage form of an intravenous and intramuscular solution.
Patient Special Groups
Children aged 3 to 17 years inclusive
There have been no studies of the oral dosage form of Ondansetron-Teva for the prevention or treatment of nausea and vomiting in the postoperative period; The use of Ondansetron-Teva, intravenous and intramuscular solution in the form of slow intravenous injections (lasting at least 30 seconds) is recommended for this purpose.
Elderly patients
There is limited experience with ondansetron for the prevention of postoperative nausea and vomiting in elderly patients, although ondansetron is well tolerated in patients 65 years and older receiving chemotherapy.
Patients with impaired renal function
Correction of the daily dose, dosing frequency or route of administration of ondansetron is not necessary. Patients with hepatic impairment
In patients with moderate to severe hepatic impairment, ondansetron clearance is significantly reduced and the elimination half-life is significantly prolonged.
The daily dose of ondansetron in these patients should not exceed 8 mg.
Patients with slow sparteine-debrisoquine metabolism
In patients with slow sparteine-debrisoquine metabolism, the half-life of ondansetron is unchanged. Consequently, when such patients are reintroduced with ondansetron, its plasma concentration will not differ from that in the general population. Therefore, there is no need to adjust the daily dose or dosing frequency of ondansetron in this case.
Interaction
Interaction
There is no evidence that ondansetron induces or inhibits the metabolism of other drugs commonly used in combination with it. Special studies have shown that ondansetron does not interact pharmacokinetically with ethanol, temazepam, furosemide, tramadol or propofol.
Ondansetron is metabolized by several cytochrome P450 isoenzymes in the liver: CYP3A4, CYP2D6 and CYP1A2. Due to the variety of isoenzymes capable of metabolizing ondansetron, inhibition of isoenzymes or decrease in activity of one of the isoenzymes (for example, in genetic deficiency of CYP2D6) is usually compensated by other isoenzymes, as a result, there are either no or little changes in total clearance of ondansetron and doses need not be adjusted. Caution should be exercised when using ondansetron with drugs that affect QT interval prolongation and/or cause electrolyte imbalance or decreased heart rate.
Apomorphine
Based on the evidence of profound hypotension and loss of consciousness during use of ondansetron with apomorphine hydrochloride, simultaneous use of ondansetron with apomorphine is contraindicated.
Phenytoin, carbamazepine and rifampicin
In patients treated with potent CYP3A4 inducers (phenytoin, carbamazepine and rifampicin), ondansetron clearance when taking the drug orally was increased and ondansetron blood concentration was decreased.
Serotonergic drugs (e.g., SSRIs (selective serotonin reuptake inhibitors) and SSRIs (selective norepinephrine and serotonin reuptake inhibitors))
The combined use of ondansetron and other serotonergic drugs, including SSRIs and SSRIs, has been found to increase the risk of serotonin syndrome (including altered consciousness, peripheral nervous system instability, and neuromuscular disorders) (see See section “Special Indications”).
Tramadol
There are data from small studies indicating that ondansetron may decrease the analgesic effect of tramadol.
Special Instructions
Special Instructions
There have been reports of hypersensitivity reactions to ondansetron in patients with a history of hypersensitivity to other selective 5HT-receptor antagonists.
It is known that ondansetron prolongs the time of passage of contents through the large intestine, if the drug is used in patients with symptoms of subacute intestinal obstruction, regular monitoring is required.
Ondansetron causes dose-dependent prolongation of the QT interval. In addition, cases of pirouette-type ventricular tachycardia have been reported in patients receiving ondansetron during post-registration follow-up.
Hypokalemia and hypomagnesemia should be corrected prior to ondansetron administration.
It has been found that concomitant use of ondansetron and other serotonergic drugs increases the risk of serotonin syndrome (see section “Interaction with other medicinal products”). If concomitant use of ondansetron and other serotonergic drugs is clinically justified, the patient should be monitored regularly.
Effects on driving and operating machinery
In case of adverse reactions on the nervous system, patients are recommended to refrain from driving vehicles and other machinery as well as activities requiring concentration and rapid psychomotor functions.
Synopsis
Synopsis
Contraindications
Contraindications
High sensitivity to the active ingredient or any other ingredient in the drug.
With caution
In patients with hypersensitivity to other 5HT3-receptor antagonists, with cardiac rhythm and conduction disorders; in patients receiving antiarrhythmic agents and beta-adrenoblockers; in patients with significant abnormalities of water-electrolyte balance; patients with prolongation or risk of QTc interval prolongation, including patients with electrolyte-water balance disorders, chronic heart failure, bradyarrhythmia, or patients taking other medications that may cause QT interval prolongation or electrolyte-water balance disorders or decreased heart rate in patients with subacute intestinal obstruction; in patients with lactase deficiency, lactose intolerance, glucose-galactose malabsorption syndrome; when concomitantly used with other serotonergic drugs.
Side effects
Side effects
The adverse reactions presented below are listed according to organ and organ system involvement and frequency of occurrence.
Frequency is defined as follows: very frequently (â¥1/10), frequently (â¥1/100 and <1/10), infrequently (â¥1/1000 and <1/100), rarely (â¥1/10000 and <1/1000), very rarely (<1/10000, including individual cases).
Unwanted reactions observed “very frequently,” “frequently,” and “infrequently” were generally determined from clinical trial data. The frequency of occurrence with placebo was also taken into account. Adverse reactions observed “infrequently” and “very rarely” were determined based on spontaneous reports from post-registration surveillance.
The incidence rate for standard recommended doses of ondansetron was established as shown below. The profile of adverse reactions in children and adolescents was comparable to that observed in adults.
Immune system disorders
Rarely: immediate hypersensitivity reactions (urticaria, bronchospasm, laryngospasm, angioedema), in some cases of severe degree, including anaphylaxis.
Nervous system disorders
Very common: headache. Infrequent: seizures, motor disorders (including extrapyramidal symptoms such as dystonia, oculogyric crisis (gaze cramp) and dyskinesia) in the absence of persistent clinical effects. Rare: Dizziness, mainly during rapid intravenous administration.
Visual disturbances
Rare: Transient visual disturbances (e.g., blurred vision), mainly during intravenous administration. Very rare: transient blindness, mainly during intravenous administration. Most cases of blindness resolved safely within 20 min. Most patients received chemotherapy drugs containing cisplatin. In some cases transient blindness was of cortical genesis.
Cardiac disorders
Infrequent: arrhythmia, chest pain, with or without ST-segment decreases, bradycardia. Rare: QT interval prolongation (including pirouette-type ventricular tachycardia). Infrequent: decreased blood pressure.
Respiratory system, thorax and mediastinum disorders
Infrequent: hiccups.
Gastrointestinal tract disorders
Frequent: constipation.
Hepatic and biliary tract disorders
Infrequent: asymptomatic increased activity of “hepatic” enzymes alanine aminotransferase (ALT), aspartate aminotransferase (AST) (mainly observed in patients receiving cisplatin chemotherapy).
Skin and subcutaneous tissue disorders
Very rare: toxic skin rash, including toxic epidermal necrolysis.
Overdose
Overdose
Symptomatics
There are currently insufficient data regarding ondansetron overdose. In most cases, the symptoms of overdose were similar to the adverse events reported in patients receiving the recommended doses. Ondansetron causes dose-dependent prolongation of the QT interval. ECG monitoring is recommended in case of drug overdose. In case of drug overdose when taken orally in children, symptoms indicative of serotonin syndrome have been reported.
Treatment
There is no specific antidote, so if overdose is suspected, appropriate symptomatic and supportive therapy is recommended. Further treatment should be based on the clinical situation. The use of ipecacuana for treatment of drug overdose is not recommended because patients are unlikely to respond to treatment with ipecacuana due to the antiemetic effects of ondansetron.
The use of ipecacuana for treatment of drug overdose is not recommended.
Pregnancy use
Pregnancy use
Pregnancy
The safety of ondansetron during pregnancy in humans has not been established. Preclinical studies have shown no direct or indirect adverse effects on embryonic, fetal, gestational, peri- and postnatal development. However, the use of ondansetron in pregnant women is contraindicated due to the fact that the results of preclinical studies cannot always be extrapolated to the safety of use in humans.
Data on the safety of ondansetron in pregnancy are limited, and available pharmacoepidemiological studies are inconsistent.
Post-registration reports have described cases of congenital abnormalities after ondansetron use during pregnancy, but there is insufficient information from these reports to establish a causal relationship.
Breastfeeding
It has not been determined whether Ondansetron-Teva passes into human breast milk. There are no data on the effect of Ondansetron-Teva on the breastfed child and on breast milk production. Studies have shown that ondansetron penetrates into breast milk of lactating animals. Breastfeeding should be stopped if ondansetron is used in breastfeeding mothers (see section “Contraindications”).
Women and men of preserved reproductive potential
Pregnancy testPregnancy test
Similarities
Similarities
Additional information
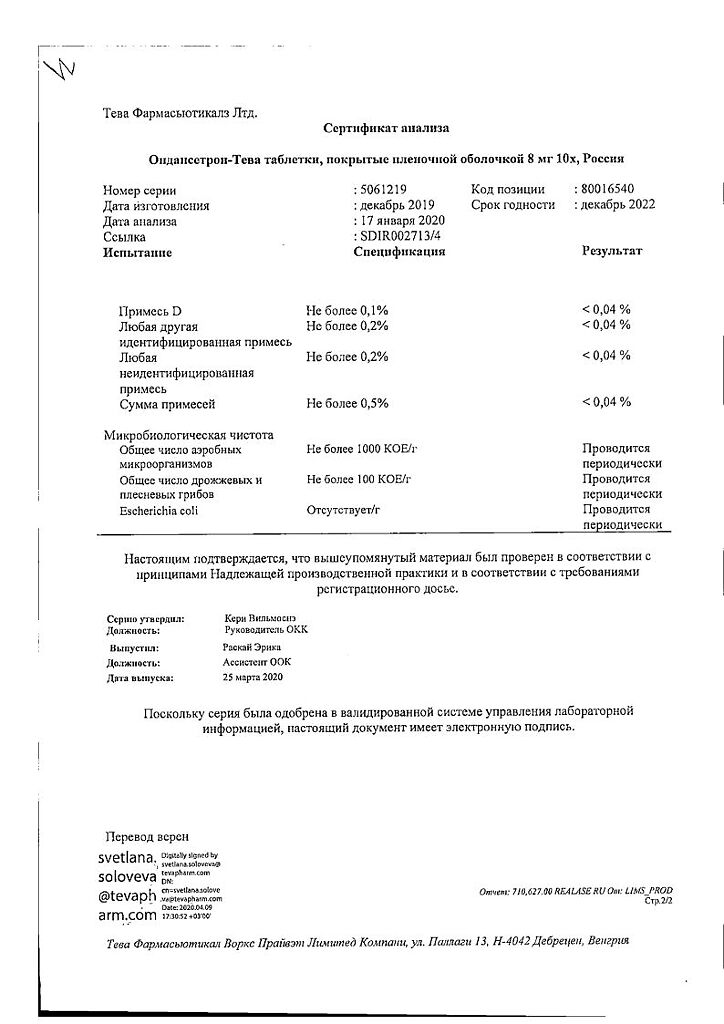
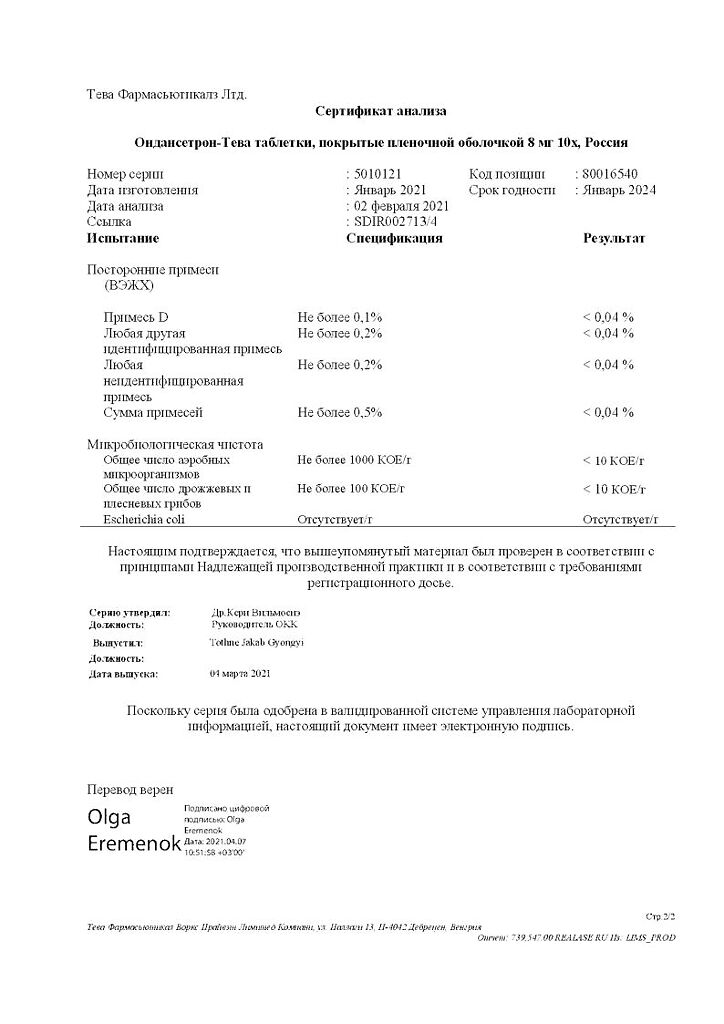
| Weight | 0.010 kg |
|---|---|
| Shelf life | 3 years. |
| Conditions of storage | In a light-protected place at a temperature not exceeding 25 °C. |
| Manufacturer | Teva Pharmaceutical Works Production Limited Company, Hungary |
| Medication form | pills |
| Brand | Teva Pharmaceutical Works Production Limited Company |
Related products
Buy Ondansetron-Teva, 8 mg 10 pcs with delivery to USA, UK, Europe and over 120 other countries.