No products in the cart.
Octreotide depot, lyophilizate 10 mg
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group: Hypothalamic-pituitary hormones and their analogs. Hormones of hypothalamus. Growth retarding hormones. Octreotide.
ATC code: H01CV02
Pharmacological properties
Pharmacokinetics
Octreotide is completely absorbed when administered intramuscularly.
Therapeutic concentration in the blood is reached after approximately 30 minutes.
Protein binding is about 65%. The binding of octreotide to blood cells is extremely low. The volume of distribution is 0.27 l/kg. Octreotide is metabolized in the liver.
The total clearance is 160 ml/min. The T1/2 is 100 min. About 32% is excreted unchanged by the kidneys. In elderly patients the clearance is decreased and the T1/2 is increased. In severe renal failure clearance is reduced by half.
Pharmacodynamics
Octreotide depot is a synthetic octapeptide derived from the natural hormone somatostatin and has similar pharmacological effects to it but longer duration of action. The drug suppresses pathologically increased secretion of growth hormone (GH), as well as peptides and serotonin produced in the gastro-entero-pancreatic endocrine system.
In carcinoid tumors, use of Octreotide leads to a reduction of symptoms such as flushing and diarrhea, which in many cases is accompanied by a decrease in plasma serotonin concentrations and urinary excretion of 5-hydroxyindoleacetic acid.
In tumors characterized by hyperproduction of vasoactive intestinal peptide (VIPoma), use of Octreotide leads to reduction of severe secretory diarrhea. At the same time there is a decrease in the accompanying electrolyte balance disorders. In some patients there is a slowing or stopping of tumor progression and even a reduction of its size, especially of liver metastases. Clinical improvement is usually accompanied by a decrease (down to normal values) of plasma concentration of vasoactive intestinal peptide (VIP).
In glucagonomas, use of Octreotide-depo in most cases results in a marked reduction of necrotizing migratory rash. Octreotide Depot has no significant effect on the severity of diabetes mellitus often seen in glucagonomas and usually does not result in a reduced need for insulin or oral antidiabetic drugs. In patients with diarrhea, Octreotide causes a decrease in diarrhea, which is accompanied by an increase in body weight. When using Octreotide, a rapid decrease in plasma glucagon concentration is often observed, but this effect does not persist with long-term treatment. At the same time, symptomatic improvement remains stable for a long time.
In gastrinomas/Zollinger-Ellison syndrome, Octreotide Depot used as monotherapy or in combination with H2-receptor blockers can reduce acid production in the stomach and lead to clinical improvement, including for diarrhea. The severity of other symptoms, including hot flashes, is also reduced. In some cases, there is a decrease in plasma gastrin concentrations.
In patients with insulinomas, Octreotide depot decreases the level of immunoreactive insulin in the blood (this effect may be transient, about 2 hours). In patients with operable tumors, Octreotide Depot can provide restoration and maintenance of normoglycemia in the preoperative period. In patients with inoperable benign and malignant tumors, glycemic control may improve without simultaneous prolonged decrease in blood insulin levels.
In refractory diarrhea in patients with acquired immunodeficiency syndrome (AIDS), use of Octreotide leads to complete or partial stool normalization in approximately 1/3 of patients with diarrhea uncontrolled by adequate therapy with antimicrobials and/or antidiarrheals.
In patients undergoing pancreatic surgery, the use of Octreotide during and after surgery reduces the incidence of typical postoperative complications (e.g., pancreatic fistulas, abscesses, sepsis, postoperative acute pancreatitis).
In bleeding from esophageal and gastric varices in patients with cirrhosis, use of Octreotide Depot in combination with specific treatment (e.g., sclerosing therapy) leads to more effective stopping of bleeding and early rebleeding, reduction of transfusion volume and improvement of 5-day survival. The drug reduces organ blood flow by inhibiting vasoactive hormones such as VIP and glucagon.
Indications
Indications
In therapy of endocrine tumors of the gastrointestinal tract (GIT) and pancreas
– carcinoid tumors with phenomena of carcinoid syndrome
– insulinomas
– VIPomas
– gastrinomas (Zollinger-Ellison syndrome)
– glucagonomas (for control of preoperative hypoglycemia as well as for maintenance therapy)
– somatoliberinomas (tumors characterized by hyperproduction of growth hormone releasing factor)
In therapy of hormone resistant prostate cancer
– As part of combination therapy against the background of surgical or medical castration
In the prevention of the development of acute postoperative pancreatitis
– In extensive abdominal and thoracoabdominal surgical interventions (including gastric, esophageal, colorectal, pancreatic cancer, primary and secondary tumor involvement of the liver).
Active ingredient
Active ingredient
Composition
Composition
One bottle contains
The active ingredient – octreotide 10.0 mg,
Auxiliary substances: copolymer of DL-lactic and glycolic acids, D-Mannit, carboxymethylcellulose sodium salt, polysorbate-80.
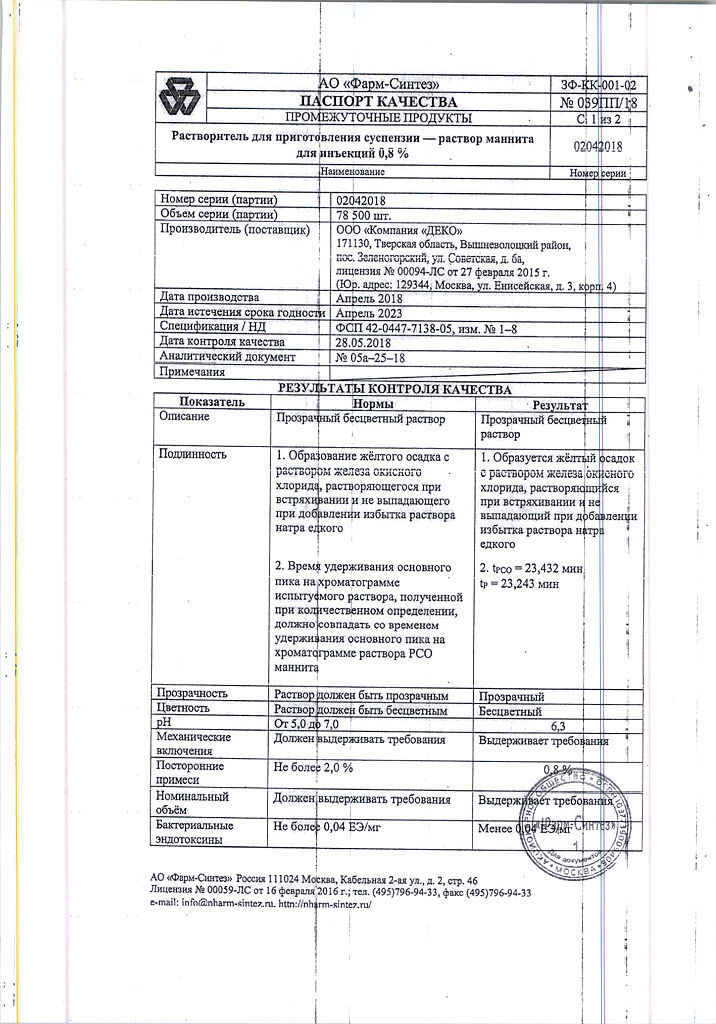
Solvent: D-Mannitol, water for injection.
How to take, the dosage
How to take, the dosage
Octreotide Depot should only be injected deeply intramuscularly (v/m), into the gluteal muscle. For repeated injections the left and right side should be alternated. Suspension should be prepared immediately before injection. On the day of injection, the bottle with the drug and the ampoule with the solvent can be kept at room temperature.
In the treatment of endocrine tumors of the gastrointestinal tract and pancreas
In patients in whom B/C administration of Octreotide provides adequate control of the manifestations of the disease, the recommended starting dose of Octreotide depot is 20 mg every 4 weeks. The oral administration of Octreotide should be continued for an additional 2 weeks after the first administration of Octreotide depot.
In patients who have not previously received oral Octreotide, it is recommended that treatment begin with an oral dose of 0.1 mg 3 times daily for a relatively short period of time (approximately 2 weeks) to evaluate its efficacy and overall tolerability. Only after that should Octreotide depot be administered according to the above scheme.
In cases where therapy with Octreotide Depot for 3 months provides adequate control of clinical manifestations and biological markers of the disease, it is possible to reduce the dose of Octreotide Depot to 10 mg administered every 4 weeks. In cases where only partial improvement has been achieved after 3 months of treatment with Octreotide depot, the dose may be increased to 30 mg every 4 weeks. During treatment with Octreotide-depo on some days, clinical manifestations typical for endocrine tumors of the gastrointestinal tract and pancreas may worsen. In these cases, additional p/c injection of Octreotide at the dose used before the start of treatment with Octreotide-depo is recommended. This may occur primarily during the first 2 months of treatment until therapeutic plasma concentrations of Octreotide are achieved.
In the treatment of hormone-resistant prostate cancer, the recommended initial dose of Octreotide Depot is 20 mg every 4 weeks for 3 months. Subsequently, the dose is adjusted according to changes in serum PSA concentrations and clinical symptoms. If after 3 months of treatment it was not possible to achieve adequate clinical and biochemical effect (decrease of PSA), the dose can be increased to 30 mg administered every 4 weeks.
The treatment with octreotide depot is combined with the use of dexamethasone, which is administered orally according to the following regimen: 4 mg daily for 1 month, then 2 mg daily for 2 weeks, then 1 mg daily (maintenance dose).
The treatment with octreotide depot and dexamethasone is combined with the use of a gonadotropin-releasing hormone (GnRH) analogue in patients who were previously treated with medication-assisted antiandrogen therapy. The GnRH analogue (depot form) is injected once every 4 weeks.
Patients receiving Octreotide depot should have their PSA concentrations determined every month.
In patients with impaired renal function, hepatic function and in elderly patients there is no need to adjust the dosing regimen of Octreotide depot.
To prevent acute postoperative pancreatitis
The drug Octreotide Depot in a dose of 10 or 20 mg is administered once no earlier than 5 days and no later than 10 days before the proposed surgical intervention.
Regulations for suspension preparation and administration
The drug is administered intramuscularly only.
The suspension for intramuscular injection is prepared using the included solvent immediately prior to administration.
The drug should only be prepared and administered by trained medical personnel.
Before injection, the ampoule with the solvent and the bottle of drug must be taken out of the refrigerator and brought to room temperature (30-50 minutes required).
The vial of Octreotide depot should be held upright. Gently tap the vial to ensure that all the lyophilizate is at the bottom of the vial.
open the diluent ampoule, draw the entire contents of the diluent ampoule into the syringe, and set the syringe to 3.5 ml.
Remove the plastic cap from the vial containing the lyophilizate. Disinfect the rubber stopper of the vial with an alcohol swab. Insert the needle into the vial with the lyophilizate through the center of the rubber stopper and carefully inject the solvent along the inner wall of the vial without touching the contents of the vial with the needle. Remove the syringe from the vial.
The vial should remain still until the lyophilizate is completely saturated with the solvent and a suspension is formed (approximately 3 to 5 minutes). After that, without turning the vial over, one should check the presence of dry lyophilizate at the walls and bottom of the vial. If you find dry lyophilizate residue, leave the vial until it is completely saturated.
After confirming that there is no residual dry lyophilizate, stir the contents of the vial gently in a circular motion for 30 to 60 seconds to form a homogeneous suspension. Do not invert or shake the vial; this may cause flakes to fall out and the suspension to become unusable.
Insert the needle quickly through the rubber stopper into the vial. Then lower the needle down, tilting the vial at a 45 degree angle, slowly draw the entire suspension into the syringe. Do not invert the vial as you draw. A small amount of drug may remain on the walls and bottom of the vial. Consumption for residue on the walls and bottom of the vial is counted.
After aspirating the suspension, replace the pink pavilion needle with the green pavilion needle (0.8 x 40 mm), gently invert the syringe, and deflate the syringe.
The Octreotide Depot suspension should be administered immediately after preparation.
The Octreotide Depot suspension should not be mixed with any other drug in the same syringe.
Use an alcohol swab to disinfect the injection site. Insert the needle deep into the gluteal muscle, then pull the syringe plunger back slightly to make sure there is no vessel damage. Slowly inject the suspension intramuscularly with constant pressure on the syringe plunger.
If you hit a blood vessel, change the injection site and needle.
If the needle becomes blocked, replace it with another needle of the same diameter.
The left and right sides should be alternated for repeated injections.
Interaction
Interaction
Octreotide reduces absorption of cyclosporine and slows down absorption of cimetidine. It is necessary to correct the dosing regimen of concomitantly used diuretics, beta-adrenoblockers, “slow” calcium channel blockers, insulin, oral hypoglycemic drugs.
In concomitant use of Octreotide and bromocriptine the bioavailability of the latter increases.
Drugs metabolized by cytochrome P450 enzymes with a narrow therapeutic dose range should be administered with caution.
Special Instructions
Special Instructions
In pituitary tumors secreting GH, patients receiving Octreotide Depot should be closely monitored, since tumors may increase in size with the development of serious complications such as narrowed visual fields. In these cases, other treatments should be considered.
Thyroid function should be monitored in patients undergoing long-term treatment with Octreotide depot.
There have been rare reports of bradycardia when using Octreotide. This may necessitate dose adjustments for drugs such as beta-blockers, calcium channel blockers, or drugs used to control water-electrolyte balance.
In 10-20% of patients receiving Octreotide Depot for a long time, gallstones may occur, so the following recommendations should be considered.
Management recommendations for patients during treatment with Octreotide Depot regarding gallstone formation.
Before prescribing Octreotide-depo, patients should have an initial gallbladder ultrasound;
People should have repeat ultrasound examinations of the gallbladder during treatment with Octreotide-depo, preferably at 6-12 month intervals;
If stones are detected before treatment begins, the potential benefits of Octreotide Depot therapy should be evaluated against the possible risks associated with the presence of gallstones. There is no evidence of any adverse effect of Octreotide Depot on the course or prognosis of pre-existing gallstones.
Management of patients in whom gallstones form during treatment with Octreotide-depo.
(a) Asymptomatic gallstones.
The use of Octreotide Depot can be discontinued or continued – according to the benefit/risk assessment. In either case, there is no need to do anything other than continue monitoring, making it more frequent if necessary.
b) Gallstones with clinical symptoms.
The use of Octreotide depot can be discontinued or continued – according to the benefit/risk assessment. In any case, the patient should be treated in the same way as in other cases of gallstone disease with clinical manifestations. Medical treatment includes combinations of bile acids (for example, chenodeoxycholic acid at a dose of 7.5 mg/kg per day with the same dose of ursodeoxycholic acid) with ultrasound monitoring until the stones have completely disappeared.
In patients with insulinomas during treatment with Octreotide-depo an increase in the severity and duration of hypoglycemia may be observed (this is due to a more pronounced suppressive effect on GH and glucagon secretion than on insulin secretion, as well as a shorter duration of inhibitory effect on insulin secretion). Such patients should be closely monitored at the beginning of treatment with Octreotide depot, as well as at each change of the drug dose. Significant fluctuations in blood glucose concentrations may be attempted to reduce by administering Octreotide Depot more frequently.
During bleeding from esophageal and gastric varices, patients with cirrhosis have an increased risk of developing insulin-dependent diabetes, and there may be changes in insulin requirements in diabetic patients; therefore, systematic monitoring of blood glucose concentrations is necessary in these cases.
In patients with type I diabetes mellitus, Octreotide Depot may decrease the need for insulin. In patients without diabetes mellitus and with type 2 diabetes with partially preserved insulin secretion, administration of Octreotide Depot may result in a postprandial increase in blood glucose.
In some patients, Octreotide may alter intestinal fat absorption, decrease vitamin B12 blood levels, and cause abnormal Shilling test values.
Pregnancy and lactation
There is no experience of using the drug in pregnancy; in such cases, the drug is prescribed only for absolute indications. Breast-feeding should be stopped during treatment with Octreotide-depo.
Pediatric use
There is no experience of using Octreotide-depo in children.
Particular effects of the drug on driving or potentially dangerous machinery
Some side effects of Octreotide Depot may adversely affect the ability to drive vehicles and other mechanisms requiring increased concentration and rapid psychomotor reactions.
Synopsis
Synopsis
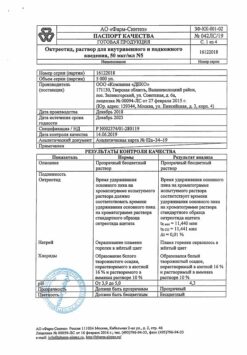
Lyophilized powder or porous, compacted into a tablet, mass of white or white with a slight yellowish tint.
Solvent: colorless clear liquid
Preconstituted suspension: When the solvent is added and shaken, a homogeneous suspension of white or white with a faint yellowish tint is formed. The reconstituted suspension should not separate for at least 5 minutes. When standing, the suspension precipitates, but resuspends easily when shaken. The suspension should flow freely into the syringe through the #0840 needle.
Contraindications
Contraindications
– hypersensitivity to octreotide or other components of the drug.
With caution:
– cholelithiasis
– diabetes mellitus
– pregnancy and lactation
Side effects
Side effects
Adverse reactions are presented based on frequency of occurrence in the following order: very often (â¥1/10); often (â¥1/100,
Overdose
Overdose
Symptoms: short-term slowing of heart rate, feeling of “rush” of blood to the face, spastic abdominal pain, diarrhea, nausea, feeling of emptiness in the stomach.
Treatment: symptomatic.
Similarities
Similarities
Additional information
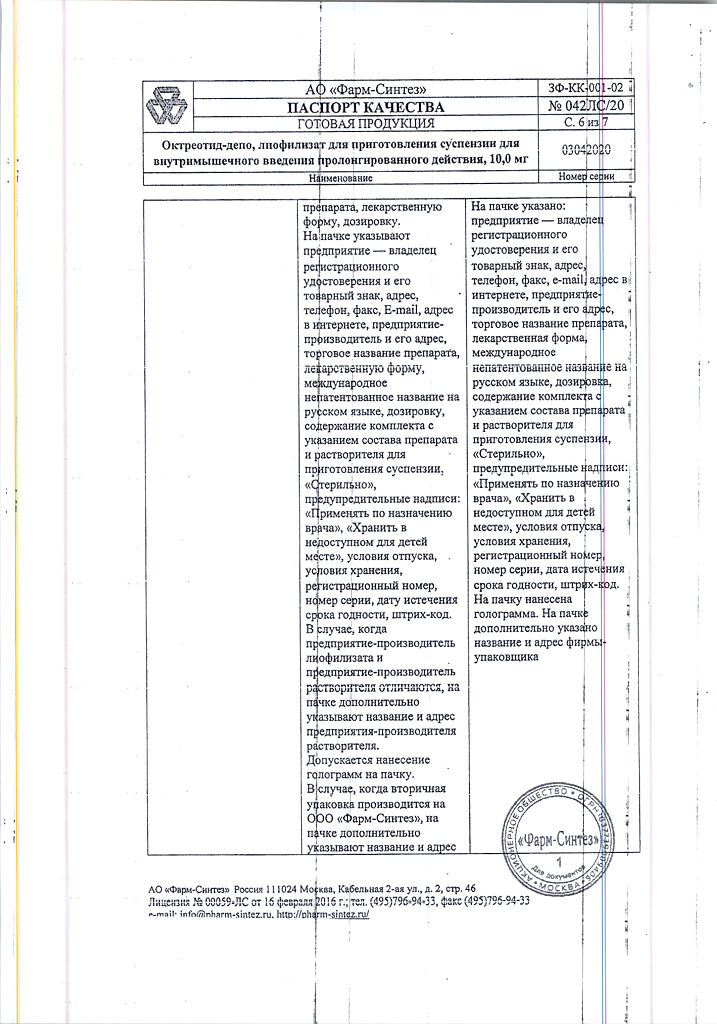
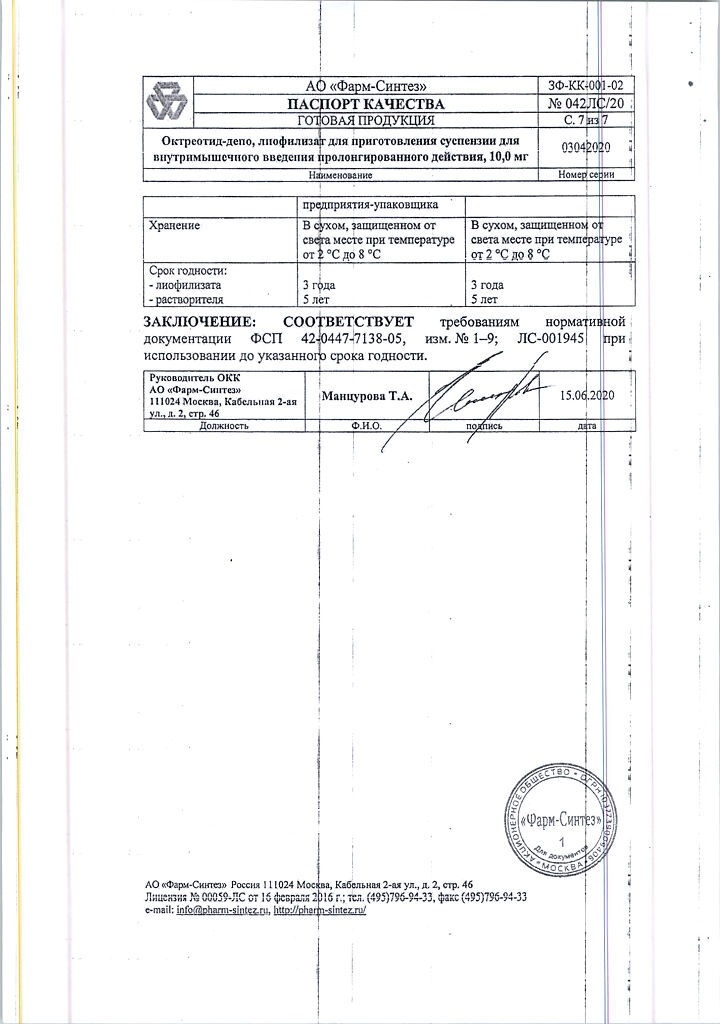
| Shelf life | Lyophilizate – 3 years Solvent – 3 years Do not use after the expiration date stated on the package. |
|---|---|
| Conditions of storage | In a dry, light-protected place at a temperature of 2 °C to 8 °C. Store out of the reach of children! |
| Manufacturer | Pharm-Sintez, Russia |
| Medication form | lyophilizate |
| Brand | Pharm-Sintez |
Related products
Buy Octreotide depot, lyophilizate 10 mg with delivery to USA, UK, Europe and over 120 other countries.