No products in the cart.
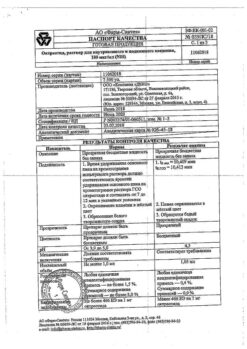
Octreotide, 100 µg/ml 1 ml 5 pcs
€18.35 €15.29
Description
Octreotide is a synthetic analog of somatostatin, which is a derivative of the natural hormone somatostatin and has similar pharmacological effects to it, but a much longer duration of action.
Octreotide suppresses growth hormone secretion, both pathologically increased and caused by arginine, physical exercise and insulin hypoglycemia. The drug also suppresses insulin, glucagon, gastrin, and serotonin secretion, both pathologically elevated and induced by food intake; it also suppresses arginine-stimulated insulin and glucagon secretion. Octreotide suppresses thyrotropin secretion induced by thyreoliberin. Unlike somatostatin, octreotide suppresses growth hormone secretion to a greater extent than insulin secretion, and its administration is not accompanied by subsequent hormone hypersecretion (such as growth hormone in acromegaly patients).
In patients with acromegaly, octreotide reduces plasma concentrations of growth hormone and insulin-like growth factor (IGF-1). Decrease of growth hormone concentration by 50% or more is noted in 90% of patients, and the value of growth hormone concentration of not less than 5 ng/ml is reached in about half of patients. In most patients with acromegaly, octreotide reduces the severity of headache, soft tissue swelling, hyperhidrosis, joint pain and paresthesias. In patients with large pituitary adenomas, treatment with Octreotide may lead to some reduction in tumor size.
In secreting tumors of the gastroenteropancreatic endocrine system in cases of ineffective therapy (surgery, hepatic artery embolization, chemotherapy including streptozotocin and fluorouracil) administration of Octreotide may lead to improvement of the disease course.
For example, in carcinoid tumors, administration of Octreotide may lead to reduction of the severity of blood flushes to the face, diarrhea, which in many cases is accompanied by reduction of serotonin concentration in plasma and renal excretion of 5-hydroxyindoleacetic acid. In tumors characterized by hyperproduction of vasoactive intestinal peptide (VIPOM), use of octreotide leads in most patients to reduction of severe secretory diarrhea and, accordingly, improvement of patient’s quality of life.
At the same time there is a reduction of concomitant electrolyte imbalances, such as hypokalemia, which allows to cancel enteral and parenteral administration of fluids and electrolytes. In some patients the progression of the tumor is slowed or stopped, its size is reduced, as well as the size of liver metastases. Clinical improvement is usually accompanied by a decrease in plasma concentration of vasoactive intestinal peptide (VIP) or its normalization.
In glucagonomas, use of Octreotide results in a reduction of erythema migrans. Octreotide has no significant effect on the severity of hyperglycemia in diabetes mellitus, and the need for insulin or oral hypoglycemic agents usually remains unchanged. The drug causes reduction of diarrhea, which is accompanied by an increase in body weight.
While decrease in plasma glucagon concentration under the influence of Octreotide is transient, the clinical improvement remains stable during the whole period of using the drug. In patients with gastrinomas/Zollinger-Ellison syndrome when using Octreotide as monotherapy or in combination with proton pump inhibitors or H2-histamine receptor blockers it is possible to decrease hypersecretion of hydrochloric acid in the stomach, decrease gastrin concentration in blood plasma and decrease the severity of diarrhea and flushes.
In patients with insulinomas octreotide decreases the level of immunoreactive insulin in blood (this effect may be transient, about 2 hours). In patients with operable tumors Octreotide can provide restoration and maintenance of normoglycemia in the preoperative period. In patients with inoperable benign and malignant tumors, glycemic control may improve without a simultaneous prolonged decrease in blood insulin levels.
In patients with rare tumors hyperproducing the growth hormone releasing factor (somatoliberinomas), octreotide reduces the severity of acromegaly symptoms. This is due to the suppression of growth hormone releasing factor and growth hormone secretion itself. Subsequently, hypertrophy of the pituitary gland may decrease.
In bleeding from esophageal and gastric varices in cirrhotic patients, the use of octreotide in combination with specific treatments (e.g., sclerosing therapy) leads to more effective bleeding arrest and early rebleeding, reduced transfusion volume and improved 5-day survival. The mechanism of action of octreotide is thought to be related to reduction of organ blood flow through suppression of vasoactive hormones such as VIP and glucagon.
Pharmacokinetics
Absorption
After oral administration, octreotide is rapidly and completely absorbed. Tmax of Octreotide in plasma is within 30 min.
Distribution
The binding to plasma proteins is 65%. The binding of octreotide with blood cells is extremely insignificant. Vd is 0.27 l/kg.
The T1/2 after p/c administration of Octreotide is 100 min. After IV administration, excretion of Octreotide occurs in 2 phases, with a T1/2 of 10 and 90 min, respectively. Most of octreotide is excreted through the intestine, about 32% is excreted unchanged by the kidneys. Total clearance is 160 ml/min.
Indications
Indications
prevention and treatment of complications after operations on the pancreas and gastroduodenal zone;
stopping bleeding and preventing re-bleeding from esophageal varices in patients with liver cirrhosis (as part of complex therapy);
treatment of acute pancreatitis;
stopping bleeding in gastric and duodenal ulcers.
Pharmacological effect
Pharmacological effect
Octreotide is a synthetic analogue of somatostatin, which is a derivative of the natural hormone somatostatin and has pharmacological effects similar to it, but a significantly longer duration of action.
Octreotide suppresses the secretion of growth hormone, both pathologically increased and caused by arginine, exercise and insulin hypoglycemia. The drug also suppresses the secretion of insulin, glucagon, gastrin, serotonin, both pathologically increased and caused by food intake; also suppresses the secretion of insulin and glucagon stimulated by arginine. Octreotide suppresses the secretion of thyrotropin caused by thyrotropin-releasing hormone. Unlike somatostatin, octreotide suppresses growth hormone secretion to a greater extent than insulin secretion, and its administration is not accompanied by subsequent hypersecretion of hormones (for example, growth hormone in patients with acromegaly).
In patients with acromegaly, octreotide reduces the concentration of growth hormone and insulin-like growth factor (IGF-1) in the blood plasma. A decrease in the concentration of growth hormone by 50% or more is observed in 90% of patients, while a growth hormone concentration of at least 5 ng/ml is achieved in approximately half of the patients. In most patients with acromegaly, octreotide reduces the severity of headache, soft tissue swelling, hyperhidrosis, joint pain and paresthesia. In patients with large pituitary adenomas, treatment with octreotide may lead to some reduction in tumor size.
For secreting tumors of the gastroenteropancreatic endocrine system, in cases of insufficient effectiveness of the therapy (surgery, embolization of the hepatic artery, chemotherapy, including streptozotocin and fluorouracil), the administration of octreotide can lead to an improvement in the course of the disease.
Thus, in carcinoid tumors, the use of octreotide can lead to a decrease in the severity of the sensation of flushing and diarrhea, which in many cases is accompanied by a decrease in the concentration of serotonin in plasma and the excretion of 5-hydroxyindoleacetic acid by the kidneys. For tumors characterized by overproduction of vasoactive intestinal peptide (VIP), the use of octreotide in most patients leads to a reduction in severe secretory diarrhea and, accordingly, an improvement in the patient’s quality of life.
At the same time, there is a decrease in concomitant electrolyte imbalances, such as hypokalemia, which makes it possible to cancel enteral and parenteral administration of fluids and electrolytes. In some patients, tumor progression slows down or stops, its size decreases, as does the size of liver metastases. Clinical improvement is usually accompanied by a decrease in the plasma concentration of vasoactive intestinal peptide (VIP) or its normalization.
For glucagonomas, the use of octreotide leads to a decrease in erythema migrans. Octreotide does not have any significant effect on the severity of hyperglycemia in diabetes mellitus, while the need for insulin or oral hypoglycemic drugs usually remains unchanged. The drug causes a decrease in diarrhea, which is accompanied by an increase in body weight.
Although the decrease in plasma glucagon concentration under the influence of octreotide is transient, clinical improvement remains stable throughout the period of drug use. In patients with gastrinomas/Zollinger-Ellison syndrome, when using octreotide as monotherapy or in combination with proton pump inhibitors or H2-histamine receptor blockers, it is possible to reduce the hypersecretion of hydrochloric acid in the stomach, reduce the concentration of gastrin in the blood plasma, as well as reduce the severity of diarrhea and hot flashes.
In patients with insulinomas, octreotide reduces the level of immunoreactive insulin in the blood (this effect can be short-term – about 2 hours). In patients with operable tumors, octreotide can restore and maintain normoglycemia in the preoperative period. In patients with inoperable benign and malignant tumors, glycemic control may improve without a simultaneous prolonged decrease in blood insulin levels.
In patients with rare tumors that overproduce growth hormone releasing factor (somatoliberinomas), octreotide reduces the severity of symptoms of acromegaly. This is due to the suppression of the secretion of growth hormone releasing factor and growth hormone itself. In the future, pituitary hypertrophy may decrease.
For bleeding from varices of the esophagus and stomach in patients with liver cirrhosis, the use of octreotide in combination with specific treatment (for example, sclerotherapy) leads to more effective stoppage of bleeding and early rebleeding, a reduction in the volume of transfusions and an improvement in 5-day survival. The mechanism of action of octreotide is believed to be associated with a decrease in organ blood flow through the suppression of vasoactive hormones such as VIP and glucagon.
Pharmacokinetics
Suction
After subcutaneous administration, octreotide is rapidly and completely absorbed. Tmax of octreotide in plasma is within 30 minutes.
Distribution
The connection with blood plasma proteins is 65%. The binding of octreotide to blood cells is extremely insignificant. Vd is 0.27 l/kg.
Removal
T1/2 after subcutaneous administration of octreotide is 100 minutes. After intravenous administration, octreotide is eliminated in 2 phases, with T1/2 – 10 and 90 minutes, respectively. Most of octreotide is excreted through the intestines, about 32% is excreted unchanged by the kidneys. The total clearance is 160 ml/min.
Special instructions
Special instructions
For pituitary tumors that secrete growth hormone, careful monitoring of patients receiving octreotide is necessary, because it is possible that the size of the tumors may increase with the development of such a serious complication as a narrowing of the visual fields. In these cases, the need for other treatment methods should be considered.
Since a decrease in growth hormone levels and normalization of IGF-1 levels during octreotide therapy can lead to restoration of fertility in women with acromegaly, patients of childbearing age should use reliable methods of contraception when using the drug.
When prescribing octreotide for a long period of time, it is necessary to monitor thyroid function.
If bradycardia develops during the use of octreotide, if necessary, it is possible to reduce the dose of beta-blockers, CCBs or drugs that affect water-electrolyte balance.
In some patients, octreotide may alter the absorption of fats in the intestine.
During the use of octreotide, there was a decrease in the content of cobalamin (vitamin B12) and deviations from the norm in the cobalamin absorption test (Schilling test). When using octreotide in patients with a history of vitamin B12 deficiency, it is recommended to monitor cobalamin levels in the body.
Recommendations for the management of patients during treatment with Octreotide regarding the formation of gallstones:
– before prescribing octreotide, patients should undergo an initial ultrasound of the gallbladder;
– during treatment with Octreotide, repeated ultrasounds of the gallbladder should be performed, preferably at intervals of 6–12 months;
– If gallstones are detected before the start of treatment, it is necessary to evaluate the potential benefits of octreotide therapy compared to the possible risks associated with their presence. There is no data on any negative effect of octreotide on the course or prognosis of existing gallstone disease.
Management of patients in whom gallstones form during treatment with Octreotide:
– asymptomatic gallstones. The use of octreotide can be stopped or continued according to the benefit/risk assessment. In any case, there is no need to do anything other than continue monitoring, making it more frequent if necessary;
– gallstones with clinical symptoms. The use of octreotide can be stopped or continued according to the benefit/risk assessment. In any case, the patient should be treated in the same way as in other cases of cholelithiasis with clinical manifestations. Drug treatment includes the use of combinations of bile acid preparations (for example, chenodeoxycholic acid at a dose of 7.5 mg/kg/day in combination with ursodeoxycholic acid at the same dose) under ultrasound control until the stones completely disappear.
When treating endocrine tumors of the gastrointestinal tract and pancreas with octreotide, in rare cases a sudden relapse of symptoms of the disease may occur. In patients with insulinomas, during treatment with octreotide, an increase in the severity and duration of hypoglycemia may be observed (this is due to a more pronounced suppressive effect on the secretion of growth hormone and glucagon than on insulin secretion, as well as a shorter duration of the inhibitory effect on insulin secretion). Careful regular monitoring of these patients should be ensured both at the beginning of treatment with Octreotide and whenever the dose of the drug is changed.
Significant fluctuations in blood glucose concentrations can be reduced by administering octreotide more frequently and in smaller doses. In patients with type 1 diabetes mellitus, octreotide may reduce the need for insulin. In patients without diabetes and with type 2 diabetes with partially preserved insulin secretion, administration of octreotide may lead to postprandial hyperglycemia. When using octreotide in patients with diabetes mellitus, monitoring of blood glucose concentrations and antidiabetic therapy is recommended.
Since after bleeding from varicose veins of the esophagus and stomach, the risk of developing type 1 diabetes mellitus is increased, and in patients with diabetes mellitus, changes in insulin requirements are also possible, in these cases systematic monitoring of blood glucose concentrations is necessary.
It is necessary to adjust the dosage regimen of simultaneously used diuretics, beta-blockers, CCBs, insulin, oral hypoglycemic agents, and glucagon.
Impact on the ability to drive vehicles and operate machinery. Some side effects of octreotide may negatively affect the ability to drive vehicles and other mechanisms that require increased concentration, accuracy and speed of psychomotor reactions. In this regard, it is recommended that when the corresponding symptoms appear, caution is exercised when driving vehicles or machinery that require increased concentration.
Active ingredient
Active ingredient
Octreotide
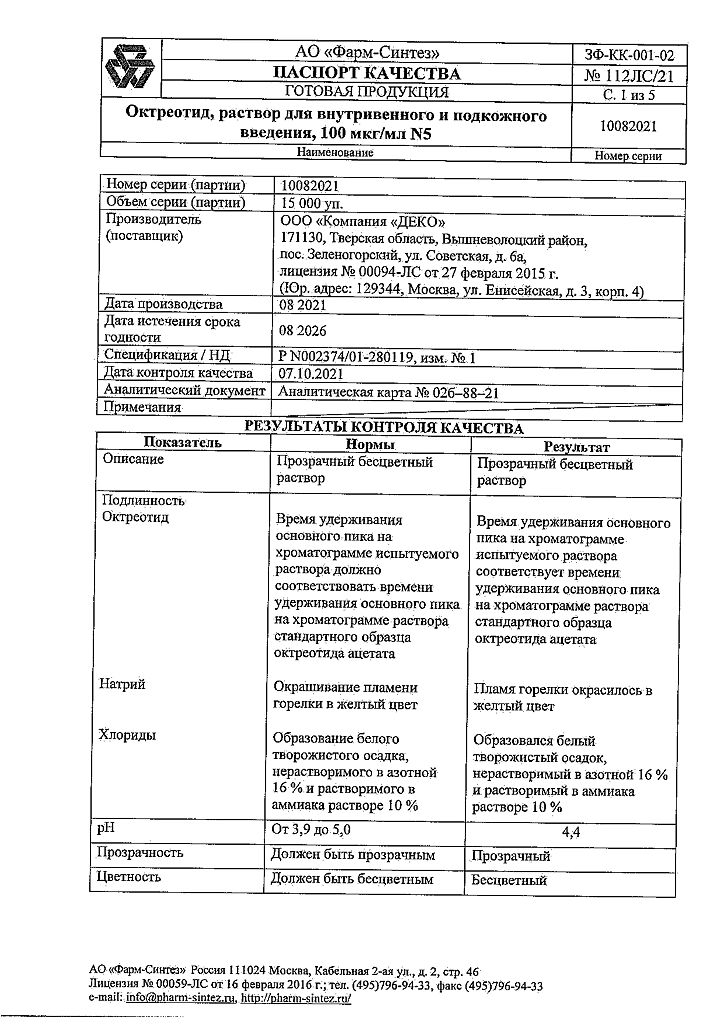
Composition
Composition
Active ingredient:
octreotide acetate;
Excipients:
sodium chloride;
water for injections
Contraindications
Contraindications
Hypersensitivity to octreotide or other components of the drug; children under 18 years of age.
With caution: cholelithiasis (cholelithiasis); diabetes mellitus
Side Effects
Side Effects
From the digestive system: very often – diarrhea, abdominal pain, nausea, constipation, bloating; often – dyspeptic disorders, vomiting, feeling of fullness/heaviness in the abdomen, steatorrhea, soft stool consistency, change in stool color, anorexia.
From the nervous system: very often – headache; often – dizziness.
From the endocrine system: very often – hyperglycemia; often – hypothyroidism/thyroid dysfunction (decreased levels of TSH, total and free thyroxine); hypoglycemia, impaired glucose tolerance.
From the hepatobiliary system: very often – cholelithiasis, i.e. formation of gallstones; often – cholecystitis, impaired colloidal stability of bile (formation of cholesterol microcrystals), hyperbilirubinemia, increased activity of liver transaminases.
Dermatological reactions: often – itching, rash, hair loss.
From the respiratory system: often – shortness of breath.
From the cardiovascular system: often – bradycardia; infrequently – tachycardia.
General disorders and reactions at the injection site: very often – pain at the injection site; infrequently – dehydration.
During therapy with octreotide, the following adverse events were observed in clinical practice, regardless of the presence of a cause-and-effect relationship with the use of the drug.
From the immune system: anaphylactic reactions, allergic reactions/hypersensitivity.
Dermatological reactions: urticaria.
From the hepatobiliary system: acute pancreatitis, acute hepatitis without cholestasis, cholestatic hepatitis, cholestasis, jaundice, cholestatic jaundice, increased levels of alkaline phosphatase, GGT.
From the cardiovascular system: arrhythmias.
Interaction
Interaction
Reduces the absorption of cyclosporine, slows down the absorption of cimetidine. It is necessary to adjust the dosage regimen of simultaneously used diuretics, beta-blockers, CCBs, oral hypoglycemic drugs, and glucagon.
The combined use of octreotide and bromocriptine increases the bioavailability of bromocriptine.
Reduces the metabolism of substances metabolized with the participation of enzymes of the cytochrome P450 system (may be due to suppression of growth hormone).
Since similar effects of octreotide cannot be excluded, caution should be exercised when prescribing drugs that are metabolized by the cytochrome P450 system and have a narrow range of therapeutic concentrations (for example, quinidine, terfenadine).
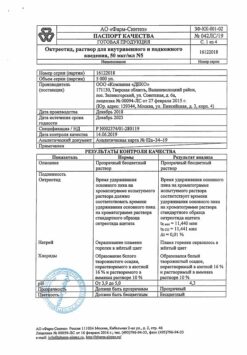
Storage conditions
Storage conditions
In a dry place, protected from light, at a temperature of 8 to 25 °C.
Shelf life
Shelf life
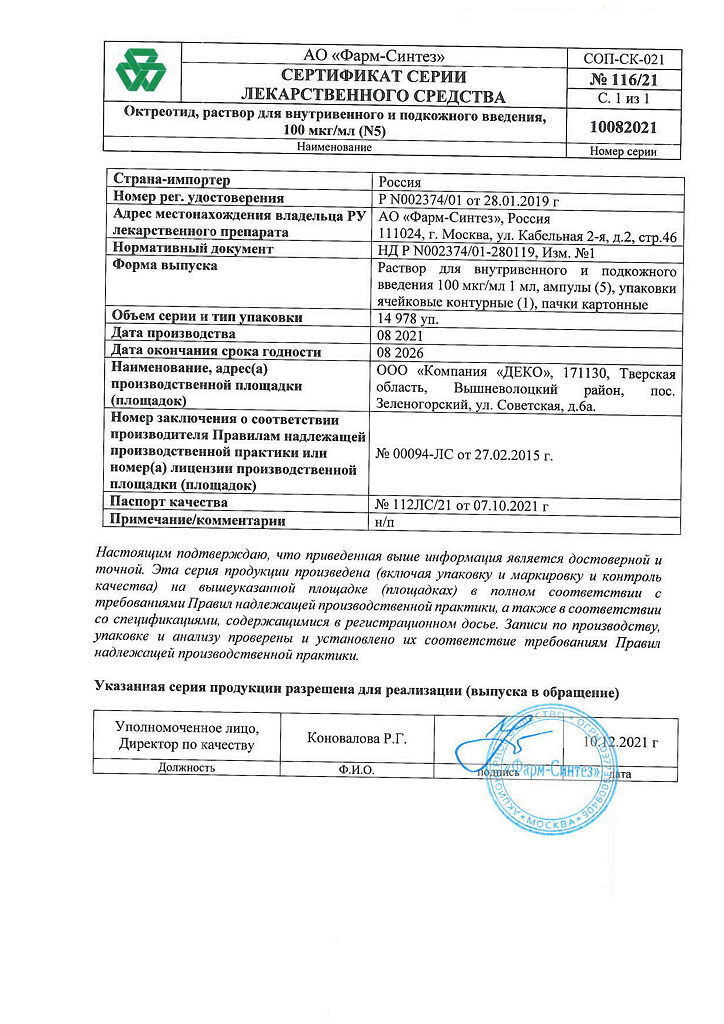
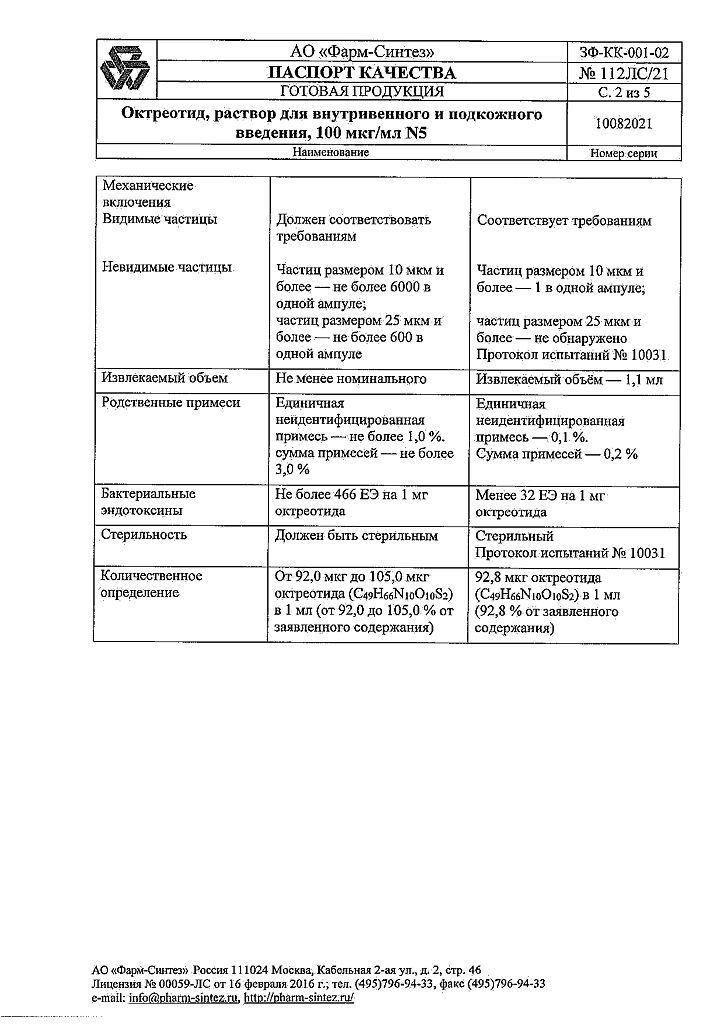
5 years
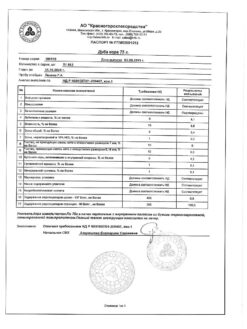
Manufacturer
Manufacturer
Pharm-Sintez, Russia
Additional information
| Shelf life | 5 years |
|---|---|
| Conditions of storage | In a dry, light-protected place at a temperature of 8 to 25 °C. |
| Manufacturer | Pharm-Sintez, Russia |
| Medication form | solution |
| Brand | Pharm-Sintez |
Other forms…
Related products
Buy Octreotide, 100 µg/ml 1 ml 5 pcs with delivery to USA, UK, Europe and over 120 other countries.