No products in the cart.
Neurontin, capsules 300 mg 50 pcs
€31.34 €26.12
Description
Gabapentin is structurally similar to GABA, but its mechanism of action differs from some other similar drugs that interact with GABA receptors, including valproate, barbiturates, benzodiazepines, GABA transaminase inhibitors, GABA capture inhibitors, GABA agonists and GABA prodrug forms: it has no GABAergic properties and does not affect GABA capture or metabolism. Preliminary studies suggest that gabapentin binds to the α2-δ-subunit of voltage-dependent calcium channels and suppresses calcium ion flux, which plays an important role in the onset of neuropathic pain.
Other mechanisms involved in the action of gabapentin in neuropathic pain are: reduction of glutamate-dependent neuronal death, increase in GABA synthesis, inhibition of monoamine group neurotransmitter release. Gabapentin in clinically relevant concentrations does not bind to receptors of other common drugs or neurotransmitters, including GABAA, GABABAB, benzodiazepine, glutamate, glycine or N-methyl-d-aspartate (NMDA) receptors.
The action of gabapentin is different from phenytoin and carbamazepine: it does not interact with sodium channels in vitro. Gabapentin partially attenuated the effects of NMDA glutamate receptor agonist in some in vitro tests, but only at concentrations greater than 100 µmol, which is not achieved in vivo. Gabapentin slightly reduces monoamine neutrotransmitter release in vitro.
A rat trial showed that administration of gabapentin resulted in increased GABA metabolism in some brain sites; this effect was similar to that of sodium valproate, although observed in other brain sites. The significance of these effects of gabapentin for its anticonvulsant activity has not been established. In animals gabapentin has also been shown to readily penetrate brain tissue and prevent seizures induced by maximal electroshock, chemicals including GABA synthesis inhibitors, and genetic factors.
Pharmacokinetics
Intake
After oral administration, Cmax of gabapentin in plasma is reached after 2-3 hours. The bioavailability of gabapentin is not proportional to the dose; thus, it decreases with increasing dose. Absolute bioavailability of gabapentin in capsules is about 60%. Food, including those with high fat content, has no effect on pharmacokinetics.
The plasma excretion of gabapentin is linear.
Metabolism
There is no evidence of metabolism in humans, The drug does not induce oxidative liver enzymes with mixed function involved in drug metabolism.
Distribution
The pharmacokinetics do not change with repeated administration; equilibrium plasma concentrations can be predicted from a single drug administration. Gabapentin is practically not bound to plasma proteins (less than 3%); Vd is approximately 57.7 L.
The T1/2 from plasma is independent of the dose and averages 5-7 hours.
Extracted exclusively by the kidneys in unchanged form.
Pharmacokinetics in special clinical cases
The clearance of gabapentin from plasma is decreased in elderly people and patients with impaired renal function.
The elimination rate constant, plasma clearance and renal clearance are directly proportional to CK. Gabapentin is eliminated from plasma by hemodialysis.
In patients with impaired renal function and patients receiving hemodialysis treatment, dose adjustment is recommended.
Plasma concentrations of gabapentin in children aged 4 to 12 years have been found to be generally similar to those in adults.
Indications
Indications
Treatment of neuropathic pain in adults aged 18 years and older. Efficacy and safety in patients under 18 years of age have not been established.
Monotherapy for partial seizures with and without secondary generalization in adults and children aged 12 years and older. The effectiveness and safety of monotherapy in children under 12 years of age have not been established.
As an additional remedy in the treatment of partial seizures with and without secondary generalization in adults and children aged 3 years and older. The safety and effectiveness of adjunctive gabapentin therapy in children less than 3 years of age have not been established.
Pharmacological effect
Pharmacological effect
The exact mechanism of action of gabapentin is not known.
The chemical structure of gabapentin is similar to that of the neurotransmitter GABA (gamma-aminobutyric acid), but its mechanism of action differs from other active substances that interact with GABA synapses, such as valproate, barbiturates, benzodiazepines, GABA transaminase inhibitors, GABA reuptake inhibitors, GABA agonists and GABA prodrugs. In vitro studies with radiolabeled gabapentin in the rat brain revealed new regions of drug binding to proteins, including the neocortex and hippocampus, which may be relevant to the anticonvulsant and analgesic activity of gabapentin and its derivatives. It was found that the binding site of gabapentin is the α-2-δ (alpha-2-delta) subunit of voltage-gated calcium channels.
At clinically relevant concentrations, gabapentin does not bind to other common drug and neurotransmitter receptors found in the brain, including GABAA, GABAB, benzodiazepine, glutamate, glycine and N-methyl-d-aspartate receptors.
Gabapentin does not interact with sodium channels in vitro, which distinguishes it from phenytoin and carbamazepine. In a number of in vitro test systems, the use of gabapentin led to a partial decrease in the response to the glutamate agonist N-methyl-D-aspartate (NMDA), but only at concentrations exceeding 100 μmol/L, which is unattainable in in vivo conditions. In vitro, the use of gabapentin leads to a slight decrease in the release of monoamine neurotransmitters. Administration of gabapentin to rats results in an increase in the rate of GABA metabolism in some areas of the brain, similar to the effect of sodium valproate, but the effect is observed in other parts of the brain. The relationship between the reported varied effects of gabapentin and its anticonvulsant activity remains to be established. In animals, gabapentin easily penetrates into brain tissue and prevents seizures provoked by maximal electric shock, chemical convulsants, including GABA synthesis inhibitors, as well as in the case of genetic models of seizure syndromes.
Clinical efficacy and safety
A clinical trial of adjuvant treatment of partial-onset seizures in children aged 3 to 12 years demonstrated a quantitative but non-significant difference in the rate of a 50% reduction in the number of seizures in the gabapentin group compared with the placebo group. Additional analysis of the response rate to therapy depending on age (when considering age as a continuous variable or when distinguishing two age subgroups: 3 – 5 years and 6 – 12 years) did not reveal a statistically significant effect of age on the effectiveness of therapy.
The results of this additional analysis are presented in the table below.
Response (≥50% improvement) by treatment and age, MITT population*
Age group: < 6 years
Placebo: 4/21 (19.0%)
Gabapentin: 4/17 (23.5%)
p value: 0.7362
Age group: 6 – 12 years old
Placebo: 17/99 (17.2%)
Gabapentin: 20/96 (20.8%)
p value: 0.5144
*The modified intention-to-treat (MITT) population was defined as the population of all patients randomized to study treatment and who had evaluable seizure diaries over a 28-day period during the baseline and double-blind phases of the study.
Suction
After oral administration, the maximum concentration of gabapentin in the blood plasma is achieved within 2 to 3 hours. The bioavailability of gabapentin tends to decrease with increasing dosage of the drug. Absolute bioavailability when taking 300 mg capsules is approximately 60%. Food, including food high in fat, does not have a clinically significant effect on the pharmacokinetic parameters of gabapentin.
The pharmacokinetics of gabapentin does not change with repeated administration of the drug. Although gabapentin plasma concentrations typically ranged from 2 mcg/mL to 20 mcg/mL in clinical studies, they did not predict either the efficacy or safety of the drug. Pharmacokinetic parameters are presented in the table.
Table – Summary of average (CV, %) parameters of the pharmacokinetics of gabapentin at steady state during repeated dosing with a dosing interval of eight hours
300 mg (N=7)
Cmax (µg/ml): Average – 4.02, % CV – (24)
tmax (h): Average – 2.7, % CV – (18)
T1/2 (h): Average – 5.2, % CV – (12)
AUC (0-8) (mcg*h/ml): Average – 24.8, % CV – (24)
Ae% (%): Average – No data available, % CV – No data available
400 mg (N=14)
Cmax (µg/ml): Average – 5.74, %CV – (38)
tmax (h): Average – 2.1, % CV – (54)
T1/2 (h): Average – 10.8, % CV – (89)
AUC (0-8) (mcg*h/ml): Average – 34.5, % CV – (34)
Ae% (%): Average – 47.2, % CV – (25)
800 mg (N=14)
Cmax (µg/ml): Average – 8.71, % CV – (29)
tmax (h): Average – 1.6, % CV – (76)
T1/2 (h): Average – 10.6, % CV – (41)
AUC (0-8) (µg*h/ml): Average – 51.4, % CV – (27)
Ae% (%): Average – 34.4, % CV – (37)
Cmax is the maximum concentration in blood plasma in a state of stable equilibrium.
tmax – time to reach Cmax.
T1/2 – half-life.
AUC(0-8) is the area under the plasma concentration versus time curve at steady state in the period from 0 to 8 hours after taking the drug.
Ae% – the proportion of the drug eliminated in the urine unchanged during the period from 0 to 8 hours after taking the drug, as a percentage of the dose taken.
Distribution
Gabapentin does not bind to plasma proteins and its volume of distribution is 57.7 L. In patients with epilepsy, the concentration of gabapentin in the cerebrospinal fluid (CSF) is approximately 20% of the minimum steady-state plasma concentration. Gabapentin is excreted into breast milk.
Biotransformation
There are no data on the metabolism of gabapentin in humans. Gabapentin does not induce nonspecific liver oxidases responsible for drug metabolism.
Removal
Gabapentin is eliminated unchanged exclusively by renal excretion. The half-life of gabapentin does not depend on the dose taken and averages from 5 to 7 hours.
In elderly people and patients with impaired renal function, the clearance of gabapentin from blood plasma is reduced. The elimination constant, plasma clearance and renal clearance of gabapentin are directly proportional to creatinine clearance.
Gabapentin is removed from blood plasma during hemodialysis. For patients with impaired renal function or those on hemodialysis, a dose adjustment of the drug is recommended (see section “Method of administration and dosage”).
The pharmacokinetics of gabapentin in children was studied in 50 healthy volunteers aged 1 month to 12 years. In general, the concentration of gabapentin in the blood plasma of children over 5 years of age is similar to that in adults when using the drug in an equivalent dose based on the calculation of mg/kg body weight.
In a pharmacokinetic study in 24 healthy children 1 to 48 months of age, drug exposure (AUC) was approximately 30% lower, Cmax was lower, and clearance per unit body weight was higher compared to available published drug kinetic data in children over 5 years of age.
Linearity/nonlinearity of pharmacokinetic parameters
The bioavailability of gabapentin decreases with increasing dose, which entails non-linearity of pharmacokinetic parameters, which include the bioavailability index (F) in the calculation, for example Ae%, CL/F, Vd/F. Elimination pharmacokinetics (non-F parameter parameters such as CLr and T1/2) are better described by a linear model. Steady-state plasma concentrations of gabapentin are predictable based on single-dose kinetic data.
Special instructions
Special instructions
Suicidal ideation and behavior
Antiepileptic drugs, including gabapentin, may increase the risk of suicidal thoughts or behavior. A meta-analysis of randomized placebo-controlled trials of antiepileptic drugs demonstrated a small increase in the risk of suicidal ideation and behavior. The mechanism for increasing the risk of developing suicidal ideation is unknown, but for gabapentin it cannot be excluded.
Therefore, patients receiving these drugs should be closely monitored for new or worsening depression, the emergence of suicidal thoughts or behavior, and any changes in behavior. Patients or their caregivers should seek medical attention if signs of suicidal thoughts or behavior occur.
Acute pancreatitis
If acute pancreatitis develops while taking gabapentin, the possibility of discontinuing the drug should be assessed.
Convulsions (withdrawal syndrome)
Although withdrawal syndrome accompanied by the development of seizures has not been observed during treatment with gabapentin, abrupt cessation of anticonvulsant drug therapy in patients with epilepsy may provoke the development of status epilepticus (see section “Dosage and Administration”).
As with other antiepileptic drugs, gabapentin may cause an increase in the frequency of seizures or the appearance of a different type of seizure.
As with other anticonvulsants, attempts to discontinue all concomitant antiepileptic drugs in order to initiate gabapentin monotherapy in cases of treatment refractory in patients taking multiple anticonvulsants are generally unsuccessful.
Gabapentin is not thought to be effective for primary generalized seizures, such as absence seizures, and may even worsen such seizures in some patients. In this regard, gabapentin should be used with caution in patients with mixed seizures, including absence seizures.
Elderly patients
Systematic studies have not been conducted in patients aged 65 years and older taking gabapentin. In a double-blind study of gabapentin for neuropathic pain, patients aged 65 years and older had a higher incidence of somnolence, peripheral edema, and asthenia compared with patients aged <65 years. Apart from these results, clinical examination of this group of patients showed that their side effect profile did not differ from the rest.
Children
The effect of long-term therapy (more than 36 weeks) with gabapentin on the learning ability, intelligence and development of the child has not been sufficiently studied. The ratio of possible risks and benefits when prescribing long-term therapy should be assessed.
Abuse and addiction
The post-marketing surveillance database contains reports of cases of drug abuse and dependence. As with any drug that affects the central nervous system, clinicians should carefully review patients’ drug abuse history and monitor patients for possible signs of gabapentin abuse (eg, drug seeking, development of resistance to gabapentin therapy, inappropriate dosage increases).
DRESS syndrome
Severe life-threatening hypersensitivity reactions, such as drug rash with associated eosinophilia and systemic symptoms, have been reported while taking antiepileptic drugs, including gabapentin. It must be remembered that early signs of a hypersensitivity reaction, such as fever, lymphadenopathy, can develop even in the absence of a skin rash. If such symptoms occur, immediate examination of the patient is necessary. If no other reason is found other than the use of gabapentin, the use of the drug should be discontinued.
Anaphylaxis
Taking gabapentin can lead to the development of anaphylaxis. The following symptoms and signs were noted in cases of anaphylaxis while taking gabapentin – difficulty breathing, swelling of the lips, throat and tongue, and a marked decrease in blood pressure was also noted, requiring urgent medical intervention. Patients should be warned that if signs or symptoms of anaphylaxis develop, they should stop taking the drug and seek medical attention.
Laboratory tests
False-positive results have been reported when gabapentin and other anticonvulsants were used concomitantly with Ames N-Multistix SG® urinary protein test strips. To determine protein in urine, it is recommended to use the more specific method of precipitation with sulfosalicylic acid.
Effect on the central nervous system
During treatment with gabapentin, cases of dizziness and drowsiness have been observed, which may increase the likelihood of accidental injury (from a fall). Cases of confusion, loss of consciousness and mental impairment have also been reported during the post-marketing period. Therefore, patients should be advised to use caution until they know the possible effects of this drug.
Concomitant use of opioid analgesics and other drugs that depress the central nervous system. When used simultaneously with opioid analgesics, an increase in
gabapentin concentrations in blood plasma. Therefore, patients who require concomitant therapy with CNS depressant drugs, including opioid analgesics, should be closely monitored for signs of CNS depression, such as somnolence, sedation, and respiratory depression. Doses of gabapentin or concomitantly used CNS depressants, including opioid analgesics, should be reduced accordingly (see Interactions with Other Drugs).
Caution should be exercised when prescribing gabapentin concomitantly with opioids due to the risk of CNS depression. In a population-based observational study using a control group in patients taking opioids, concomitant use of opioids and gabapentin was associated with an increased risk of opioid-related deaths compared with use of opioids alone (adjusted odds ratio [aOR], 1.49 [95% CI, 1.18 to 1.88, p < 0.001]).
Combined use with antacids
Gabapentin is recommended to be taken approximately 2 hours after taking the antacid.
Active ingredient
Active ingredient
Gabapentin
Composition
Composition
Active ingredient: gabapentin – 300 mg;
Excipients: lactose monohydrate – 42.75 mg, corn starch – 30.00 mg, talc – 30.00 mg; capsule shell: gelatin – 64.07 mg, water – 11.02 mg, titanium dioxide (E 171) – 0.76 mg, iron dye yellow oxide (E 172) – 0.15 mg, sodium lauryl sulfate – less than 0.15 mg; ink: shellac – 0.075 mg, titanium dioxide (E 171) – 0.027 mg, indigo carmine – 0.021 mg.
Pregnancy
Pregnancy
General risk due to epilepsy and antiepileptic drugs
The risk of having children with congenital anomalies in mothers who are treated with anticonvulsants increases 2-3 times. Most often, cleft lip and palate, malformations of the cardiovascular system and neural tube defects are observed. However, taking multiple anticonvulsants may be associated with a greater risk of malformations than in the case of monotherapy. Therefore, if possible, one of the anticonvulsants should be used. Women of childbearing age, and all women who may become pregnant, should seek advice from a qualified healthcare professional. If a woman is planning a pregnancy, the need to continue anticonvulsant therapy should be re-evaluated. However, anticonvulsant drugs should not be discontinued abruptly, as this can lead to resumption of seizures with serious consequences for the mother and child. In rare cases, developmental delays have been observed in children whose mothers have epilepsy. However, it is impossible to determine whether developmental delay is due to genetic or social factors, maternal illness or anticonvulsant therapy.
Risk associated with gabapentin
Gabapentin crosses the placenta. Congenital malformations and adverse pregnancy outcomes have been reported with the use of gabapentin, however, there are no adequate controlled studies of the drug in pregnant women, and no definitive conclusion can be drawn regarding the association of gabapentin with an increased risk of congenital anomalies or other adverse developmental outcomes when used during pregnancy. The risk of developing congenital anomalies increases 2-3 times in the offspring of women treated with antiepileptic drugs. Experiments on animals showed the toxicity of the drug to the fetus. People have no data regarding the possible risk. Therefore, gabapentin should be used during pregnancy only if the expected benefit to the mother justifies the possible risk to the fetus.
In the cases that have been reported, it is impossible to say with certainty whether or not the use of gabapentin during pregnancy is accompanied by an increased risk of malformations, firstly, due to the presence of epilepsy itself, and secondly, due to the use of other anticonvulsants.
Breastfeeding
Gabapentin is excreted in breast milk and its effect on the nursing infant is unknown, so Neurontin should only be prescribed during breastfeeding if the benefit to the mother clearly outweighs the risk to the infant.
There was no effect of gabapentin on fertility in animal studies.
Contraindications
Contraindications
Hypersensitivity to gabapentin or auxiliary components of the drug.
Epilepsy
Use as monotherapy for partial seizures with and without secondary generalization in children under 12 years of age.
Use as an additional agent in the treatment of partial seizures with and without secondary generalization in children under 3 years of age.
Neuropathic pain
For the treatment of neuropathic pain in children and adolescents under 18 years of age.
Lactase deficiency, lactose intolerance, glucose-galactose malabsorption.
Side Effects
Side Effects
Adverse effects observed in clinical studies in patients with epilepsy (when using gabapentin as monotherapy or in combination with other anticonvulsants) or neuropathic pain are presented below and categorized by organ system and frequency. The frequency category was defined as follows: very often (≥1/10); often (from ≥1/100 to <1/10); uncommon (from ≥1/1000 to <1/100); rare (from ≥1/10000 to <1/1000); very rare (<1/10000). If the frequency category was different between studies, the side effect was assigned a higher category.
Side effects reported during the use of the drug after registration were assigned a frequency category of “unknown” (frequency cannot be calculated based on available data).
In each frequency section, side effects are presented in order of decreasing severity.
Infectious and parasitic diseases: very often – viral infections; often – pneumonia, respiratory tract infection, urinary tract infection, other types of infection, otitis media.
Disorders of the blood and lymphatic system: often – leukopenia; unknown – thrombocytopenia.
Immune system disorders: uncommon – allergic reactions, including urticaria; unknown – hypersensitivity, including systemic reactions such as fever, rash, hepatitis, lymphadenopathy, eosinophilia and others.
Metabolic and nutritional disorders: often – anorexia, increased appetite.
Mental disorders: often – hostility, confusion, depression, anxiety, nervousness, impaired thinking, emotional lability; infrequently – deterioration of mental state; unknown – hallucinations.
Nervous system disorders: very often – drowsiness, dizziness, ataxia; often – convulsions, hyperkinesia, dysarthria, amnesia, tremor, insomnia, headache, sensory disturbances (for example, paresthesia, hypesthesia), loss of coordination, nystagmus, strengthening, weakening or absence of reflexes; infrequently – hypokinesia; rarely – loss of consciousness, unknown – other movement disorders (for example, choreoathetosis, dyskinesia and dystonia).
Visual disorders: often – visual impairment (such as amblyopia, diplopia).
Hearing disorders and labyrinthine disorders: often – vertigo, unknown – tinnitus.
Cardiac disorders: uncommon – palpitations.
Vascular disorders: often – symptoms of vasodilation, arterial hypertension.
Disorders of the respiratory system, chest and mediastinal organs: often – shortness of breath, bronchitis, pharyngitis, cough, rhinitis.
Gastrointestinal disorders: often – constipation, diarrhea, dry mucous membrane of the mouth or pharynx, dyspepsia, flatulence, nausea, vomiting, abdominal pain, dental disease, gingivitis; unknown – pancreatitis.
Disorders of the liver and biliary tract: unknown – hepatitis, jaundice.
Disorders of the skin and subcutaneous tissues: often – swelling of the face, purpura (most often it was described as bruising resulting from physical trauma), skin rash, acne, skin itching; unknown – Stevens-Johnson syndrome, angioedema, anaphylaxis, erythema multiforme, alopecia, drug skin rash, including eosinophilia and systemic reactions (see section “Special instructions”).
Musculoskeletal and connective tissue disorders: often – myalgia, arthralgia, back pain, muscle twitching; unknown – rhabdomyolysis, myoclonus. Renal and urinary tract disorders: unknown – urinary incontinence, acute renal failure.
Disorders of the genital organs and mammary gland: often – impotence, unknown – enlargement of the mammary glands, gynecomastia, sexual dysfunction (including changes in libido, ejaculation disorders and anorgasmia).
General disorders and disorders at the injection site: very often – fatigue, fever; often – peripheral edema, gait disturbance, asthenia, pain of various localizations, general malaise, flu-like syndrome; infrequently – generalized edema, falls; unknown – withdrawal syndrome (the most frequently reported side effects were anxiety, insomnia, nausea, pain of various localizations and increased sweating), chest pain. There have been cases of sudden unexplained death, the connection of which with gabapentin treatment has not been established.
Laboratory and instrumental data: often – decreased concentration of leukocytes, increased body weight; infrequently – increased activity of alanine aminotransferase, aspartate aminotransferase and bilirubin concentration in the blood plasma, hyperglycemia; rarely – hypoglycemia (mainly in patients with diabetes mellitus); unknown – hyponatremia, increased creatine phosphokinase activity.
Injuries, intoxications and complications of manipulations: often – injuries, fractures, abrasions associated with falls.
There are reports of the development of acute pancreatitis during therapy with gabapentin.
The causal relationship with gabapentin remains unclear (see section “Special instructions”).
There have been case reports of myopathy with increased creatine kinase activity in patients with end-stage renal disease undergoing hemodialysis.
Cases of respiratory tract infection, otitis media, bronchitis and seizures were reported only in clinical studies. In addition, clinical studies have reported cases of aggressive behavior and hyperkinesis in children.
Interaction
Interaction
There have been spontaneous case reports and literature reports of possible respiratory depression, symptoms of sedation, and death associated with gabapentin when coadministered with CNS depressants, including opioid analgesics. In some of these cases, the authors considered that the concomitant use of gabapentin with opioids is a particular problem in frail patients, in elderly patients, in patients with serious underlying respiratory conditions, in patients who are prescribed multiple medications at the same time, and in patients who abuse substances.
When gabapentin 600 mg was administered 2 hours after administration of morphine 60 mg extended-release capsules, there was a 44% increase in mean gabapentin AUC compared to gabapentin monotherapy, which was associated with an increase in pain threshold (cold pressor test). The clinical significance of this change has not been established; the pharmacokinetic characteristics of morphine did not change. The side effects of morphine when taken together with gabapentin did not differ from those when morphine was taken together with placebo. The extent to which these drugs interact at other doses is unknown.
No interactions were observed between gabapentin and phenobarbital, phenytoin, valproic acid and carbamazepine. The pharmacokinetics of gabapentin at steady state are similar in healthy subjects and patients receiving other anticonvulsants.
Concomitant use of gabapentin with oral contraceptives containing norethisterone and/or ethinyl estradiol is not accompanied by changes in the pharmacokinetics of both components.
The simultaneous use of gabapentin with antacids containing aluminum and magnesium is accompanied by a decrease in the bioavailability of gabapentin by approximately 24% (see section “Special instructions”).
Probenecid does not affect the renal excretion of gabapentin.
The small decrease (14%) in renal excretion of gabapentin with concomitant use of cimetidine is probably not clinically significant.
With simultaneous use of naproxen (250 mg) and gabapentin (125 mg), an increase in gabapentin absorption from 12% to 15% was observed. Gabapentin has no effect on the pharmacokinetic parameters of naproxen. The indicated doses of drugs are less than the minimum therapeutic ones. The simultaneous use of these drugs in large doses has not been studied.
Overdose
Overdose
With a single dose of 49 g of gabapentin, the following symptoms were observed: dizziness, double vision, speech impairment, drowsiness, loss of consciousness, lethargy and mild diarrhea, which completely disappeared with symptomatic therapy.
It should be taken into account that after taking high doses of gabapentin, its absorption in the intestine decreases.
In case of an overdose of gabapentin, coma may develop, especially with the simultaneous use of other drugs that suppress the central nervous system.
Although gabapentin can be eliminated by hemodialysis, current experience shows that this is not usually necessary. Hemodialysis may be indicated for patients with severe renal impairment.
In experiments on mice and rats, to which the drug was administered in doses of up to 8000 mg/kg, it was not possible to establish the lethal dose of gabapentin when administered orally. Signs of acute toxicity in animals included ataxia, difficulty breathing, ptosis, hypoactivity or agitation.
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C.
Keep out of the reach of children.
Shelf life
Shelf life
3 years.
Do not use after the expiration date.
Manufacturer
Manufacturer
USA
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | The drug should be kept out of reach of children, at a temperature not exceeding 25°C |
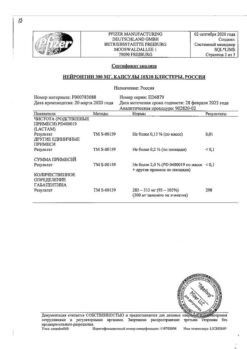
| Manufacturer | Pfizer, Puerto Rico |
| Medication form | capsules |
| Brand | Pfizer |
Other forms…
Related products
Buy Neurontin, capsules 300 mg 50 pcs with delivery to USA, UK, Europe and over 120 other countries.