No products in the cart.
Description
GCS of intranasal application.
It has anti-inflammatory and anti-allergic effect.
The mechanism of anti-allergic and anti-inflammatory action is due to the ability to inhibit the release of inflammatory mediators. It increases production of lipomodulin, which is an inhibitor of phospholipase A, thus reducing the release of arachidonic acid, and, accordingly, inhibiting the synthesis of products of arachidonic acid metabolism – cyclic endoperoxides, prostaglandins.
It prevents marginal accumulation of neutrophils that reduces inflammatory exudate and lymphokine production, inhibits macrophage migration, results in a decrease of infiltration and granulation processes.
In vitro reduces inflammation due to a decrease in chemotaxis substance formation (effect on late allergic reactions), inhibits the development of immediate allergic reactions (caused by inhibition of arachidonic acid metabolites production and decrease of inflammatory mediators release from mast cells).
In vitro mometasone furoate significantly inhibits the release of leukotrienes from leukocytes. In cell cultures, mometasone furoate has demonstrated a high ability to inhibit the synthesis and release of IL-1,IL-5, IL-6, and TNFα; it is also an inhibitor of leukotriene production and is an extremely potent inhibitor of Th2 cytokines, IL-4 and IL-5, by human CD4+ T-cells.
In studies in preclinical models, mometasone reduced inflammatory cell accumulation (including eosinophils), infiltrated the walls of the upper and lower airways, and improved lung function after a provocation test. Mometazone reduced lymphocyte counts and mRNA concentrations of cytokines IL-4 and IL-5.
In studies with nasal mucosa antigen provocation tests, high anti-inflammatory activity of Mometazone was demonstrated in both the early and late stages of an allergic reaction.
This was confirmed by a decrease (compared with placebo) in histamine levels and eosinophil activity, as well as a decrease (compared with baseline) in eosinophils, neutrophils and epithelial cell adhesion proteins.
Pharmacokinetics.
After intranasal administration, the systemic bioavailability of mometasone is low, particularly because of the low absorption and significant presystemic metabolism upon ingestion of mometasone.
When used at the recommended doses, the plasma concentration of mometasone is near or below the threshold of determination (50 pg/mL). As a consequence, neither the T1/2 nor the Vd of mometasone after inhalation can be determined. It is excreted in the urine and bile.
Indications
Indications
For intranasal use:
treatment of seasonal and year-round allergic rhinitis in adults, adolescents and children over 2 years of age;
acute sinusitis or exacerbation of chronic sinusitis in adults (including the elderly) and adolescents over 12 years of age (as an auxiliary therapeutic agent in antibiotic treatment);
acute rhinosinusitis with mild to moderate symptoms without signs of severe bacterial infection in patients aged 12 years and older;
prevention of seasonal allergic rhinitis of moderate and severe course in adults and adolescents from 12 years of age;
nasal polyposis, accompanied by impaired nasal breathing and sense of smell in adults.
Pharmacological effect
Pharmacological effect
GCS for intranasal use.
Has anti-inflammatory and anti-allergic effects.
The mechanism of antiallergic and anti-inflammatory action is due to the ability to inhibit the release of inflammatory mediators. Increases the production of lipomodulin, which is an inhibitor of phospholipase A, which causes a decrease in the release of arachidonic acid and, accordingly, inhibition of the synthesis of arachidonic acid metabolic products – cyclic endoperoxides, prostaglandins.
Prevents the marginal accumulation of neutrophils, which reduces inflammatory exudate and the production of lymphokines, inhibits the migration of macrophages, and leads to a decrease in the processes of infiltration and granulation.
Reduces inflammation by reducing the formation of a chemotaxis substance (impact on late allergy reactions), inhibits the development of an immediate allergic reaction (due to inhibition of the production of arachidonic acid metabolites and a decrease in the release of inflammatory mediators from mast cells).
In vitro, mometasone furoate significantly inhibits the release of leukotrienes from leukocytes. In cell cultures, mometasone furoate demonstrated a high ability to inhibit the synthesis and release of IL-1, IL-5, IL-6, as well as TNFα; it is also an inhibitor of leukotriene production, as well as an extremely potent inhibitor of Th2 cytokines, IL-4 and IL-5, by human CD4+ T cells.
When studied in preclinical models, mometasone reduced the accumulation of inflammatory cells (including eosinophils), penetrated into the walls of the upper and lower respiratory tract, and also improved lung function after a challenge test. Mometasone reduced the number of lymphocytes and the concentration of mRNA for the cytokines IL-4 and IL-5.
In studies with provocative tests with the application of antigens to the nasal mucosa, the high anti-inflammatory activity of mometasone was demonstrated, both in the early and late stages of the allergic reaction.
This was confirmed by a decrease (compared to placebo) in histamine levels and eosinophil activity, as well as a decrease (compared to baseline) in the number of eosinophils, neutrophils and epithelial cell adhesion proteins.
Pharmacokinetics.
After intranasal administration, the systemic bioavailability of mometasone is low, in part due to poor absorption and significant first-pass metabolism when mometasone is swallowed.
When used in recommended doses, the plasma concentration of mometasone is near or below the detection threshold (50 pg/ml). As a result, it is impossible to determine either T1/2 or Vd of mometasone after inhalation. Excreted in urine and bile.
Special instructions
Special instructions
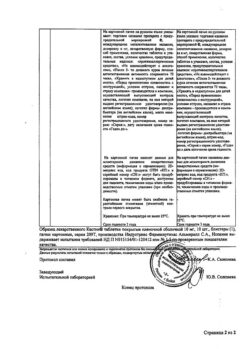
Mometasone should be used with caution in case of tuberculosis infection (active or latent) of the respiratory tract, untreated fungal, bacterial, systemic viral infection or infection caused by Herpes simplex with eye damage (as an exception, the drug can be prescribed for these infections as directed by a doctor), the presence of an untreated local infection involving the mucous membrane of the nasal cavity.
With long-term intranasal use of mometasone, periodic examination of the nasal mucosa by an ENT doctor is necessary. If a local bacterial or fungal infection of the nose or throat develops, it is recommended to stop treatment and begin special treatment.
Irritation of the mucous membrane of the nasal cavity and pharynx that persists for a long time is an indication for discontinuation of the drug.
When switching from GCS for systemic use to intranasal use of mometasone, special caution is required due to the possible risk of developing adrenal insufficiency. After discontinuation of systemic corticosteroids, it takes several months to restore the function of the hypothalamic-pituitary-adrenal axis.
During stressful situations, including trauma, surgery, infectious diseases or a severe attack of bronchial asthma, patients who have previously received systemic corticosteroids require an additional short course of systemic corticosteroids, which are then gradually withdrawn as symptoms subside.
When switching from systemic corticosteroids, intranasal use of mometasone may result in the manifestation of concomitant allergic diseases, the symptoms of which were previously suppressed by the use of systemic corticosteroids.
During this period, some patients may experience signs of withdrawal from systemic corticosteroids, including muscle and/or joint pain, depression, and fatigue, despite the fact that pulmonary function tests are stable or even improving.
If signs of adrenal insufficiency occur, the dose of GCS for systemic use should be temporarily increased, and subsequently discontinued more gradually.
Patients receiving corticosteroids or other immunosuppressants should be advised to avoid contact with patients with certain infections (chicken pox, measles) and be sure to consult a doctor if such contact occurs (especially important when used in adolescents over 12 years of age).
To maintain a low hypothalamic-pituitary-adrenal axis suppressive potential, recommended doses should not be exceeded and the dose of mometasone should be titrated to the minimum effective dose in each patient.
When using mometasone, be aware that the effect on cortisol production may vary between patients.
The occurrence of candidiasis may require appropriate antifungal therapy or discontinuation of mometasone.
Use in pediatrics
It is recommended to regularly monitor the growth of adolescents receiving long-term therapy with mometasone. If growth slows, therapy should be reconsidered in order to reduce the dose of mometasone to the minimum effective dose to control the symptoms of the disease.
In placebo-controlled clinical studies in children with intranasal use of mometasone at a dose of 100 mcg/day for a year, no growth retardation was observed.
Active ingredient
Active ingredient
Mometasone
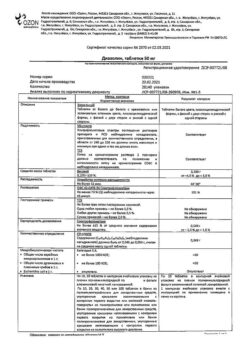
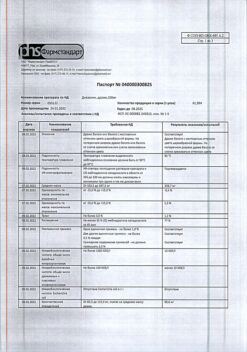
Composition
Composition
1 dose:
mometasone furoate monohydrate 0.0517 mg,
which corresponds to the content of mometasone furoate 0.05 m.
Excipients:
microcrystalline cellulose and carmellose sodium (Avicel RC-591) – 2 mg,
glycerin – 2.1 mg,
citric acid monohydrate – 0.2 mg,
sodium citrate dihydrate – 0.28 mg,
polysorbate 80 – 0.01 mg,
benzalkonium chloride – 0.02 mg,
water d/i – up to 100 mg.
Pregnancy
Pregnancy
There have been no adequate and well-controlled studies of the use of mometasone during pregnancy. It is not known whether mometasone is excreted in breast milk.
Intranasal use of mometasone during pregnancy and breastfeeding is only possible if the expected benefit to the mother outweighs the potential risk to the fetus or infant.
Newborns whose mothers received corticosteroids during pregnancy should be monitored for possible symptoms of adrenal insufficiency.
Contraindications
Contraindications
Hypersensitivity to mometasone;
recent surgery or trauma to the nose with damage to the mucous membrane of the nasal cavity – before the wound heals (due to the inhibitory effect of GCS on the healing processes);
children and adolescents up to 18 years of age with nasal polyposis;
children under 12 years of age with acute sinusitis or exacerbation of chronic sinusitis;
children under 2 years of age with seasonal and year-round allergic rhinitis.
Side Effects
Side Effects
From the respiratory system: with intranasal use, nosebleeds, pharyngitis, a burning sensation in the nose, sneezing are possible; irritation of the nasal mucosa; very rarely with intranasal use – cases of perforation of the nasal septum.
Other: possible headache.
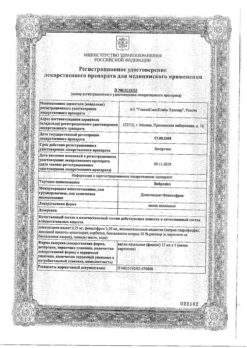
Manufacturer
Manufacturer
Lek d.d., Slovenia
Additional information
| Manufacturer | Lek d.d., Slovenia |
|---|---|
| Medication form | nasal spray |
| Brand | Lek d.d. |
Other forms…
Related products
Buy Mometazon Sandoz, spray 50 mcg/dose 10 g with delivery to USA, UK, Europe and over 120 other countries.