No products in the cart.
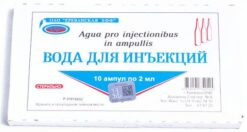
Novocaine, 0.5%, 5 ml, 10 pcs.
€1.00
Out of stock
(E-mail when Stock is available)
EAN: 4602509005638
SKU: 45250
Categories: Anesthesia and resuscitation, Anesthesia solutions, Medicine
Description
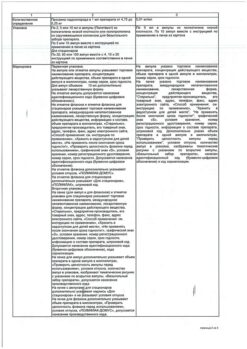
Novocaine is a local anesthetic. Disrupts generation and conduction of nerve impulses mainly in non-myelinated fibers. Being a weak base, it interacts with the receptors of membrane sodium channels, blocks the flow of sodium ions, displaces calcium from the receptors located on the inner surface of the membrane. When absorbed or injected directly into the blood, it reduces acetylcholine formation and excitability of choline reactive systems, has a ganglion-blocking effect, reduces smooth muscle spasm, inhibits myocardial and motor cortical excitability. It changes the action potential in the membranes of nerve cells without a pronounced effect on the resting potential. Antiarrhythmic action is associated with an increase in the effective refractory period, reducing myocardial excitability and automaticity. It is effective (when administered v/m) in elderly patients in the early stages of diseases associated with functional disorders of the CNS (hypertension, spasms of coronary vessels and brain vessels, etc.). It has analgesic and antishock activity, hypotensive and antiarrhythmic action. It removes descending inhibitory effects of reticular formation of the brain stem. Inhibits polysynaptic reflexes. In high doses may cause convulsions. It has short anesthetic activity (duration of infiltration anesthesia is 0.5-1 hours). It is used in combination with vasoconstrictors (adrenaline) to reduce systemic action, toxicity and prolong the effect. With increasing concentration of the solutions it is recommended to reduce the total dose.
Indications
Indications
Pain syndrome in gastric and duodenal ulcers, infiltration, conduction, epidural and spinal anesthesia; vagosympathetic and paranephral blockade; nausea; hemorrhoids.
Active ingredient
Active ingredient
Composition
Composition
Active substances: procaine hydrochloride 5 mg
How to take, the dosage
How to take, the dosage
Novocaine is given intramuscularly – 5-10 ml of 1-2% solution 3 times a week for a month, followed by a 10-day break; for infiltration anesthesia use 0.25-0.5% solutions, for percutaneous – 2% solution.
Ingestion – 1/2 teaspoonful (in pain).
Injection: 1/2 spoonful (in pain).
Interaction
Interaction
Local anesthetics increase the depressing effect of other drugs on the central nervous system. Anticoagulants (sodium ardeparin, sodium dalteparin, sodium danaparoid, sodium enoxaparin, heparin, warfarin) increase the risk of bleeding. Cholinesterase inhibitors (antimiasthenic drugs, cyclo-fosfamide, demecaria bromide, ecothiopath iodide, thiotepa) decrease the metabolism of local anesthetic drugs. The metabolite of procaine (para-aminobenzoic acid) is an antagonist of sulfonamides, which leads to a weakening of antimicrobial action. When used with monoamine oxidase inhibitors (furazolidone, procarbazine, selegiline) increases the risk of decreased blood pressure. Vasoconstrictors (epinephrine, methoxamine, phenylephrine) prolong the local anesthetic effect. Procaine reduces antimyasthenic effect of anticholinesterase drugs, especially when used in high doses, which requires additional correction of myasthenia gravis treatment.
Special Instructions
Special Instructions
During treatment, caution should be exercised when driving motor vehicles and engaging in other potentially hazardous activities that require increased concentration and quick psychomotor reactions.
Patients require monitoring of cardiovascular, respiratory and central nervous system functions. Monoamine oxidase inhibitors should be discontinued 10 days prior to local anesthetic administration.
Contraindications
Contraindications
With caution Emergency surgery accompanied by acute blood loss, conditions accompanied by decreased hepatic blood flow (e.g., chronic heart failure, liver disease), progressive cardiovascular failure (usually due to the development of heart block and shock), proctitis, pseudocholinesterase deficiency, renal failure, in older patients (over 65 years), critically ill, weakened patients. Contraindicated: Hypersensitivity (including to para-aminobenzoic acid and other local anesthetic esters), children (under 18 years).
Side effects
Side effects
Central and peripheral nervous system: headache, dizziness, somnolence, weakness, motor anxiety, loss of consciousness, convulsions, trismus, tremor, visual and auditory disturbances, nystagmus, cauda equina syndrome (leg paralysis, paresthesias), respiratory muscle paralysis, sensory and motor conduction disorders, respiratory center paralysis develops more frequently in subarachnoid anesthesia. Cardiovascular system: increased or decreased blood pressure, peripheral vasodilation, collapse, bradycardia, arrhythmias, chest pain. Digestive system: nausea, vomiting, involuntary defecation. Urinary system: involuntary urination. Blood: methemoglobinemia. Allergic reactions: skin itching, skin rash, other anaphylactic reactions (including anaphylactic shock), urticaria (on skin and mucous membranes), dizziness, weakness, decreased blood pressure. In these cases, you should stop using the drug and consult a physician. Rarely, hyperemia and anal itching (when using in high doses). Local reactions: in the first days of using the drug, there may be urge to defecation and feeling of discomfort, which subsequently disappear on their own and do not require withdrawal of the drug.
Overdose
Overdose
Symptoms: nausea, vomiting, apnea, methemoglobinemia, pallor of skin and mucous membranes, dizziness, cold sweats, tachycardia, increased nervous excitability, reduced blood pressure almost to collapse, tremors, convulsions, respiratory depression, sudden cardiovascular collapse. The effect on the central nervous system is manifested by feelings of fear, motor agitation, hallucinations, seizures. In cases of overdose the drug administration shall be stopped immediately. In case of local anesthesia the injection site may be injected with adrenaline. Treatment: general resuscitation measures that include oxygen inhalation, if necessary, artificial lung ventilation. In cases of arterial hypotension and/or myocardial depression, intravenous ephedrine (15-30 mg), in severe cases, detoxification and symptomatic therapy. If seizures last more than 15-20 seconds, they are stopped by intravenous administration of thiopental (100-150 mg) or diazepam (5-20 mg). If intoxication develops after injection of novocaine into the leg or arm muscles, it is recommended that a tourniquet be applied urgently to reduce the subsequent entry of the drug into the general bloodstream.
Similarities
Similarities
Additional information
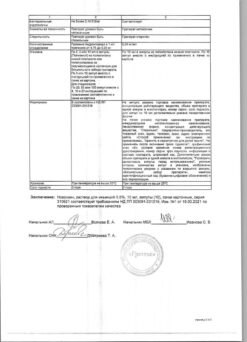
| Shelf life | 3 years |
|---|---|
| Conditions of storage | In a place protected from light |
| Manufacturer | Biokhimik JSC, Russia |
| Medication form | solution for injection |
| Brand | Biokhimik JSC |
Other forms…
Related products
Buy Novocaine, 0.5%, 5 ml, 10 pcs. with delivery to USA, UK, Europe and over 120 other countries.