No products in the cart.
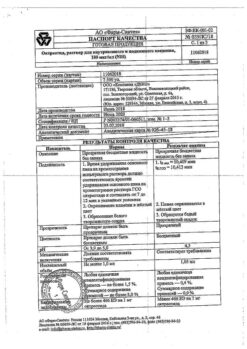
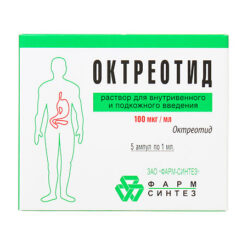
Octreotide,. 50 µg/ml 1 ml 10 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Octreotide is a synthetic analog of somatostatin, which is a derivative of the natural hormone somatostatin and has similar pharmacological effects to it, but a much longer duration of action.
Octreotide suppresses growth hormone secretion, both pathologically increased and caused by arginine, exercise and insulin hypoglycemia.
The drug also suppresses insulin, glucagon, gastrin, and serotonin secretion, both pathologically elevated and induced by food intake; it also suppresses arginine-stimulated insulin and glucagon secretion. Octreotide suppresses thyrotropin secretion induced by thyreoliberin.
In contrast to somatostatin, octreotide suppresses growth hormone secretion to a greater extent than insulin secretion, and its administration is not accompanied by subsequent hormone hypersecretion (such as growth hormone in acromegaly patients).
In patients with acromegaly, octreotide reduces plasma concentrations of growth hormone and insulin-like growth factor (IGF-1). Decrease of growth hormone concentration by 50% or more is noted in 90% of patients, and the value of growth hormone concentration of at least 5 ng/ml is achieved in about half of patients.
In most patients with acromegaly, octreotide reduces the severity of headache, soft tissue swelling, hyperhidrosis, joint pain and paresthesias. In patients with large pituitary adenomas, treatment with Octreotide may lead to some reduction in tumor size.
In secreting tumors of the gastroenteropancreatic endocrine system in cases of insufficient effectiveness of therapy (surgery, hepatic artery embolization, chemotherapy, including streptozotocin and fluorouracil) administration of Octreotide may lead to improvement of the disease course.
In carcinoid tumors, for example, administration of Octreotide may decrease the severity of facial flushing and diarrhea, which in many cases is accompanied by decreased plasma serotonin concentrations and renal excretion of 5-hydroxyindoleacetic acid.
In tumors characterized by hyperproduction of vasoactive intestinal peptide (VIPOM), use of octreotide leads in most patients to reduction of severe secretory diarrhea and, accordingly, improvement of patient’s quality of life.
At the same time there is a reduction of concomitant electrolyte disturbances, such as hypokalemia, which allows to cancel enteral and parenteral administration of fluids and electrolytes.
In some patients the progression of the tumor is slowed or stopped, its size and the size of liver metastases are reduced. Clinical improvement is usually accompanied by a decrease in plasma concentration of vasoactive intestinal peptide (VIP) or its normalization.
In glucagonomas, use of Octreotide results in a reduction of erythema migrans. Octreotide has no significant effect on the severity of hyperglycemia in diabetes mellitus, and the need for insulin or oral hypoglycemic agents usually remains unchanged. The drug causes reduction of diarrhea, which is accompanied by an increase in body weight.
While decrease in plasma glucagon concentration under the influence of Octreotide is transient, the clinical improvement remains stable during the whole period of using the drug.
In patients with gastrinomas/Zollinger-Ellison syndrome, when using octreotide as monotherapy or in combination with proton pump inhibitors or H blockers2-histamine receptor blockers may decrease gastric hydrochloric acid hypersecretion, decrease plasma gastrin concentrations, and decrease the severity of diarrhea and flushes.
In patients with insulinomas, octreotide decreases the level of immunoreactive insulin in the blood (this effect may be short-lived, about 2 hours).
In patients with operable tumors, Octreotide may provide restoration and maintenance of normoglycemia in the preoperative period. In patients with inoperable benign and malignant tumors, glycemic control may improve without concomitant prolonged reduction in blood insulin levels.
In patients with rare tumors hyperproducing the growth hormone releasing factor (somatoliberinomas), octreotide reduces the severity of acromegaly symptoms. This is due to the suppression of growth hormone releasing factor and growth hormone secretion itself. Subsequently, hypertrophy of the pituitary gland may decrease.
In bleeding from esophageal and gastric variceal veins in cirrhotic patients, use of octreotide in combination with specific treatments (such as sclerosing therapy) results in more effective bleeding arrest and early rebleeding, reduced transfusion volume and improved 5-day survival.
The mechanism of action of octreotide is thought to be related to reduction of organ blood flow through suppression of vasoactive hormones such as VIP and glucagon.
Pharmacokinetics
Intake
After p/k administration, octreotide is quickly and completely absorbed. Tmax of Octreotide in plasma is within 30 min.
Distribution
The binding to plasma proteins is 65%. The binding of Octreotide to blood cells is extremely insignificant. Vd is 0.27 l/kg.
Excretion
T1/2 after p/c administration of Octreotide is 100 min. After IV administration, excretion of Octreotide occurs in 2 phases, with T1/2 of 10 and 90 min, respectively. Most part of octreotide is excreted through the intestine, about 32% – unchanged by the kidneys. Total clearance is 160 ml/min.
Indications
Indications
The drug is not antitumor and its use is not expected to cure this category of patients.
Active ingredient
Active ingredient
Composition
Composition
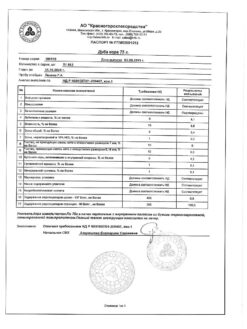
1 ml of the solution contains:
The active ingredient:
Octreotide acetate (in terms of octreotide) 0.050 mg, 0.100 mg and 0.300 mg
Auxiliary substances:
How to take, the dosage
How to take, the dosage
The drug Octreotide is recommended to be injected subcutaneously or intravenously.
Injections of the drug are recommended between meals or before bedtime.
In acromegaly, by injection, at an initial dose of 0.05 to 0.1 mg at 8 or 12-hour intervals. Further dose adjustments should be made on monthly blood GH concentrations (target concentration: GH <2.5 ng/ml; IGF-1 within normal values), analysis of clinical symptoms and tolerability of the drug. In most patients, the optimal daily dose is 0.2-0.3 mg p/k. The maximum dose of 1.5 mg/sug should not be exceeded.
In patients receiving octreotide at a stable dose, GH and IGF-1 concentrations should be determined every 6 months. If after 1 month of treatment with Octreotide there is insufficient decrease of GH and/or IGF-1 concentration and improvement of clinical symptoms of the disease, the therapy should be discontinued.
In endocrine tumors of the gastrointestinal tract and pancreas – p/c, in an initial dose of 0.05 mg 1-2 times per day.
Thereafter, depending on the therapeutic effect achieved, the effect on the concentration of hormones produced by the tumor (in the case of carcinoid tumors, the effect on renal excretion of 5-hydroxy-indoleacetic acid) and tolerability of the drug, the dose may be gradually increased to 0.2 mg p/c 3 times/day. In exceptional cases, higher doses may be required.
The maintenance dose of the drug should be adjusted individually. In carcinoid tumors, if therapy with octreotide at the maximum tolerated dose for 1 week has not been effective, treatment should not be continued.
In refractory diarrhea in AIDS patients, by p/c, in an initial dose of 0.1 mg 3 times/day. If after 1 week of therapy there is no clinical improvement, the dose is increased individually (in case of normal tolerance) up to 0.25 mg 3 times per day.
Dose adjustment is carried out taking into account stool dynamics and tolerability of the drug. If within 1 week of therapy with Octreotide (in dose of 0.25 mg 3 times per day) there is no improvement, therapy should be discontinued.
For prevention of complications after pancreatic surgery – the drug is administered by p/c in a dose of 0.1 mg 3 times/day for 7 days, starting from the day of surgery (the first dose of Octreotide is given at least 1 hour before surgery).
In case of bleeding from varices of the esophagus and stomach – by continuous IV infusion at a rate of 0.025 mg/h for 5 days.
The drug Octreotide should be diluted in 0.9% sodium chloride solution.
Patients with cirrhosis with bleeding from esophageal varices tolerate well therapy with the drug by continuous intravenous infusion at a dose of 0.05 mg/h for 5 days.
The use of octreotide in special clinical patient groups
In children and adolescents under 18 years of age
The experience with octreotide in children and adolescents under 18 years of age is limited.
In elderly patients (â¥65 years)
There is no need to adjust the dose of octreotide in elderly patients. In patients with impaired liver function
In patients with cirrhosis, the half-life of octreotide may be prolonged, and therefore adjustment of the maintenance dose in patients with impaired liver function is recommended.
In patients with impaired renal function
Octreotide dose adjustment is not necessary in patients with impaired renal function.
Recommendations for use
Subcutaneous administration
The physician or nurse should teach the patient the proper technique of the manipulation before giving Octreotide injections by themselves. In order to reduce pain at the injection site, the solution should be injected at room temperature.
The drug should not be injected in the same place at short intervals. Ampoules should be opened immediately prior to administration of the drug, the unused amount of the solution should be disposed of.
Injection
If it is necessary to administer Octreotide by injection, the contents of 1 ampoule containing 0.5 mg of Octreotide should be diluted in 60 ml of 0.9% sodium chloride solution, the solution obtained is administered using an infusion machine. The infusion is repeated with the required frequency in accordance with the recommended duration of therapy. It is also possible to administer the drug in lower concentrations by IV.
The drug can be diluted in 5% dextrose (glucose) solution in water. But it is preferable to use 0.9% sodium chloride solution because octreotide may affect glucose metabolism.
Before IV administration, the ampoule should be carefully inspected for damage, discoloration of the solution, presence of foreign particles and kept at room temperature.
The diluted solution should be used immediately after preparation to avoid microbial contamination. Unused residual solution should be disposed of.
Interaction
Interaction
It reduces absorption of cyclosporine, slows down absorption of cimetidine. It is necessary to correct the dosing regimen of concomitantly used diuretics, beta-adrenoblockers, BCC, oral hypoglycemic drugs, glucagon.
The combined use of octreotide and bromocriptine increases the bioavailability of bromocriptine.
Decreases the metabolism of substances metabolized with the participation of cytochrome P450 system enzymes (may be due to inhibition of growth hormone).
Because these effects of Octreotide cannot be excluded, caution should be exercised when prescribing drugs that are metabolized by the cytochrome P450 system and have a narrow range of therapeutic concentrations (e.g. quinidine, terfenadine).
Special Instructions
Special Instructions
In pituitary tumors secreting growth hormone, patients receiving octreotide should be closely monitored, as tumors may increase in size and develop serious complications such as narrowing of the visual fields. In these cases other treatment options should be considered.
Because a decrease in growth hormone levels and normalization of IGF-1 levels with octreotide therapy may lead to restoration of fertility in women with acromegaly, patients of childbearing age should use reliable contraception when using the drug.
When prescribing Octreotide for an extended period of time, thyroid function should be monitored.
If bradycardia develops with octreotide, doses of beta-adrenoblockers, BCCs or drugs affecting the water-electrolyte balance may be reduced if necessary.
In some patients octreotide may alter absorption of fats in the intestine.
With the use of Octreotide a decrease in cobalamin (vitamin B12) and deviations from normal values of cobalamin absorption test (Schilling test) have been observed. When using Octreotide in patients with a history of vitamin B12 deficiency it is recommended to monitor the cobalamin content in the body.
Management recommendations for patients during treatment with Octreotide regarding gallstone formation:
– Patients should have an initial gallbladder ultrasound before prescribing Octreotide;
– Repeated gallbladder ultrasounds should be performed during treatment with Octreotide, preferably at 6-12 month intervals;
If gallstones are detected before treatment begins, the potential benefits of Octreotide therapy should be evaluated against the possible risks associated with their presence. There is no evidence of any adverse effect of octreotide on the course or prognosis of pre-existing gallstone disease.
Management of patients in whom gallstones form during treatment with Octreotide:
– asymptomatic gallstones. Use of Octreotide can be discontinued or continued – according to a benefit/risk assessment. In either case, there is no need to do anything other than continue monitoring, making it more frequent if necessary;
– gallstones with clinical symptoms. The use of octreotide can be discontinued or continued – according to the benefit/risk assessment. In either case the patient should be treated as in other cases of gallstones with clinical manifestations. Medical treatment includes the use of combinations of bile acids (for example, chenodeoxycholic acid at a dose of 7.5 mg/kg/day in combination with ursodeoxycholic acid at the same dose) with ultrasound monitoring until the stones have completely disappeared.
In treatment of endocrine tumors of the gastrointestinal tract and pancreas with Octreotide in rare cases a sudden relapse of the disease symptoms may occur. In patients with insulinomas during treatment with Octreotide an increase in the severity and duration of hypoglycemia may be observed (this is due to a more pronounced suppressive effect on growth hormone and glucagon secretion than on insulin secretion, as well as a shorter duration of inhibitory effect on insulin secretion).
These patients should be closely monitored regularly, both at the start of treatment with Octreotide and with each change in dose.
Significant fluctuations in blood glucose concentrations may be attempted to be reduced by administering Octreotide more frequently at lower doses. In patients with type 1 diabetes, octreotide may reduce the need for insulin. In nondiabetic and type 2 diabetic patients with partially preserved insulin secretion, administration of octreotide may result in postprandial hyperglycemia.
When using Octreotide in patients with diabetes mellitus, monitoring of blood glucose concentrations and antidiabetic therapy are recommended.
Because there is an increased risk of developing type 1 diabetes after bleeding from esophageal and gastric varices, and patients with diabetes may also have changes in insulin requirements, systematic monitoring of blood glucose concentrations is necessary in these cases.
The dosing regimen of concomitantly used diuretics, beta-adrenoblockers, BKK, insulin, oral hypoglycemic agents, and glucagon must be corrected.
The effect on the ability to drive vehicles and operate machinery. Some side effects of octreotide may adversely affect the ability to operate motor vehicles and other mechanisms requiring increased concentration, accuracy and speed of psychomotor reactions.
In this regard, it is recommended that caution be exercised when driving vehicles or operating machinery requiring increased concentration if appropriate symptoms occur.
Contraindications
Contraindications
Side effects
Side effects
The digestive system: very often – diarrhea, abdominal pain, nausea, constipation, bloating; often – dyspeptic disorders, vomiting, feeling of a full/heavy stomach, steatorrhea, soft stool consistency, changes in stool color, anorexia.
Nervous system disorders: very often – headache; often – dizziness.
Endocrine system: very common – hyperglycemia; common – hypothyroidism/disorders of thyroid function (decreased levels of TSH, total and free thyroxine); hypoglycemia, impaired glucose tolerance.
Hepatobiliary system disorders: very common – cholelithiasis, i.e., gallstones formation; common – cholecystitis, disorders of colloidal stability of bile (formation of cholesterol microcrystals), hyperbilirubinemia, increased activity of liver transaminases.
Dermatological reactions: often – itching, rash, hair loss.
Respiratory system: often – shortness of breath.
System: often – bradycardia; infrequent – tachycardia.
General disorders and reactions at the injection site: very often – pain at the injection site; infrequently – dehydration.
The following adverse events have been noted in clinical practice during therapy with Octreotide regardless of any causal relationship to the use of the drug.
Immune system disorders: anaphylactic reactions, allergic reactions/hypersensitivity.
Dermatological reactions: urticaria.
Hepatobiliary system disorders: acute pancreatitis, acute hepatitis without signs of cholestasis, cholestatic hepatitis, cholestasis, jaundice, cholestatic jaundice, increased levels of ALP, GGT.
Systemic reactions: arrhythmia.
Overdose
Overdose
The administration of octreotide in a dose of up to 2000 mcg as a p/k injection 3 times over several months is known to be well tolerated. The maximum single dose when administered by intravenous bolus in an adult patient was 1000 mcg.
Symptoms such as decreased heart rate, “rushes” of blood to the face, abdominal pain of a spastic nature, diarrhea, nausea, and a feeling of emptiness in the stomach were noted.
All of these symptoms resolved within 24 hours of administration. One patient was inadvertently administered an excessive dose of octreotide of 250 mcg/h (instead of 25 mcg/h) by prolonged infusion, with no side effects. No life-threatening reactions were noted in acute overdose.
Treatment: symptomatic therapy.
Pregnancy use
Pregnancy use
Pregnancy
There are limited data (less than 300 pregnancy outcomes) on the use of Octreotide in pregnant women and approximately one-third of pregnancy outcomes are unknown.
More than 50% of the cases in which women received octreotide during pregnancy were reported in patients with acromegaly. Most women received octreotide in the first trimester of pregnancy as a p/c injection of octreotide at a dose of 100-1200 mcg/day or with an intravenous injection of octreotide suspension at a dose of 10-40 mg/month. Congenital malformations have been reported in approximately 4% of pregnancies with known outcomes.
In these cases, there is no causal relationship between these phenomena and octreotide. Animal studies have shown no toxic effects of octreotide on reproduction, with the exception of temporary fetal growth retardation.
The drug Octreotide should be used during pregnancy only for absolute indications. Women of preserved reproductive potential should use reliable contraception.
Breastfeeding period
It is not known whether Octreotide penetrates into human breast milk.
An animal study found that octreotide penetrates the milk of lactating rats.
Breastfeeding should be avoided during therapy with Octreotide.
Similarities
Similarities
Additional information
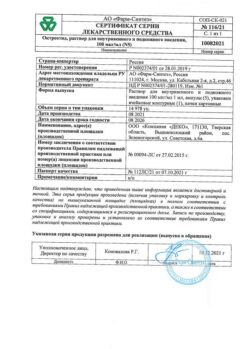
| Shelf life | 3 years. Do not use after the expiration date stated on the package. |
|---|---|
| Conditions of storage | Store in a light-protected place at 2 to 8 ° C. Do not freeze. Store out of the reach of children. |
| Manufacturer | Pharmstandard-Leksredstva, Russia |
| Medication form | solution |
| Brand | Pharmstandard-Leksredstva |
Other forms…
Related products
Buy Octreotide,. 50 µg/ml 1 ml 10 pcs with delivery to USA, UK, Europe and over 120 other countries.