No products in the cart.
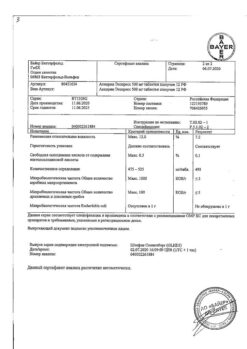
Nurofen for children, 100 mg/5 ml suspension 200 ml strawberry
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group:
Non-steroidal anti-inflammatory drug (NSAID).
ATC code: M01AE01
Pharmacological properties
Pharmacodynamics:
The mechanism of action of ibuprofen, a propionic acid derivative from the group of nonsteroidal anti-inflammatory drugs (NSAIDs), is due to inhibiting the synthesis of prostaglandins, mediators of pain, inflammation and hyperthermia. It indiscriminately blocks cyclooxygenase 1 (COX-1) and cyclooxygenase 2 (COX-2), and therefore inhibits the synthesis of prostaglandins. In addition, ibuprofen reversibly inhibits platelet aggregation. It has analgesic, antipyretic and anti-inflammatory effects. The analgesic effect is most pronounced for pain of inflammatory nature. The action of the drug lasts up to 8 hours.
Pharmacokinetics:
Absorption is high and is quickly and almost completely absorbed from the gastrointestinal tract (GIT) (binding to plasma proteins – 90%). After taking the drug on an empty stomach in adults ibuprofen is detected in blood plasma after 15 minutes, the maximum concentration (Cmax) of ibuprofen in plasma is reached after 60 minutes. Taking the drug with food can increase the time to reach maximum concentration (TCmax) up to 1-2 hours. The half-life (T1/2) is 2 hours. Slowly penetrates into the joint cavity, stays in synovial fluid, creating higher concentrations in it than in blood plasma. After absorption, about 60% of the pharmacologically inactive R-form is slowly transformed into the active S-form. It is metabolized in the liver. It is excreted by kidneys (not more than 1% unchanged) and, to a lesser extent, in bile.
In limited studies ibuprofen was found in very low concentrations in breast milk.
Indications
Indications
– acute respiratory diseases;
– influenza;
– childhood infections;
– other infectious and inflammatory diseases and post-vaccination reactions.
As an analgesic in pain syndrome of mild to moderate intensity, including:
– toothache;
– headache;
– migraine;
– neuralgia;
– ear pain;
– sore throat;
– pain from sprains;
– muscle pain;
– rheumatic pain;
– joint pain.
The drug is intended as symptomatic therapy, reducing pain and inflammation at the time of use; it has no effect on the progression of the disease.
Active ingredient
Active ingredient
Composition
Composition
How to take, the dosage
How to take, the dosage
Interaction
Interaction
The concomitant use of ibuprofen with the medicinal products listed below should be avoided.
Acetylsalicylic acid: except for acetylsalicylic acid in low doses (not more than 75 mg/day) prescribed by a physician, because co-administration may increase the risk of side effects. When concomitant use, ibuprofen reduces anti-inflammatory and antiplatelet effects of acetylsalicylic acid (increased incidence of acute coronary failure is possible in patients receiving low-dose acetylsalicylic acid as an antiplatelet agent, after starting ibuprofen administration).
Other NSAIDs, including selective COX-2 inhibitors: Concomitant use of two or more drugs from the NSAID group should be avoided because of possible increased risk of side effects.
Cautiously use concomitantly with the following drugs.
Anticoagulants and thrombolytics: NSAIDs may increase the effect of anticoagulants, particularly warfarin and thrombolytics.
Antihypertensive drugs (ACE inhibitors and angiotensin II receptor antagonists) and diuretics: NSAIDs may decrease the effectiveness of drugs in these groups. Diuretics and ACE inhibitors may increase nephrotoxicity of NSAIDs.
GCS: increased risk of GI ulcers and gastrointestinal bleeding.
Antiaggregants and selective serotonin reuptake inhibitors: increased risk of gastrointestinal bleeding.
Heart glycosides: Simultaneous administration of NSAIDs and cardiac glycosides may worsen heart failure, decrease glomerular filtration rate, and increase plasma concentrations of cardiac glycosides.
Lithium drugs: There is data on the likelihood of increased plasma lithium concentrations with NSAIDs.
Methotrexate: There is data on the likelihood of increased plasma concentrations of methotrexate with NSAIDs.
Cyclosporine: increased risk of nephrotoxicity with concomitant administration of NSAIDs and cyclosporine.
Mifepristone: NSAIDs should not be started earlier than 8-12 days after mifepristone administration because NSAIDs may reduce the effectiveness of mifepristone.
Tacrolimus: Simultaneous use of NSAIDs and tacrolimus may increase the risk of nephrotoxicity.
Zidovudine: Concomitant use of NSAIDs and zidovudine may increase hematotoxicity. There is evidence of an increased risk of hemarthrosis and hematomas in HIV-positive patients with hemophilia who have received concomitant treatment with zidovudine and ibuprofen.
Quinolone antibiotics: patients co-treated with NSAIDs and quinolone antibiotics may have an increased risk of seizures.
Special Instructions
Special Instructions
It is recommended that the drug be taken for as short a course as possible and at the lowest effective dose necessary to relieve symptoms.
During long-term treatment, monitoring of peripheral blood count and functional status of the liver and kidneys is necessary. In case of gastropathy symptoms occurrence a thorough control is indicated, including esophagogastroduodenoscopy, general blood test (hemoglobin determination), fecal occult blood test. If it is necessary to determine 17-ketosteroids, the drug should be cancelled 48 hours before the study. Ethanol intake is not recommended during the treatment period. The drug is contraindicated in patients with fructose intolerance because it contains maltitol.
Nurofen® for children can be used in children with diabetes because the drug does not contain sugar. It does not contain dyes.
Patients with renal insufficiency should consult their physician before using the drug, because there is a risk of impairment of renal function.
Patients with hypertension, including a history of hypertension and/or chronic heart failure, should consult a physician before using the drug, as the drug may cause fluid retention, increased blood pressure, and edema.
The use of NSAIDs in patients with chickenpox may be associated with an increased risk of severe suppurative complications of infectious and inflammatory skin and subcutaneous fat diseases (e.g., necrotizing fasciitis). In this regard, it is recommended to avoid using the drug in case of chicken pox.
Influence on driving and other potentially dangerous machinery
Patients who have dizziness, drowsiness, lethargy or visual disturbances while taking ibuprofen should avoid driving or operating machinery.
Contraindications
Contraindications
Side effects
Side effects
The risk of side effects can be minimized by taking the drug in a short course, at the lowest effective dose necessary to relieve symptoms.
The side effects are mostly dose-dependent. The following adverse reactions have been reported with short-term administration of ibuprofen in doses not exceeding 1200 mg/day. When treating chronic conditions and with long-term use, other adverse reactions may occur.
The incidence of adverse reactions has been evaluated on the basis of the following criteria: Very frequent (⥠1/10), Frequent (⥠1/100 to < 1/10), Infrequent (⥠1/1000 to < 1/100), Rare (⥠1/10 000 to < 1/1000), Very rare (< 1/10 000), Frequency unknown (no frequency assessment data available).
Disorders of the blood and lymphatic system
– Very rare: disorders of hematopoiesis (anemia, leukopenia, aplastic anemia, hemolytic anemia, thrombocytopenia, pancytopenia, agranulocytosis). The first symptoms of these disorders are fever, sore throat, superficial mouth ulcers,
flu-like symptoms, marked weakness, nosebleeds and subcutaneous hemorrhages, bleeding and bruising of unknown etiology.
Immune system disorders
– Infrequent: hypersensitivity reactions – non-specific allergic reactions and anaphylactic reactions, respiratory reactions (bronchial asthma, including its exacerbation, bronchospasm, dyspnea), skin reactions (itching, urticaria, purpura, Quincke’s edema, exfoliative and bullous dermatoses, including toxic epidermal necrolysis, Lyell syndrome, Stevens-Johnson syndrome, erythema multiforme), allergic rhinitis, eosinophilia.
– Very rare: severe hypersensitivity reactions, including swelling of the face, tongue and throat, shortness of breath, tachycardia, arterial hypotension (anaphylaxis, Quincke’s edema or severe anaphylactic shock).
Gastrointestinal disorders
– Infrequent: abdominal pain, nausea, dyspepsia.
– Rare: diarrhea, flatulence, constipation, vomiting.
– Very rare: peptic ulcer, perforation or gastrointestinal bleeding, melena, bloody vomiting, ulcerative stomatitis, gastritis.
– Frequency unknown: exacerbation of ulcerative colitis and Crohn’s disease.
Liver and biliary tract disorders
– Very rare: disorders of liver function.
Rare renal and urinary tract disorders
– Very rare: acute renal failure (compensated and decompensated), especially with long-term use, in
combined with increased plasma urea concentration and edema, papillary necrosis.
Nervous system disorders
– Infrequent: headache.
– Very rare: aseptic meningitis (in patients with autoimmune diseases).
Cardiovascular disorders
– Frequency unknown: heart failure, peripheral edema, with prolonged use, increased risk of thrombotic complications (e.g., myocardial infarction, stroke), increased blood pressure.
Respiratory and mediastinal disorders
– Frequency unknown: bronchial asthma, bronchospasm, dyspnea.
Other
– Very rare: edema, including peripheral edema.
Laboratory parameters
– Hematocrit or hemoglobin (may decrease)
– Bleeding time (may increase)
/p>
– plasma glucose concentration (may decrease)
– creatinine clearance (may decrease)
/p>
– plasma creatinine concentration (may increase)
– “hepatic” transaminase activity (may increase)
If side effects occur, discontinue the drug and seek medical attention.
Overdose
Overdose
In children, overdose symptoms may occur after a dose greater than 400 mg/kg body weight. In adults, the dose-dependent effect of overdose is less pronounced. T1/2 of the drug in overdose is 1.5-3 hours.
Symptoms: nausea, vomiting, epigastric pain or, less frequently, diarrhea, tinnitus, headache and gastrointestinal bleeding. In more severe cases, CNS manifestations are observed: drowsiness, rarely – agitation, convulsions, disorientation, coma. In cases of severe poisoning metabolic acidosis and increased prothrombin time, renal failure, liver tissue damage, decreased BP, respiratory depression and cyanosis may develop. In patients with bronchial asthma, exacerbation of this disease is possible.
The treatment: symptomatic, with mandatory provision of airway patency, ECG monitoring and basic vital signs until the patient’s condition normalizes. Oral administration of activated charcoal or gastric lavage within 1 hour after taking a potentially toxic dose of ibuprofen is recommended. If ibuprofen has already been absorbed, alkaline drinking may be prescribed in order to eliminate the acidic derivative of ibuprofen by the kidneys, forced diuresis. Frequent or prolonged seizures should be stopped by IV administration of diazepam or lorazepam. If bronchial asthma worsens, the use of bronchodilators is recommended.
Similarities
Similarities
Additional information
| Weight | 0.280 kg |
|---|---|
| Shelf life | 3 years. Between 6 months after opening the bottle, do not use. Do not use if the product has expired. |
| Conditions of storage | At a temperature not exceeding + 25°C, out of the reach of children! In a dry place. |
| Manufacturer | Reckitt Benckiser Healthcare India Private Limited, India |
| Medication form | oral suspension |
| Brand | Reckitt Benckiser Healthcare India Private Limited |
Related products
Buy Nurofen for children, 100 mg/5 ml suspension 200 ml strawberry with delivery to USA, UK, Europe and over 120 other countries.