No products in the cart.
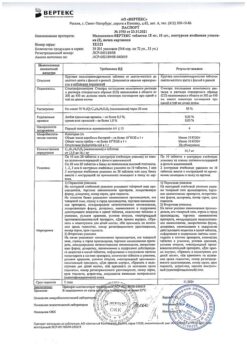
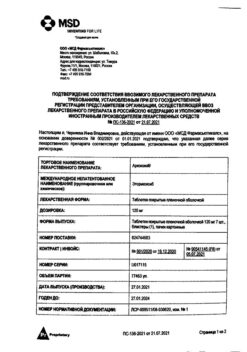
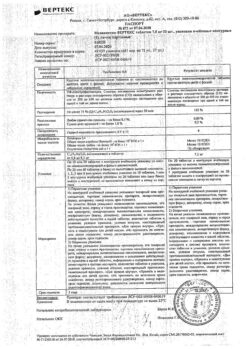
Nobedolak 400 mg 14 pcs
€12.48 €10.35
SKU: 0001650
Categories: Joint diseases, Medicine, Pain and fever
Description
inflammatory and degenerative diseases of the musculoskeletal system: psoriatic, rheumatoid, gouty arthritis, ankylosing spondylitis (Bechterew’s disease), osteoarthritis;
• pain syndrome: myalgia, ossalgia, arthralgia, headache and toothache, post-traumatic pain syndrome accompanied by inflammation, algomenorrhea;
• intended for symptomatic therapy, reduction of pain and inflammation at the time of use, does not affect the progression of the disease.
Composition
Composition
1 film-coated tablet contains:
active ingredient: Etodolac DC (98%) (equivalent to 400 mg etodolac) 408.0 mg;
excipients: lactose anhydrous 146.50 mg, microcrystalline cellulose PH 200 245.00 mg, sodium croscarmellose 34.50 mg, colloidal silicon dioxide anhydrous (Aerosil 200) 2.00 mg, magnesium stearate 13.00 mg, povidone K30 16.00 mg;
film coating: (opadry II pink (85F240035)) 40.00 mg: polyvinyl alcohol (E 1203) 40.000%, titanium dioxide (E 171) 24.930%, macrogol 20.200%, talc 14.800%, iron oxide red (E 172) 0.070%.
Contraindications
Contraindications
• hypersensitivity to etodolac or other components of the drug;
• intolerance to acetylsalicylic acid and pyrazolone series drugs;
• contraindicated in the period after coronary artery bypass grafting;
• decompensated heart failure;
• complete or incomplete combination of bronchial asthma, recurrent polyposis of the nose and paranasal sinuses and intolerance to acetylsalicylic acid and other NSAIDs (including history);
• erosive and ulcerative changes in the mucous membrane of the stomach or duodenum, active gastrointestinal bleeding;
• history of gastrointestinal bleeding or perforation of ulcers caused by NSAID use;
• inflammatory bowel diseases (ulcerative colitis, Crohn’s disease);
• rare hereditary diseases (lactose intolerance, lactase deficiency, glucose-galactose malabsorption (due to the presence of lactose)).
• cerebrovascular bleeding or other bleeding;
• severe liver failure or active liver disease;
• severe renal failure in patients not undergoing dialysis (creatinine clearance less than 30 ml/min), progressive kidney disease including confirmed hyperkalemia;
• pregnancy, breastfeeding period;
• children under 15 years of age.
Carefully
Ischemic heart disease, cerebrovascular disease, chronic heart failure, dyslipidemia/hyperlipidemia, diabetes mellitus, peripheral arterial disease, smoking, liver failure, chronic renal failure (CC 30-60 ml/min).
Concomitant use of other NSAIDs, gastritis, enteritis, colitis, bronchial asthma or allergic diseases in the acute stage or in the anamnesis – possible development of bronchospasm, systemic lupus erythematosus or mixed connective tissue disease (Sharp’s syndrome) – increased risk of aseptic meningitis, liver cirrhosis with portal hypertension, hyperbilirubinemia, nephrotic syndrome, arterial hypertension, edema. Anamnestic data on the development of ulcerative lesions of the gastrointestinal tract, the presence of Helicobacter pylori infection, old age, long-term use of NSAIDs, frequent alcohol consumption, severe somatic diseases, concomitant use of drugs that can increase the risk of ulcers or bleeding:
• anticoagulants (eg, warfarin);
• antiplatelet agents (eg, acetylsalicylic acid, clopidogrel);
• oral glucocorticosteroids (eg, prednisolone);
• selective serotonin reuptake inhibitors (eg, citalopram, fluoxetine, paroxetine, sertraline);
• children under 18 years of age.
To reduce the risk of developing adverse events from the gastrointestinal tract, the minimum effective dose should be used for the shortest possible course.
Use during pregnancy and breastfeeding
Etodolac is contraindicated for use in pregnant women and women during breastfeeding.
Method of administration and dosage
Method of administration and dosage
Adults and children over 18 years of age: the recommended daily dose of Nobedolak® is 400 – 1200 mg. The maximum daily dose is 1200 mg. The drug is prescribed twice a day: 1 tablet in the morning and evening after meals. If necessary, the dose can be increased to 3 tablets per day.
For patients weighing less than 60 kg, the maximum daily dose of the drug should not exceed 20 mg/kg.
In rheumatic diseases, the course of treatment depends on the effectiveness of therapy and the nature of the disease. In case of a long course of therapy, the dose should be adjusted every 2-3 weeks of use of the drug.
In the treatment of pain conditions due to acute inflammatory processes (such as toothache, myositis, tendinitis), as well as postoperative pain syndromes, the course of treatment is 5 days. For headaches and menstrual pain, Nobedolak® is prescribed 1-2 tablets per day as needed, for no more than 3 days.
Special instructions
Special instructions
To reduce the risk of developing adverse events, the minimum effective dose should be used for the shortest possible course.
Cardiac disorders
In studies of some selective COX-2 inhibitors and non-selective NSAIDs, cardiovascular thrombotic complications, myocardial infarction, and seizures that can lead to death have been reported. All NSAIDs, both selective and non-selective, may cause such a risk. To reduce the severity of adverse reactions from the cardiovascular system, the lowest effective dose of NSAIDs should be used for the shortest possible period. Cardiac disorders may occur even without previous symptoms. There is no evidence that acetylsalicylic acid alleviates symptoms from the cardiovascular system.
The use of NSAIDs for pain relief in the first 10-14 days of coronary artery bypass grafting increases the risk of myocardial infarction (see section “Contraindications”).
Concomitant use of etodolac and other NSAIDs, including selective COX-2 inhibitors, should be avoided.
Arterial hypertension
NSAIDs, including etodolac, may increase blood pressure or worsen existing hypertension, which may lead to adverse cardiovascular effects. Patients taking thiazide and loop diuretics concomitantly with etodolac may experience a decrease in the effect of the latter. Blood pressure should be monitored while taking NSAIDs.
Chronic heart failure and edema
Fluid retention and edema have been reported in patients taking NSAIDs. Etodolac should be used with caution in patients with fluid retention or heart failure.
Effect on the gastrointestinal tract
NSAIDs, including etodolac, can cause serious gastrointestinal side effects, including inflammation, bleeding, ulceration, or perforation of the stomach or intestines, which can lead to death.
NSAIDs should be used with caution in patients with a history of gastric and duodenal ulcers or gastrointestinal bleeding. Other risk factors that increase the risk of gastrointestinal bleeding include concomitant oral corticosteroids, anticoagulants, prolonged use of NSAIDs, smoking, alcohol consumption, advanced age, and severe general condition. Most spontaneous reports have been reported in elderly and debilitated patients. To reduce the potential risk of gastrointestinal adverse reactions, use the lowest effective dose for the shortest period. It is necessary to be aware of the symptoms of gastrointestinal bleeding and ulcers during treatment with NSAIDs; if adverse reactions are suspected, the patient’s condition should be assessed, the drug should be discontinued, and appropriate measures should be taken. In such patients, combination therapy with gastroprotectors (eg, misoprostol or proton pump inhibitors) should be considered.
Effect on the kidneys
Long-term use of NSAIDs may cause papillary necrosis and other renal damage. Renal prostaglandins play a compensatory role in maintaining renal perfusion. Patients taking NSAIDs may experience a dose-dependent decrease in prostaglandin formation, which leads to the development of renal decompensation. Patients at high risk of developing these reactions include those with impaired renal function, heart failure, impaired liver function, those taking diuretics and ACE inhibitors, and elderly patients. Discontinuation of NSAIDs leads to restoration of the previous condition.
Worsening of kidney disease
There is no information on the use of etodolac in patients with advanced renal failure, so etodolac is not recommended in these patients. Renal function should be monitored before starting treatment with etodolac.
Anaphylactic reactions.
As with other NSAIDs, anaphylactic reactions with or without a history of hypersensitivity reactions may occur in patients taking NSAIDs. The drug should not be used in patients with aspirin-sensitive asthma. These symptoms occur in patients with asthma with rhinitis with or without nasal polyps or with the development of severe, potentially fatal cases of bronchospasm after taking acetylsalicylic acid or other NSAIDs.
NSAIDs, including etodolac, may cause severe skin reactions such as exfoliative dermatitis, Stevens-Johnson syndrome, and toxic epidermal necrolysis, sometimes resulting in death. Patients should be advised of the symptoms of severe skin reactions. Patients are at increased risk of such reactions early in therapy: most reactions occur within the first month of treatment. If skin rash or other hypersensitivity reactions occur, the drug should be discontinued.
Patients with systemic lupus erythematosus and mixed connective tissue diseases may be at increased risk of aseptic meningitis.
Are common
Etodolac is not a substitute for corticosteroids in cases of corticosteroid insufficiency. Abrupt discontinuation of etodolac may result in exacerbation of the disease. Patients taking corticosteroids for a long time should discontinue them gradually.
Effect on the liver
Liver enzymes are increased with etodolac. Laboratory changes may progress, remain unchanged, or resolve after discontinuation of therapy. Significant increases in ALT and AST (3-fold or more) were observed in 1% of patients during clinical trials of NSAIDs. Isolated cases of severe liver reactions have been reported, including jaundice and fatal fulminant hepatitis, liver necrosis, liver failure, sometimes fatal. If clinical symptoms of renal dysfunction develop, systemic manifestations (eosinophilia, skin rash) are possible, in which case etodolac should be discontinued.
Effect on blood
Sometimes, when using NSAIDs, including etodolac, anemia is observed due to fluid retention in the body, gastrointestinal bleeding, and impaired erythropoiesis. With prolonged use of NSAIDs, including etodolac, it is necessary to monitor the level of hemoglobin and hematocrit in the blood. NSAIDs inhibit platelet aggregation and prolong bleeding time in some patients. Compared with acetylsalicylic acid, the effect of etodolac on platelets is significantly less, the duration of treatment is reduced, and the opposite effect is noted. In patients taking etodolac and anticoagulants, it is necessary to monitor the level of platelets in the blood, since coagulation may change.
Bronchial asthma
In patients with bronchial asthma, drug-induced asthma is possible. The use of acetylsalicylic acid in drug-induced asthma causes severe bronchospasm. The drug should not be taken by patients with a history of asthma, rhinitis, urticaria during treatment with other NSAIDs.
The product contains lactose and should not be used in cases of hereditary galactose intolerance, Lapp lactase deficiency or glucose-galactose malabsorption.
Fertility
Etodolac may impair female fertility and is not recommended for use in women trying to conceive. In women who are having difficulty conceiving or undergoing infertility investigations, discontinuation of etodolac should be considered.
Children
Do not use in children.
Impact on the ability to drive vehicles and operate machinery
The use of the drug may cause undesirable effects in the form of headaches and dizziness. You should refrain from driving vehicles and performing actions that require increased concentration and speed of psychomotor reactions.
Side effects
Side effects
The frequency of side effects is classified in accordance with the recommendations of the World Health Organization: very often – not less than 10%; often – not less than 1% but less than 10%; infrequently – not less than 0.1% but less than 1%; rarely – not less than 0.01% but less than 0.1%; very rarely – less than 0.01%; unknown frequency – cannot be estimated based on the available data.
From the blood and lymphatic system:
uncommon – leukopenia;
very rarely –
thrombocytopenia, hemolytic anemia, neutropenia, pancytopenia, lymphadenopathy, aplastic anemia, and agranulocytosis.
Allergic reactions:
uncommon – hypersensitivity reaction;
unknown frequency – anaphylactic reaction (including anaphylactic shock), Quincke’s edema.
From the nervous system:
often –
headache;
uncommon – dizziness,
taste disturbances, asthenia/weakness, paresthesia, drowsiness, insomnia,
nervousness depression;
rarely – impaired consciousness, agitation, sleep disturbance, convulsions, coma, hallucinations, meningitis, tremor, fatigue;
Unknown frequency – reports of aseptic meningitis (especially in patients with autoimmune disorders such as systemic lupus erythematosus, mixed connective tissue disease).
From the side of the organ of vision:
uncommon – blurred vision, photophobia, transient visual disturbances, conjunctivitis.
From the side of the organ of hearing:
Unknown frequency – hearing loss including deafness and/or tinnitus.
From the cardiovascular system:
infrequently – a feeling of palpitations, “flushes” of blood to the face;
unknown frequency – arterial hypertension, chronic heart failure, syncope, vasculitis (including necrotizing and allergic), torsades de pointes, ventricular tachycardia, arterial thrombotic complications (myocardial infarction or stroke).
From the respiratory system:
uncommon – dyspnea, pulmonary infiltration with eosinophilia, bronchitis, bronchial asthma, pharyngitis, rhinitis, sinusitis, respiratory depression, pneumonia, nosebleed.
From the gastrointestinal tract:
uncommon: abdominal pain, constipation, diarrhea, dyspepsia, flatulence, bleeding/perforation, heartburn, nausea, vomiting, vomiting of blood, glossitis, ulcer (stomach/duodenum) with or without bleeding and/or perforation, gastritis, melena, thirst, dry mouth, ulcerative stomatitis, anorexia, belching;
very rare: intestinal ulceration, pancreatitis, esophagitis with or without strictures or cardiospasm, colitis.
From the kidneys and urinary tract:
uncommon: water-electrolyte imbalance, hypernatremia, dysuria, frequent urination, increased urea levels, renal failure, renal papillary necrosis, oliguria, polyuria, proteinuria, cystitis, hematuria, leukorrhea;
unknown frequency: kidney stones, interstitial nephritis, irregular uterine bleeding, nephrotoxicity, hyperkalemia.
From the liver and biliary system
paths:
uncommon increase in the activity of “liver” transaminases;
unknown frequency cholestatic hepatitis, hepatitis, cholestatic jaundice, duodenitis, jaundice, liver failure, liver necrosis.
From the skin and subcutaneous tissues:
uncommon: itching, skin rash, angioedema, increased sweating, urticaria, vesiculobullous changes, cutaneous vasculitis with purpura;
rarely – photosensitivity reaction;
unknown frequency – Stevens-Johnson syndrome, toxic epidermal necrolysis, erythema multiforme, hyperpigmentation, alopecia, maculopapular rash, skin peeling.
Metabolic disorders:
uncommon: edema, increased creatinine levels, hyperglycemia in patients with controlled blood glucose levels, changes in body weight in patients with diabetes mellitus;
Others:
uncommon – chills and fever, infections, sepsis, feeling of fatigue.
Drug interactions
Drug interactions
Antihypertensive drugs
Nobedolak® reduces the effect of antihypertensive drugs, ACE inhibitors.
Antacid drugs
When antacids are used simultaneously, there is no effect on the overall absorption of etodolac. Antacids can reduce Cmax of etodolac by 15 to 20%, but there is no determining effect on Cmax.
Quinolone antibiotics
Animal data suggest that NSAIDs may increase the risk of seizures associated with quinolone antibiotics. Patients taking NSAIDs and quinolones may have an increased risk of developing seizures.
Enhances the effect of oral hypoglycemic agents, phenytoin.
Other NSAIDs, including selective COX-2 inhibitors
Concomitant use of two or more NSAIDs (including acetylsalicylic acid) should be avoided due to the potential for increased incidence of adverse effects.
Cyclosporine, digoxin, methotrexate, tacrolimus
Etodolac, like other NSAIDs, can affect the excretion of prostaglandins, leading to an increase in the level of cyclosporine, digoxin, methotrexate and increasing their toxicity. Increased nephrotoxicity of tacrolimus and cyclosporine is possible.
When taken simultaneously with cardiac glycosides, NSAIDs may worsen heart failure, reduce the glomerular filtration rate and increase the concentration of cardiac glycosides in the blood plasma.
When used simultaneously with methotrexate, the side effects of the latter on the hematopoietic system are enhanced (risk of developing anemia and leukopenia, periodic monitoring of the general blood test is indicated).
To avoid specific toxicity of these drugs, it is necessary to carefully monitor the condition of patients taking etodolac or other NSAIDs, especially in patients with impaired renal function.
Diuretics
There are no data on interaction reactions with the simultaneous use of furosemide and hydrochlorothiazide. However, there are reports that etodolac in some patients reduces the natriuretic effect of furosemide and thiazides. This occurs due to the inhibition of prostaglandin synthesis. It is necessary to avoid the simultaneous administration of etodolac and diuretics due to a decrease in the diuretic effect on the one hand and an increased risk of kidney damage on the other. It is necessary to monitor kidney function.
Glibenclamide
There are no data on the pharmacokinetic interaction of etodolac and glibenclamide.
Lithium
NSAIDs can increase the level of lithium in the blood plasma and reduce the renal clearance of lithium. The average Cmax of lithium in the blood increases by 15%, and the renal clearance decreases by 20%, respectively. This occurs due to the inhibition of prostaglandin synthesis by the kidneys. Therefore, with the simultaneous use of lithium and etodolac, lithium toxicity increases.
Monitoring of lithium blood concentrations is recommended.
Phenylbutazone
Concomitant use of phenylbutazone and etodolac is not recommended, since phenylbutazone increases (up to 80%) the free fraction of etodolac; in vivo studies have not been conducted.
Phenytoin
There are no apparent pharmacokinetic interactions between phenytoin and etodolac.
Warfarin
When used simultaneously with anticoagulants (heparin, ticlopidine), as well as with thrombolytic drugs (streptokinase, fibrinolysin), the risk of bleeding increases (periodic monitoring of blood clotting parameters is necessary).
When used concomitantly with antiplatelet agents and selective serotonin reuptake inhibitors, the risk of gastrointestinal bleeding increases.
When using NSAIDs and warfarin, the risk of ulcers and gastrointestinal bleeding increases. A short-term pharmacokinetic study shows that when warfarin and etodolac are used simultaneously, the binding of warfarin to plasma proteins decreases, but the clearance of warfarin does not change. With this combination, prothrombin time should be monitored to avoid bleeding.
Because etodolac is highly bound to plasma proteins, dosage adjustments of other drugs that bind to plasma proteins may be necessary.
Due to the presence of phenolic metabolites of etodolac in urine, false-positive results of bilirubin tests (with Ehrlich reagent) are possible.
Zidovudine
The risk of hematological toxicity increases with the concomitant use of NSAIDs and zidovudine. There is evidence of an increased risk of hemarthrosis and hematoma in HIV-positive patients with hemophilia who received zidovudine and ibuprofen concomitantly.
Mifepristone
NSAIDs should not be used for 8-12 days after mifepristone administration, as NSAIDs may reduce its therapeutic effect.
When taken simultaneously with corticosteroids, the risk of ulcers and bleeding from the gastrointestinal tract increases.
Pharmacodynamics
Pharmacodynamics
Etodolac is a non-steroidal anti-inflammatory drug (NSAID), a derivative of indoleacetic acid, which differs from other NSAIDs by the presence of a tetrahydropyranoindole core. Etodolac has anti-inflammatory, analgesic and antipyretic properties. The drug reduces the synthesis of prostaglandins from arachidonic acid by inhibiting the enzyme cyclooxygenase (COX), thereby reducing the sensitivity of receptors to pain mediators (histamine, bradykinin), reducing exudation, leukocyte migration, and the sensitivity of the hypothalamic thermoregulatory centers to the action of endogenous pyrogens (interleukin-1, etc.). Etodolac has moderate selectivity for COX-2, so it acts primarily at the site of inflammation.
Overdose
Overdose
Symptoms: nausea, vomiting, epigastric pain, gastrointestinal bleeding, hypernatremia, hyperkalemia, edema, increased blood pressure, allergic interstitial nephritis, jaundice, hepatitis, bronchospasm.
Treatment: there is no specific antidote; in case of drug overdose, gastric lavage, activated charcoal (within the next hour), symptomatic therapy should be performed
Other forms…
Related products
Buy Nobedolak 400 mg 14 pcs with delivery to USA, UK, Europe and over 120 other countries.