No products in the cart.
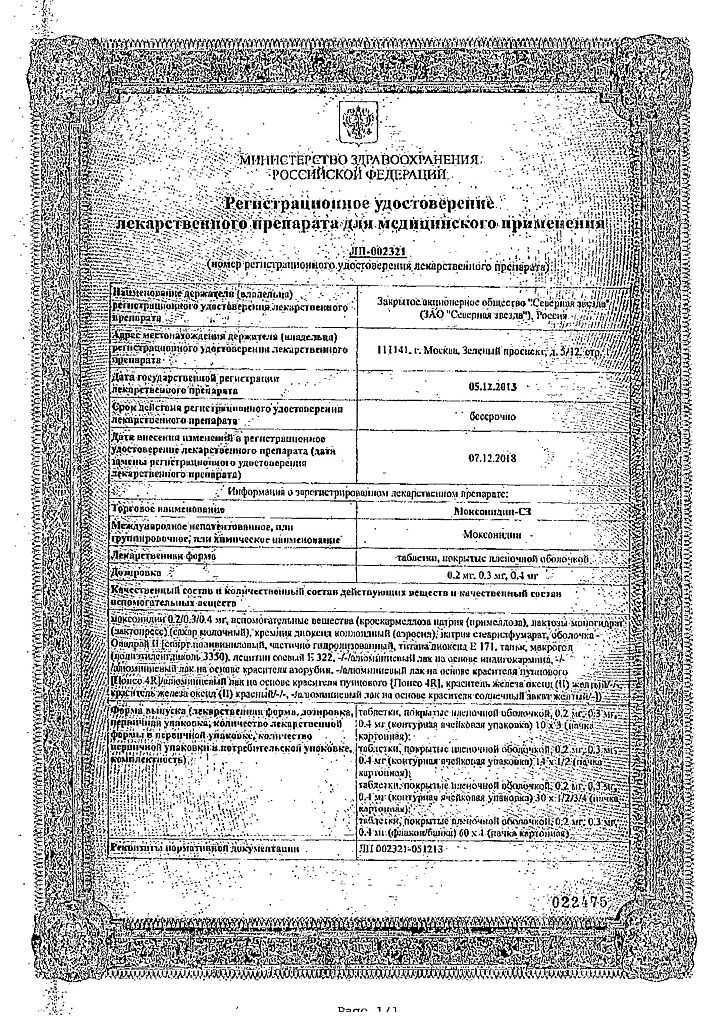
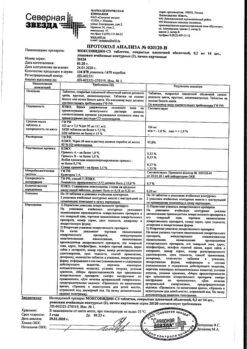
Moxonidine-SZ, 0.4 mg 28 pcs
€8.15 €7.13
Description
Pharmacotherapeutic drug group:
Hypotensive drug of central action.
ATC code: [C02AC05]
Pharmacodynamics
Moxonidine is a hypotensive drug with a central mechanism of action. In brain stem structures (rostral layer of lateral ventricles) moxonidine selectively stimulates imidazoline-sensitive receptors involved in tonic and reflex regulation of sympathetic nervous system. Stimulation of imidazoline receptors reduces peripheral sympathetic activity and blood pressure (BP).
Moxonidine differs from other sympatholytic hypotensive agents in its lower affinity for α2-adrenoreceptors, which explains the lower probability of developing sedation and dry mouth. Administration of moxonidine results in reduction of systemic vascular resistance and BP. Moxonidine improves insulin sensitivity index (compared to placebo) by 21 % in patients with obesity, insulin resistance and moderate arterial hypertension. Pharmacokinetics
Intake:
After oral administration, moxonidine is rapidly and almost completely absorbed in the upper gastrointestinal tract. Absolute bioavailability is approximately 88%. Time of reaching maximum concentration is; about 1 hour. Food intake has no effect on the pharmacokinetics of the drug.
Distribution
The binding to plasma proteins is 7.2%.
Metabolism
The main metabolite is; dehydrated moxonidine. The pharmacodynamic activity of dehydrated moxonidine is; about 10% compared to moxonidine. Excretion The elimination half-life (T1/2) of moxonidine and the metabolite is 2.5 and 5 hours, respectively. Within 24 hours, over 90% of moxonidine is excreted by the kidneys (approximately 78% unchanged and 13% as dehydro-romoxonidine, other metabolites in the urine do not exceed 8% of the dose taken). Less than 1% of the dose is excreted through the intestine.
Pharmacokinetics in patients with arterial hypertension: Compared with healthy volunteers, patients with arterial hypertension show no changes in the pharmacokinetics of moxonidine.
Pharmacokinetics in the elderly
Clinically insignificant changes in the pharmacokinetic parameters of moxonidine have been observed in elderly patients, probably due to a decrease in its metabolic rate and/or slightly higher bioavailability.
Pharmacokinetics in children
Moxonidine is not recommended for use in patients younger than 18 years of age; therefore, no pharmacokinetic studies have been performed in this group. Pharmacokinetics in renal failure
The excretion of moxonidine is highly correlated with creatinine clearance (CK). In patients with moderate renal insufficiency (CK between 30-60 mL/min), equilibrium plasma concentrations and final T1/2 are approximately 2 and l.5 times higher than in patients with normal renal function (CK greater than 90 mL/min).
In patients with severe renal impairment (CKR less than 30 mL/min), equilibrium plasma concentrations and final T1/2 are 3 times higher than in patients with normal renal function. Administration of multiple doses of moxonidine results in predictable cumulation in patients with moderate to severe renal impairment.
In patients with terminal renal failure (KC less than 10 ml/min) on hemodialysis, equilibrium plasma concentrations and final T1/2 are 6 and 4 times higher, respectively, than in patients with normal renal function. In all groups, the maximum plasma concentration of moxonidine is 1.5 to 2 times higher. In patients with impaired renal function the dosage should be adjusted individually. Moxonidine is slightly excreted during hemodialysis.
Indications
Indications
Arterial hypertension.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group of the drug:
Centrally acting antihypertensive agent.
ATX code: [C02AC05]
Pharmacodynamics
Moxonidine is an antihypertensive drug with a central mechanism of action. In the brain stem structures (rostral layer of the lateral ventricles), moxonidine selectively stimulates imidazoline-sensitive receptors that take part in the tonic and reflex regulation of the sympathetic nervous system. Stimulation of imidazoline receptors reduces peripheral sympathetic activity and blood pressure (BP).
Moxonidine differs from other sympatholytic antihypertensive drugs in its lower affinity for α2-adrenergic receptors, which explains the lower likelihood of developing sedation and dry mouth. Taking moxonidine leads to a decrease in systemic vascular resistance and blood pressure. Moxonidine improves the insulin sensitivity index by 21% (compared to placebo) in patients with obesity, insulin resistance and moderate hypertension. Pharmacokinetics
Suction:
After oral administration, moxonidine is rapidly and almost completely absorbed from the upper gastrointestinal tract. Absolute bioavailability is approximately 88%. Time to reach maximum concentration -; about 1 hour. Food intake does not affect the pharmacokinetics of the drug.
Distribution
The connection with blood plasma proteins is 7.2%.
Metabolism
The main metabolite is; dehydrogenated moxonidine. Pharmacodynamic activity of dehydrogenated moxonidine -; about 10% compared to moxonidine. Elimination The half-life (T1/2) of moxonidine and metabolite is 2.5 and 5 hours, respectively. Within 24 hours, over 90% of moxonidine is excreted by the kidneys (about 78% unchanged and 13% as dehydriroxonidine, other metabolites in the urine do not exceed 8% of the dose taken). Less than 1% of the dose is excreted through the intestines.
Pharmacokinetics in patients with arterial hypertension: Compared with healthy volunteers, patients with arterial hypertension do not show changes in the pharmacokinetics of moxonidine.
Pharmacokinetics in old age
Clinically insignificant changes in the pharmacokinetic parameters of moxonidine were noted in elderly patients, probably due to a decrease in the intensity of its metabolism and/or slightly higher bioavailability.
Pharmacokinetics in children
Moxonidine is not recommended for use in patients under 18 years of age, and therefore pharmacokinetic studies have not been conducted in this group. Pharmacokinetics in renal failure
Moxonidine excretion is significantly correlated with creatinine clearance (CC). In patients with moderate renal failure (creatinine clearance in the range of 30-60 ml/min.), steady-state plasma concentrations and final T1/2 are approximately 2 and l.5 times higher than in patients with normal renal function (creatinine clearance more than 90 ml/min.).
In patients with severe renal failure (creatinine clearance less than 30 ml/min.), steady-state plasma concentrations and final T1/2 are 3 times higher than in patients with normal renal function. The administration of multiple doses of moxonidine leads to predictable accumulation in the body of patients with moderate and severe renal failure.
In patients with end-stage renal failure (creatinine clearance less than 10 ml/min) on hemodialysis, steady-state plasma concentrations and final T1/2 are 6 and 4 times higher, respectively, than in patients with normal renal function. In all groups, the maximum concentration of moxonidine in blood plasma was 1.5 – 2 times higher. In patients with impaired renal function, the dosage should be adjusted individually. Moxonidine is excreted to a small extent during hemodialysis.
Special instructions
Special instructions
If it is necessary to cancel beta-blockers and the drug Moxonidine taken simultaneously, first cancel the beta-blockers and only after a few days Moxonidine. There is currently no evidence that stopping Moxonidine leads to an increase in blood pressure. However, it is not recommended to stop taking Moxonidine suddenly; instead, you should gradually reduce the dose of the drug over two weeks. Avoid drinking alcohol during treatment. During treatment, regular monitoring of heart rate and electrocardiography is necessary.
Impact on the ability to drive vehicles and operate machinery
The effect of Moxonidine on the ability to drive vehicles or operate machinery has not been studied. However, taking into account the possibility of dizziness and drowsiness, patients should be careful when engaging in potentially hazardous activities that require increased attention, such as driving a vehicle or operating equipment that requires increased concentration.
Active ingredient
Active ingredient
Moxonidine
Composition
Composition
Active substance:
moxonidine 0.4 mg
excipients (core):
croscarmellose sodium (primellose) -3.0 mg;
lactose monohydrate (lactopress) (milk sugar) – 95.1 mg;
colloidal silicon dioxide (Aerosil) – 0.5 mg;
sodium stearyl fumarate – 1.0 mg;
excipients (shell):
Pregnancy
Pregnancy
Pregnancy
There are no clinical data on the use of Moxonidine in pregnant women.
In animal studies, the embryotoxic effect of the drug was established. Moxonidine should be prescribed to pregnant women only after a careful assessment of the risk-benefit ratio, when the benefit to the mother outweighs the potential risk to the fetus.
Lactation period
Moxonidine passes into breast milk and should therefore not be given during breastfeeding. If it is necessary to use Moxonidine during lactation, breastfeeding should be stopped.
Contraindications
Contraindications
Severe renal failure (creatinine clearance less than 30 ml/min);
severe heart rhythm disturbances;
SSSU;
severe bradycardia (resting heart rate less than 50 beats/min);
AV block II and III degrees;
acute and chronic heart failure (III-IV functional class according to the NYHA classification);
simultaneous use with tricyclic antidepressants;
hemodialysis;
lactation period;
age over 75 years;
age under 18 years (due to lack of data on safety and effectiveness);
hereditary lactose intolerance, lactase deficiency or glucose-galactose malabsorption;
hypersensitivity to the active substance and other components of the drug.
With caution
Particular caution must be exercised when using moxonidine in patients with first degree AV block (risk of developing bradycardia); severe coronary artery disease, severe coronary artery disease or unstable angina (insufficient experience with use), chronic heart failure, severe liver failure, impaired renal function (creatinine clearance more than 30 ml/min).
Side Effects
Side Effects
The frequency of side effects listed below was determined according to the following: very often (>1/10); often (>1/100.1/1000,
From the central nervous system: Often: headache*, dizziness (vertigo), drowsiness. Uncommon: fainting*.
From the cardiovascular system: Uncommon: marked decrease in blood pressure, orthostatic hypotension*, bradycardia.
From the gastrointestinal tract: Very often: dryness of the oral mucosa. Common: diarrhea, nausea, vomiting, dyspepsia.
From the skin and subcutaneous tissues: Often: skin rash, itching. Uncommon: angioedema. Mental disorders: Often: insomnia. Uncommon: nervousness.
Hearing and labyrinthine disorders: Uncommon: tinnitus.
Musculoskeletal and connective tissue disorders: Common: back pain. Uncommon: neck pain. General disorders and disorders at the injection site: Common: asthenia. Uncommon: peripheral edema. (* – frequency comparable to placebo).
Interaction
Interaction
The combined use of moxonidine with other antihypertensive drugs leads to an additive effect. Tricyclic antidepressants may reduce the effectiveness of centrally acting antihypertensive drugs, and therefore their use together with moxonidine is not recommended.
Moxonidine may enhance the effect of tricyclic antidepressants, tranquilizers, ethanol, sedatives and hypnotics.
Moxonidine may moderately improve impaired cognitive function in patients receiving lorazepam.
Moxonidine may enhance the sedative effect of benzodiazepine derivatives when administered simultaneously.
Moxonidine is released by tubular secretion. Therefore, its interaction with other drugs released by tubular secretion is not excluded. Beta-blockers increase bradycardia and the severity of negative ino- and dromotropic effects.
Overdose
Overdose
There have been reports of several cases of non-fatal overdose when doses up to 19.6 mg were used simultaneously.
Symptoms: headache, sedation, marked decrease in blood pressure, dizziness, asthenia, bradycardia, dry oral mucosa, vomiting, fatigue, pain in the epigastric region, respiratory depression and impaired consciousness. In addition, short-term increases in blood pressure, tachycardia and hyperglycemia are also possible, as shown in several high-dose animal studies.
Treatment
There is no specific antidote. In the case of a pronounced decrease in blood pressure, it may be necessary to restore the volume of circulating blood by introducing fluid and dopamine (injection). Bradycardia can be stopped with atropine (injection).
In severe cases of overdose, it is recommended to carefully monitor disturbances of consciousness and avoid respiratory depression. Alpha-adrenergic antagonists may reduce or eliminate the paradoxical hypertensive effects of moxonidine overdose. Moxonidine is excreted to a small extent during hemodialysis.
Storage conditions
Storage conditions
In a dry place, protected from light, at a temperature not exceeding 25 ° C. Keep out of the reach of children.
Shelf life
Shelf life
3 years. Do not use after the expiration date stated on the package.
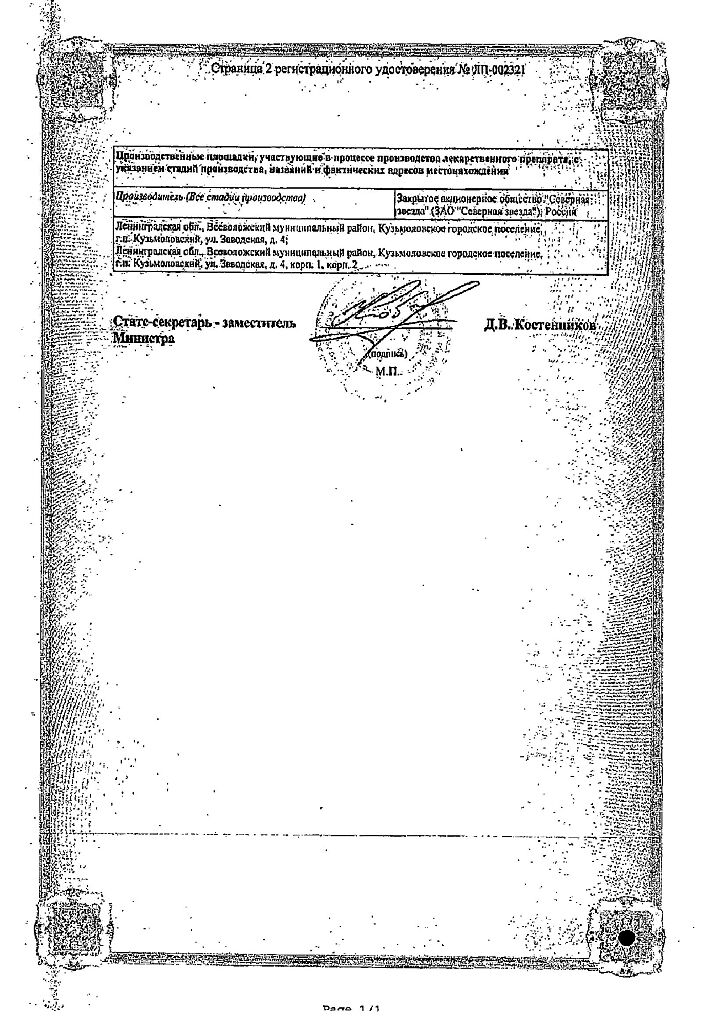
Manufacturer
Manufacturer
North Star NAO, Russia
Additional information
| Shelf life | 3 years. Do not use after the expiration date printed on the package. |
|---|---|
| Conditions of storage | In a dry, light-protected place at a temperature not exceeding 25 oC. Keep out of reach of children. |
| Manufacturer | North Star NAO, Russia |
| Medication form | pills |
| Brand | North Star NAO |
Other forms…
Related products
Buy Moxonidine-SZ, 0.4 mg 28 pcs with delivery to USA, UK, Europe and over 120 other countries.