No products in the cart.
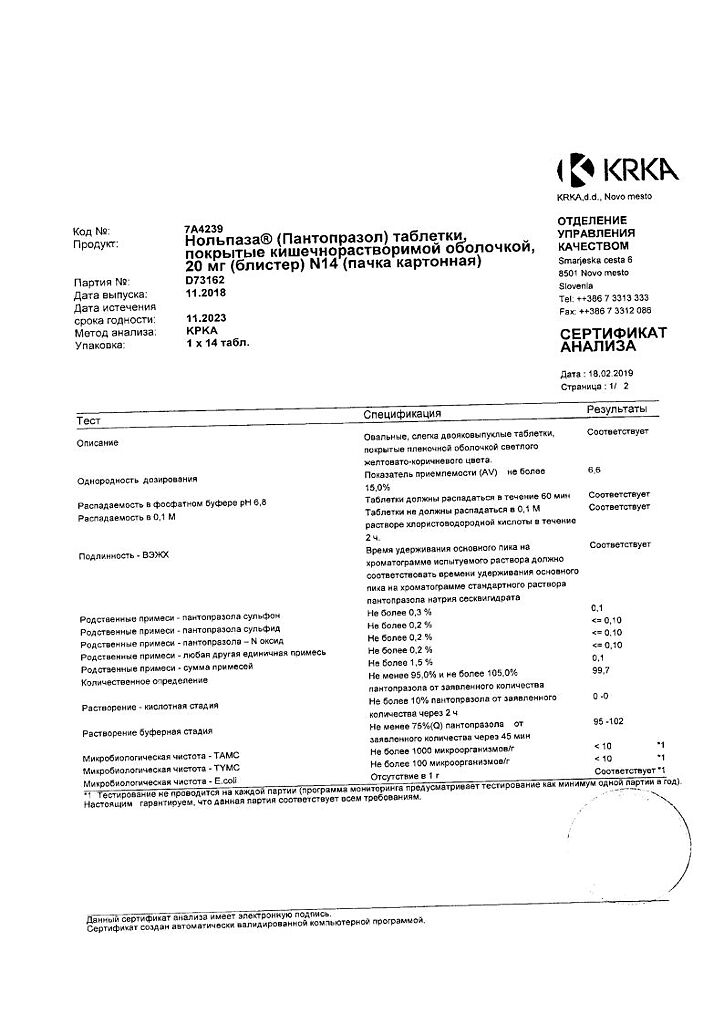
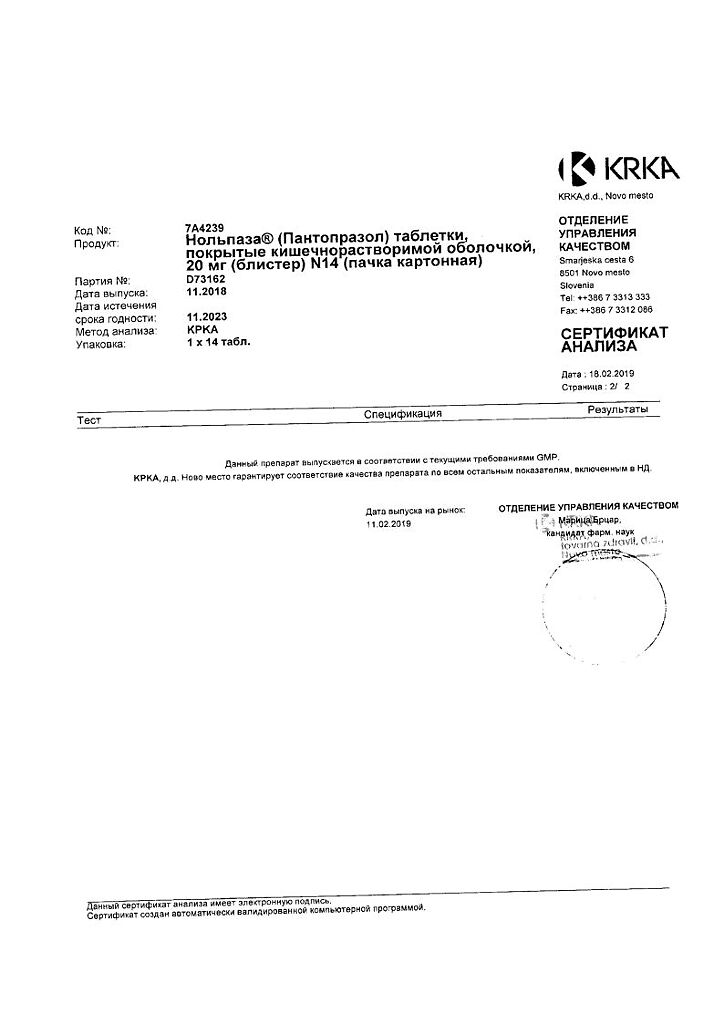
Nolpaza, 20 mg 14 pcs
€6.23 €5.45
EAN: 3838989556976
SKU: 211619
Categories: Medicine, Stomach, intestines, liver, Ulcer and gastritis
Description
Gastric and duodenal ulcer, GI infections caused by Helicobacter pylori, Nausea, Gastritis, Heartburn, Sour belching, Reflux esophagitis
Gastroesophageal reflux disease (GERD), including erosive ulcerative reflux esophagitis and GERD-associated symptoms: heartburn, acid regurgitation, pain on swallowing.
Gastric and duodenal ulcer (in the acute phase), erosive gastritis (including those associated with taking non-steroidal anti-inflammatory drugs (NSAIDs)).
Zollinger-Ellison syndrome.
Eradication of Helicobacter pylori in combination with antibacterial agents.
Indications
Indications
Gastroesophageal reflux disease (GERD), including erosive and ulcerative reflux esophagitis and symptoms associated with GERD: heartburn, acid regurgitation, pain when swallowing.
Peptic ulcer of the stomach and duodenum (in the acute phase), erosive gastritis (including those associated with taking non-steroidal anti-inflammatory drugs (NSAIDs)).
Zollinger-Ellison syndrome.
Eradication of Helicobacter pylori in combination with antibacterial agents.
Pharmacological effect
Pharmacological effect
gastric glands secretion reducing agent – proton pump inhibitor
Special instructions
Special instructions
Liver failure, risk factors for cyanocobalamin (vitamin B12) deficiency (especially against the background of hypo- and achlorhydria).
Contraindicated for persons under 18 years of age.
In patients with severe liver dysfunction, the daily dose of pantoprazole should not exceed 20 mg per day (1 tablet of Nolpaza® 20 mg). In this regard, the use of pantoprazole at a dosage of 40 mg in this group of patients is not recommended. The activity of liver enzymes should be regularly monitored during treatment with pantoprazole, especially with long-term use of the drug. If the activity of liver enzymes increases, treatment should be discontinued.
No dose adjustment is required in elderly patients and patients with renal failure.
Due to the lack of data on the use of Nolpaza® as part of combination antimicrobial therapy against Helicobacter pylori in patients with impaired renal function, as well as in patients with moderate and severe liver failure, the drug should not be used.
Before starting treatment with Nolpaza®, the possibility of a malignant neoplasm should be excluded, since the drug can mask symptoms and delay the correct diagnosis.
Patients should consult their physician if they are undergoing an endoscopy or urea breath test.
Patients should consult a doctor if the following occur:
unintentional weight loss, anemia, gastrointestinal bleeding, difficulty swallowing, persistent vomiting or vomiting blood. In these cases, taking the drug may partially relieve symptoms and delay correct diagnosis;
previous surgery on the gastrointestinal tract or gastric ulcer;
continuous symptomatic treatment of dyspepsia and heartburn for 4 weeks or more;
liver diseases, including jaundice and liver failure;
other serious diseases that worsen general health.
Patients over the age of 55 who have new or recently changed symptoms should consult a doctor.
When taking drugs that reduce the acidity of gastric juice, the risk of gastrointestinal infections caused by bacteria of the genus Salmonella spp., Campylobacter spp. slightly increases. or C. difficile.
In patients with Zollinger-Ellison syndrome and other pathological hypersecretory conditions who require long-term treatment, pantoprazole, like other drugs that block gastric acid secretion, may reduce the absorption of vitamin B12 (cyanocobalamin) due to hypo- and achlorhydria. This should be taken into account when treating patients with reduced reserves of this vitamin in the body, or during long-term treatment of patients with risk factors for developing vitamin B12 deficiency, as well as when observing corresponding clinical symptoms.
Long-term therapy, especially lasting more than 1 year, requires regular monitoring of patients.
Pantoprazole is not recommended for use with HIV protease inhibitors, the absorption of which depends on gastric pH (for example, atazanavir), due to a significant decrease in their bioavailability.
There are reports of the development of severe hypomagnesemia in patients receiving PPIs for at least 3 months, and in most cases for a year. Serious manifestations of hypomagnesemia, such as fatigue, tetany, delirium, convulsions, dizziness and ventricular arrhythmia, may occur, but hypomagnesemia may develop unnoticed and not be recognized in a timely manner. In most patients with hypomagnesemia, it decreases after magnesium replacement therapy and discontinuation of PPIs. In patients undergoing long-term treatment or in patients receiving PPIs concomitantly with digoxin or other drugs that can cause hypomagnesemia (eg, diuretics), serum magnesium levels should be determined before initiating PPI treatment and periodically during treatment.
Proton pump inhibitors, especially when used in high doses and over a long period of time (> 1 year), may slightly increase the risk of fractures of the femur, wrist and spine, mainly in elderly patients or those with other recognized risk factors. Observational studies indicate that proton pump inhibitors may increase the overall risk of fracture by 10% to 40%. Some of these fractures may be due to other risk factors. Patients at risk of osteoporosis should receive treatment in accordance with current clinical guidelines and adequate amounts of vitamin D and calcium.
When treating PPI, the development of subacute cutaneous lupus erythematosus is very rarely observed. If skin lesions occur, especially in sun-exposed areas, or in the presence of concomitant arthralgia, the patient should seek immediate medical attention and a healthcare professional should evaluate the need to discontinue treatment with Nolpaza. The occurrence of PCLE after previous treatment with a PPI may increase the risk of developing PCLE during treatment with other proton pump inhibitors.
When conducting laboratory tests, it is necessary to take into account that increased levels of CgA in the blood serum may distort the results of diagnostic studies to identify neuroendocrine tumors. In this regard, the use of the drug Nolpaza® should be stopped at least 5 days before the CgA content study. If CgA and gastrin levels have not returned to normal values after the first determination, the study should be repeated 14 days after stopping the proton pump inhibitor.
Impact on the ability to drive vehicles and machinery
You should refrain from driving vehicles and other mechanisms that require increased attention due to the likelihood of dizziness and visual impairment.
You should refrain from driving vehicles and other mechanisms that require increased attention due to the likelihood of dizziness and visual impairment.
Active ingredient
Active ingredient
Pantoprazole
Composition
Composition
for 1 tablet 20 mg/40 mg
Core:
Active ingredient:
Pantoprazole sodium sesquihydrate 22.55 mg/45.10 mg, equivalent to pantoprazole 20.00 mg/40.00 mg
Excipients: mannitol, crospovidone, sodium carbonate, sorbitol, calcium stearate
Film shell:
Hypromellose, povidone K-25, titanium dioxide (E171), iron oxide yellow dye (E172), propylene glycol, methacrylic acid and ethyl acrylate copolymer (1:1), 30% dispersion1, talc, macrogol-6000
1 Polymer dispersion contains 0.7% sodium lauryl sulfate and 2.3% polysorbate-80 as emulsifiers.
Pregnancy
Pregnancy
Pregnancy
As a precautionary measure, it is necessary to avoid the use of Nolpaza® during pregnancy.
Breastfeeding period
Due to insufficient information on the use of Nolpaza® in women during breastfeeding, a potential risk for newborns and breastfed infants cannot be excluded. In this regard, it is necessary to make a decision to stop breastfeeding or to cancel/suspension of treatment with Nolpaza®.
Fertility
There are no data on the effects of Nolpaza® on fertility in humans. Preclinical studies have shown no effect on male or female fertility.
Contraindications
Contraindications
Hypersensitivity to any of the components of the drug, as well as to substituted benzimidazoles.
Dyspepsia of neurotic origin.
Concomitant use of HIV protease inhibitors, such as atazanavir, nelfinavir, and drugs whose absorption depends on the acidity (pH) of gastric juice.
Children under 18 years of age.
Pregnancy, breastfeeding period.
Patients with congenital fructose intolerance are not recommended to take Nolpaza®, since it contains sorbitol.
Side Effects
Side Effects
Approximately 5% of patients can be expected to develop adverse drug reactions (ADRs). The most common ADRs are diarrhea and headache, occurring in approximately 1% of patients.
The following are listed ADRs reported with pantoprazole, classified according to frequency as follows:
very often (³ 1/10)
often (³ 1/100 and < 1/10)
uncommon (³ 1/1000 and < 1/100)
rare (³ 1/10,000 and < 1/1000)
very rare (< 1/10,000)
frequency unknown (cannot be estimated from available data).
For adverse reactions identified during post-marketing use of the drug, it is not possible to apply any frequency category and are therefore listed as “frequency unknown”.
Within each frequency group, adverse reactions are presented in order of decreasing severity.
Blood and lymphatic system disorders:
rarely: agranulocytosis;
very rarely: thrombocytopenia, leukopenia, pancytopenia.
Immune system disorders:
rarely: hypersensitivity (including anaphylactic reactions, including anaphylactic shock).
Metabolic and nutritional disorders:
rarely: hyperlipidemia and increased concentrations of lipids (triglycerides, cholesterol) in the blood plasma, changes in body weight;
frequency unknown: hyponatremia, hypomagnesemia, hypocalcemia in combination with hypomagnesemia, hypokalemia.
Mental disorders:
uncommon: sleep disturbance;
rarely: depression (including exacerbations of existing disorders);
very rarely: disorientation (including exacerbations of existing disorders);
frequency unknown: hallucinations, confusion (especially in predisposed patients, as well as possible exacerbation of symptoms if they were present before using the drug).
Nervous system disorders:
uncommon: headache, dizziness;
rarely: dysgeusia (taste disturbance);
frequency unknown: paresthesia.
Visual disorders:
rare: visual impairment/blurred vision.
Gastrointestinal disorders:
often: glandular polyps of the fundus of the stomach (benign);
uncommon: diarrhea, nausea/vomiting, bloating and flatulence, constipation, dry mouth, abdominal pain and discomfort;
frequency unknown: microscopic colitis.
Disorders of the liver and biliary tract:
uncommon: increased activity of liver enzymes (transaminases, γ-glutamyltransferase) in the blood plasma;
rarely: increased concentration of bilirubin in blood plasma;
frequency unknown: hepatocellular damage, jaundice, hepatocellular failure.
Disorders of the skin and subcutaneous tissues:
uncommon: skin rash/exanthema/rash, itching;
rarely: urticaria, angioedema;
frequency unknown: erythema malignant exudative (Stevens-Johnson syndrome), toxic epidermal necrolysis (Lyell’s syndrome), erythema multiforme exudative, photosensitivity, subacute cutaneous lupus erythematosus (SCLE).
Musculoskeletal and connective tissue disorders:
uncommon: fracture of the femoral neck, wrist bones or spine;
rarely: arthralgia, myalgia;
frequency unknown: muscle spasm as a consequence of electrolyte imbalance.
Renal and urinary tract disorders:
frequency unknown: interstitial nephritis (with possible progression to renal failure).
Disorders of the genital organs and breast:
rarely: gynecomastia.
General disorders and disorders at the injection site:
uncommon: asthenia, excessive fatigue and malaise;
rarely: increased body temperature, peripheral edema.
Interaction
Interaction
The simultaneous use of other proton pump inhibitors or H2-histamine receptor blockers is not recommended without consulting a doctor.
Concomitant use of Nolpaza® may reduce the absorption of drugs whose bioavailability depends on the pH of the stomach (for example, ketoconazole, itraconazole, posaconazole and other drugs such as erlotinib).
During drug interaction studies, no clinically significant interactions were identified when using pantoprazole in the following cases:
patients with diseases of the cardiovascular system taking cardiac glycosides (digoxin), slow calcium channel blockers (nifedipine), beta-blockers (metoprolol);
patients with gastrointestinal diseases taking antacids, antibiotics (amoxicillin, clarithromycin);
patients taking oral contraceptives containing levonorgestrel and ethinyl estradiol;
patients taking non-steroidal anti-inflammatory drugs (diclofenac, naproxen, piroxicam);
patients with diseases of the endocrine system taking glibenclamide, levothyroxine;
patients with anxiety and sleep disorders taking diazepam;
patients with epilepsy taking carbamazepine and phenytoin;
patients taking indirect anticoagulants, such as warfarin and phenprocoumon, under the control of prothrombin time and international normalized ratio (INR) at the beginning and at the end of treatment, as well as during irregular use of pantoprazole. At the same time, it should be noted that there are known cases of increased INR and prothrombin time in patients receiving PPIs along with warfarin or phenprocoumon. An increase in INR and prothrombin time can lead to pathological bleeding that is life-threatening. In this regard, such patients should be monitored for increases in INR and prothrombin time.
The absence of clinically significant drug interactions with caffeine, ethanol, and theophylline was also noted.
There are reports of increased blood levels of methotrexate in some patients when used in high doses (eg, 300 mg) with a PPI. Therefore, when high doses of methotrexate are used, for example in cancer or psoriasis, it may be necessary to consider temporary withdrawal of pantoprazole.
Inhibitors of CYP2C19 activity, such as fluvoxamine, may increase the systemic exposure of pantoprazole. A dose reduction may be necessary in patients receiving long-term treatment with high doses of pantoprazole or in patients with hepatic impairment.
Inducers of the activity of the CYP2C19 and CYP3A4 isoenzymes, such as rifampicin and St. John’s wort (Hypericum perforatum), can reduce the plasma concentrations of PPIs metabolized by these enzyme systems.
HIV protease inhibitors
Pantoprazole is not recommended for use with HIV protease inhibitors, the absorption of which depends on gastric pH (for example, atazanavir), due to a significant decrease in their bioavailability.
If concomitant use of HIV protease inhibitors and PPIs is still necessary, careful clinical monitoring (for example, determination of viral load) is recommended. The dose of pantoprazole should not exceed 20 mg per day. The HIV protease inhibitor dosage may also need to be adjusted.
Overdose
Overdose
There have been no cases of overdose resulting from the use of Nolpaza®.
Doses of pantoprazole up to 240 mg were administered intravenously over 2 minutes and were well tolerated.
In case of overdose and only when clinical manifestations appear, symptomatic and supportive therapy is carried out. Pantoprazole is not eliminated by hemodialysis.
Clinical pharmacology
Clinical pharmacology
Pharmacodynamics
Proton pump inhibitor (H+/K+-ATPase). Blocks the final stage of hydrochloric acid secretion, regardless of the nature of the stimulus.
Pantoprazole is a substituted benzimidazole that suppresses the secretion of hydrochloric acid in the stomach by specifically blocking the proton pumps of parietal cells.
Pantoprazole is transformed into its active form under acidic conditions in parietal cells, where it suppresses the activity of the H+/K+-ATPase enzyme, i.e., it blocks the final stage of the formation of hydrochloric acid in the stomach. Suppression of activity is dose-dependent and results in a decrease in both basal and stimulated acid secretion. Treatment with pantoprazole, as with other proton pump inhibitors (PPIs) and H2 receptor blockers, reduces gastric acidity and thereby increases gastrin levels in proportion to the decrease in acidity. The increase in gastrin levels is reversible. Because pantoprazole binds the enzyme distal to the cellular receptor, it can inhibit the secretion of hydrochloric acid regardless of stimulation by other substances (acetylcholine, histamine, gastrin).
The effect of oral and intravenous use of the drug is the same.
The content of chromogranin A (CgA) in the blood serum also increases due to a decrease in the secretion of hydrochloric acid. Elevated levels of CgA may distort the results of diagnostic tests for the detection of neuroendocrine tumors.
Antisecretory activity
After the first oral dose of 20 mg of Nolpaza®, a decrease in gastric juice secretion by 24% occurs after 2.5-3.5 hours and by 26% after 24.5-25.5 hours. After oral administration of pantoprazole once a day for 7 days, its antisecretory activity, measured 2.5-3.5 hours after administration, increases to 56%, and after 24.5-25.5 hours – up to 50%. In case of duodenal ulcer associated with Helicobacter pylori, a decrease in gastric secretion increases the sensitivity of microorganisms to antibiotics. Does not affect gastrointestinal motility. Secretory activity returns to normal 3-4 days after the end of treatment.
Compared to other PPIs, Nolpaza® has greater chemical stability at neutral pH, and a lower potential for interaction with the liver oxidase system, which is dependent on the cytochrome P450 system. Therefore, no clinically significant interactions were observed between Nolpaza® and many other drugs.
Pharmacokinetics
Pantoprazole is rapidly absorbed after oral administration. The maximum concentration (Cmax) in blood plasma after oral administration is achieved after the first dose of 20 mg or 40 mg. Cmax of about 1.0-1.5 mcg/ml is achieved on average approximately 2.0-2.5 hours after taking a dose of 20 mg and about 2.0-3.0 mcg/ml – 2.5 hours after taking a dose of 40 mg. Cmax remains constant after repeated administration of the drug.
The pharmacokinetics of pantoprazole after single and repeated use are the same. In the dose range of 10-80 mg, the pharmacokinetics of pantoprazole in blood plasma remains linear with both oral and intravenous administration.
The absolute bioavailability of pantoprazole tablets is about 77%. Joint food intake does not affect the area under the concentration-time curve (AUC), Cmax in the blood serum and, accordingly, bioavailability. When taken together with food, the time for the onset of action of the drug may vary. The binding of pantoprazole to plasma proteins is 98%. The volume of distribution is 0.15 l/kg.
Metabolized mainly in the liver. The main metabolic pathway is demethylation by the CYP2C19 isoenzyme followed by sulfate conjugation. Other metabolic pathways include oxidation via the CYP3A4 isoenzyme.
The terminal half-life (T1/2) is approximately 1 hour, and the clearance is about 0.1 l/h/kg. Due to the specific binding of pantoprazole to proton pumps of parietal cells, T1/2 does not correlate with a much longer duration of action (inhibition of acid secretion).
The main route of elimination is by the kidneys (about 80%) in the form of pantoprazole metabolites, the rest is excreted in feces. The main metabolite in blood plasma and urine is desmethylpantoprazole, which is conjugated with sulfate. T1/2 of the main metabolite is about 1.5 hours, which is slightly higher than T1/2 of pantoprazole.
In individuals with low functional activity of the CYP2C19 isoenzyme (slow metabolizers), pantoprazole is probably metabolized mainly by the CYP3A4 isoenzyme. After a single dose of pantoprazole 40 mg, the mean area under the concentration-time curve was approximately 6 times greater in poor metabolizers than in subjects with a functionally active CYP2C19 isoenzyme (extensive metabolizers). Average Cmax values in blood plasma are increased by approximately 60%. These features do not affect the dosage of pantoprazole.
When using pantoprazole in patients with limited renal function (including patients on hemodialysis), no dose reduction is required. As in healthy volunteers, T1/2 of pantoprazole is short. Only a very small portion of the drug is dialyzed. Despite the moderately long half-life of the main metabolite (2-3 hours), its elimination occurs quite quickly, and therefore accumulation does not occur.
In patients with liver cirrhosis (classes A and B according to the Child-Pugh classification), T1/2 time increases to 3-6 hours, AUC values increase by 3-5 times, Cmax in serum increases slightly, only 1.3 times compared to that in healthy volunteers when using pantoprazole at a dosage of 20 mg and, accordingly, when using pantoprazole at a dosage of 40 mg, T1/2 time increases to 7-9 h, AUC values increase 5-7 times, Cmax in serum increases 1.5 times compared to that in healthy volunteers.
The slight increase in AUC and Cmax in elderly patients compared with the corresponding values in younger individuals is not clinically significant.
Storage conditions
Storage conditions
At a temperature not exceeding 25 ºС, in the original packaging.
Keep out of the reach of children.
Shelf life
Shelf life
5 years.
Do not use the drug after the expiration date.
Manufacturer
Manufacturer
KRKA-RUS, Russia
Additional information
| Shelf life | 5 years. Do not use the product after the expiration date. |
|---|---|
| Conditions of storage | At the temperature not more than 25 ºС, in the original package. Keep out of reach of children. |
| Manufacturer | KRKA-RUS, Russia |
| Medication form | enteric soluble tablets |
| Brand | KRKA-RUS |
Related products
Buy Nolpaza, 20 mg 14 pcs with delivery to USA, UK, Europe and over 120 other countries.