No products in the cart.
Meloxicam bufus, 10 mg/ml 1.5 ml 5 pcs
€14.25 €12.47
Description
Pharmacodynamics
Meloxicam is a non-steroidal anti-inflammatory drug with analgesic, anti-inflammatory and antipyretic effects. It belongs to the class of oxycams, derivatives of enolic acid. Anti-inflammatory effect is associated with inhibition of enzymatic activity of cyclooxygenase-2, which is involved in the biosynthesis of prostaglandins in the area of inflammation. To a lesser extent, meloxicam acts on cyclooxygenase-1, which is involved in the synthesis of prostaglandin that protects the mucosa of the gastrointestinal tract (GIT) and is involved in the regulation of blood flow in the kidneys.
Pharmacokinetics
Absorption
The relative bioavailability is about 100%. After intramuscular administration of the drug at a dose of 15 mg, the maximum plasma concentration of the drug (Cmax) is 1.62 µg/mL and is reached within approximately 60 minutes.
Distribution
Meloxicam binds well to plasma proteins, especially to albumin (99%). It penetrates the synovial fluid, the concentration in synovial fluid being approximately 50% of the plasma concentration of the drug. The volume of distribution is low, approximately 11 liters. Interindividual variation is 30-40%.
Metabolism
Meloxicam is almost completely metabolized in the liver to form four pharmacologically inactive metabolites. The main metabolite, 5′-carboxymeloxicam (60% of the dose value), is formed by oxidation of the intermediate metabolite 5′-hydroxymethylmeloxicam, which is also excreted, but to a lesser extent (9% of the dose value).
In vitro studies have shown that CYP2C9 isoenzyme plays an important role in this metabolic transformation, CYP3A4 isoenzyme has additional importance. Peroxidase, the activity of which probably varies individually, is involved in the formation of the other two metabolites (which constitute, respectively, 16% and 4% of the drug dose).
Extracted equally in the feces and urine, mainly as metabolites. Less than 5% of daily dose is excreted unchanged in feces, in urine the drug is excreted unchanged only in trace amounts. The average half-life of meloxicam is 20 hours. Plasma clearance averages 8 ml/min.
Hepatic and/or renal insufficiency
Hepatic insufficiency and mild to moderate renal insufficiency have no significant effect on the pharmacokinetics of meloxicam. In terminal renal insufficiency, increased volume of distribution may lead to higher concentrations of free meloxicam; therefore, in patients with hepatic and/or renal insufficiency, the daily dose should not exceed 7.5 mg.
Elderly patients
The average plasma clearance during equilibrium pharmacokinetics is slightly lower in elderly patients than in younger patients.
Indications
Indications
Initial therapy and short-term
symptomatic treatment for osteoarthritis (arthrosis, degenerative diseases
joints), rheumatoid arthritis, ankylosing spondylitis, other inflammatory
and degenerative diseases of the musculoskeletal system, such
such as arthropathy, dorsopathies (for example, sciatica, low back pain, shoulder
periarthritis and others), accompanied by pain.
Pharmacological effect
Pharmacological effect
Pharmacodynamics
Meloxicam is a non-steroidal anti-inflammatory drug that has analgesic, anti-inflammatory and antipyretic effects. Belongs to the class of oxicams, derivatives of enolic acid. The anti-inflammatory effect is associated with inhibition of the enzymatic activity of cyclooxygenase-2, which is involved in the biosynthesis of prostaglandins in the area of inflammation. To a lesser extent, meloxicam acts on cyclooxygenase-1, which is involved in the synthesis of prostaglandin, which protects the mucous membrane of the gastrointestinal tract (GIT) and takes part in the regulation of blood flow in the kidneys.
Pharmacokinetics
Absorption
Relative bioavailability is about 100%. After intramuscular administration of the drug at a dose of 15 mg, the maximum concentration of the drug in plasma (Cmax) is 1.62 μg/ml and is achieved within approximately 60 minutes.
Distribution
Meloxicam binds well to plasma proteins, especially albumin (99%). Penetrates into synovial fluid, the concentration in synovial fluid is approximately 50% of the plasma concentration of the drug. The distribution volume is low, approximately 11 liters. Interindividual differences are 30-40%.
Metabolism
Meloxicam is almost completely metabolized in the liver to form four pharmacologically inactive metabolites. The main metabolite, 5′-carboxymeloxicam (60% of the dose), is formed by oxidation of the intermediate metabolite 5′-hydroxymethylmeloxicam, which is also excreted, but to a lesser extent (9% of the dose).
In vitro studies have shown that the CYP2C9 isoenzyme plays an important role in this metabolic transformation; the CYP3A4 isoenzyme is of additional importance. Peroxidase is involved in the formation of the other two metabolites (constituting, respectively, 16% and 4% of the drug dose), the activity of which probably varies individually.
Removal
It is excreted equally in feces and urine, mainly in the form of metabolites. Less than 5% of the daily dose is excreted unchanged in feces; the drug is found unchanged in urine only in trace amounts. The average half-life of meloxicam is 20 hours. Plasma clearance averages 8 ml/min.
Insufficiency of liver and/or kidney function
Failure of liver function, as well as mild or moderate renal failure, do not have a significant effect on the pharmacokinetics of meloxicam. In end-stage renal failure, an increase in the volume of distribution may lead to higher concentrations of free meloxicam; therefore, in patients with impaired liver and/or renal function, the daily dose should not exceed 7.5 mg.
Elderly patients
In elderly patients, the average plasma clearance during steady-state pharmacokinetics is slightly lower than in younger patients.
Special instructions
Special instructions
Patients suffering from gastrointestinal diseases should be monitored regularly. If ulcerative lesions of the gastrointestinal tract or gastrointestinal bleeding occur, the drug must be discontinued.
Gastrointestinal ulcers, perforation, or bleeding may occur at any time during the use of NSAIDs, with or without warning symptoms or a history of serious gastrointestinal complications. The consequences of these complications are generally more serious in older people.
When using the drug, serious skin reactions such as exfoliative dermatitis, Stevens-Johnson syndrome, and toxic epidermal necrolysis may develop. Therefore, special attention should be paid to patients reporting the development of adverse events from the skin and mucous membranes, as well as hypersensitivity reactions to the drug, especially if such reactions were observed during previous courses of treatment. The development of such reactions is observed, as a rule, during the first month of treatment. If the first signs of skin rash, changes in mucous membranes or other signs of hypersensitivity appear, discontinuation of the drug should be considered.
When taking NSAIDs, cases of increased risk of developing serious cardiovascular thrombosis, myocardial infarction, and angina pectoris, possibly fatal, have been described. This risk increases with long-term use of the drug, as well as in patients with a history of the above diseases and predisposed to such diseases.
NSAIDs inhibit the synthesis of prostaglandins in the kidneys, which are involved in maintaining renal perfusion. The use of NSAIDs in patients with reduced renal blood flow or reduced circulating blood volume may lead to decompensation of latent renal failure. After discontinuation of NSAIDs, renal function usually returns to baseline levels. Elderly patients are most at risk of developing this reaction; patients with dehydration, chronic heart failure, liver cirrhosis, nephrotic syndrome or acute renal dysfunction; patients simultaneously taking diuretics, angiotensin-converting enzyme inhibitors, angiotensin-II receptor antagonists, as well as patients who have undergone major surgical interventions,
which lead to hypovolemia. In such patients, diuresis and renal function should be carefully monitored when initiating therapy. The use of NSAIDs in combination with diuretics can lead to sodium, potassium and water retention, as well as a decrease in the natriuretic effect of diuretics.
As a result, predisposed patients may experience increased signs of heart failure or hypertension. Therefore, such patients must be closely monitored and adequate hydration maintained. Before starting treatment, a kidney function test is necessary.
In case of combination therapy, renal function should also be monitored.
When using meloxicam (as well as most other NSAIDs), episodic increases in serum transaminase activity or other indicators of liver function are possible. In most cases, this increase was small and transitory. If the detected changes are significant or do not decrease over time, the drug should be discontinued and the detected laboratory changes should be monitored.
Weakened or malnourished patients may be less able to tolerate adverse events and should be monitored closely.
Like other NSAIDs, meloxicam may mask the symptoms of an underlying infectious disease.
The use of meloxicam, like other drugs that block cyclooxygenase and prostaglandin synthesis, can affect fertility and is therefore not recommended for women wishing to become pregnant. If the ability to conceive in women is impaired or when undergoing examination for infertility, it is necessary to consider discontinuing meloxicam.
In patients with mild or moderate renal impairment (creatinine clearance more than 25 ml/min), no dose adjustment is required.
In patients with liver cirrhosis (compensated), no dose adjustment is required.
Impact on the ability to drive vehicles and machinery
During the treatment period, due to possible side effects from the cardiovascular and nervous system, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Meloxicam
Composition
Composition
Active ingredient:
Meloxicam – 10,000 mg
Excipients:
glycofurol (tetraglycol) – 100,000 mg
Poloxamer 188 – 50,000 mg
meglumine – 6,250 mg
glycine – 5,000 mg
sodium chloride – 3,000 mg
sodium hydroxide – 0.152 mg
water for injection – up to 1 ml
Pregnancy
Pregnancy
The drug is contraindicated during pregnancy. The safety of this drug during pregnancy has not been proven. The effect of delayed prostaglandin synthesis on embryogenesis during the first two trimesters of pregnancy is unclear. In the last trimester of pregnancy, the mechanism of action of meloxicam is characterized by inhibition of labor, premature closure of the Ductus arteriosus Botalli in the fetus, an increased susceptibility to bleeding in the mother and child, and an increased risk of edema in the mother.
It is known that NSAIDs
passes into breast milk, so meloxicam is not recommended for use in
breastfeeding period.
Contraindications
Contraindications
– Hypersensitivity to the active substance or auxiliary components of the drug, to acetylsalicylic acid and other NSAIDs;
– complete or incomplete combination of bronchial asthma, recurrent polyposis of the nasal mucosa and paranasal sinuses, angioedema or urticaria caused by intolerance to acetylsalicylic acid or other NSAIDs due to the existing likelihood of cross-sensitivity (including history);
– erosive and ulcerative changes in the mucous membrane of the stomach and duodenum in the acute stage or recently suffered;
– inflammatory bowel diseases – Crohn’s disease or ulcerative colitis in the acute stage;
– active gastrointestinal bleeding, recent cerebrovascular bleeding or an established diagnosis of diseases of the blood coagulation system;
– severe liver failure or active liver disease;
– severe renal failure (if hemodialysis is not performed, creatinine clearance less than 30 ml/min), progressive kidney disease, including confirmed hyperkalemia;
– severe uncontrolled heart failure;
– therapy of perioperative pain during coronary artery bypass surgery;
– concomitant therapy with anticoagulants, as there is a risk of intramuscular hematoma formation;
– pregnancy;
– breastfeeding period;
– age up to 18 years.
With caution
– History of gastrointestinal (GIT) diseases (presence of Helicobacter pylori infection);
– chronic heart failure;
– coronary heart disease;
– renal failure (creatinine clearance 30-60 ml/min);
– cerebrovascular diseases;
– dyslipidemia/hyperlipidemia;
– diabetes mellitus;
– concomitant therapy with the following drugs: anticoagulants, oral glucocorticosteroids, antiplatelet agents, selective serotonin reuptake inhibitors;
– bronchial asthma, tuberculosis, severe osteoporosis;
– diseases of peripheral arteries;
– old age;
– long-term use of NSAIDs;
– smoking;
– frequent alcohol consumption.
To reduce the risk of developing adverse events from the gastrointestinal tract (GIT), the minimum effective dose should be used for the shortest possible short course.
Side Effects
Side Effects
The incidence of side effects is classified according to the recommendations of the World Health Organization, characterized as: very often (≥ 1/10), often (≥ 1/100, < 1/10), infrequently (≥ 1/1000, < 1/100), rarely (≥ 1/10000, < 1/1000), very rarely (< 1/10000), not established.
Disorders of the blood and lymphatic system: infrequently – anemia; rarely – leukopenia, thrombocytopenia, changes in the number of blood cells, including changes in the leukocyte formula.
Immune system disorders: uncommon – other immediate hypersensitivity reactions; not established – anaphylactic shock, anaphylactoid reactions.
Mental disorders: rarely – mood changes; not established – confusion, disorientation.
Nervous system disorders: often – headache; infrequently – dizziness, drowsiness.
Visual, hearing and labyrinthine disorders: uncommon – vertigo; rarely – conjunctivitis, visual impairment, including blurred vision, tinnitus.
Disorders of the heart and blood vessels: infrequently – increased blood pressure, a feeling of a “rush” of blood to the face; rarely – a feeling of palpitations.
Respiratory system disorders: rarely – bronchial asthma in patients with allergies to acetylsalicylic acid and other NSAIDs.
Gastrointestinal disorders: often – abdominal pain, dyspepsia, diarrhea, nausea, vomiting; uncommon – hidden and obvious gastrointestinal bleeding, gastritis, stomatitis, constipation, bloating, belching; rarely – gastroduodenal ulcers, colitis, esophagitis; very rarely – perforation of the gastrointestinal tract.
Disorders of the liver and biliary tract: infrequently – transient changes in liver function tests (for example, increased activity of transaminases or bilirubin); very rarely – hepatitis.
Skin and subcutaneous tissue disorders: uncommon – angioedema, itching, skin rash; rarely – toxic epidermal necrolysis, Stevens-Johnson syndrome, urticaria; very rarely – bullous dermatitis, erythema multiforme; not established – photosensitivity.
Renal and urinary tract disorders: uncommon – changes in renal function (increased levels of creatinine and/or urea in the blood serum), urinary disorders, including acute urinary retention; very rarely – acute renal failure.
Disorders of the genital organs and mammary glands: infrequently – late ovulation; not established – infertility in women.
General disorders and disorders at the injection site: often – pain and swelling at the injection site; infrequently – swelling.
Concomitant use with drugs that suppress bone marrow (for example, methotrexate) may cause cytopenia.
Gastrointestinal bleeding, ulceration, or perforation can be fatal.
As with other NSAIDs, the possibility of interstitial nephritis, glomerulonephritis, renal medullary necrosis, and nephrotic syndrome cannot be excluded.
Interaction
Interaction
Other inhibitors of prostaglandin synthesis, including glucocorticoids and salicylates. Concomitant use with meloxicam increases the risk of ulcers in the gastrointestinal tract and gastrointestinal bleeding (due to synergistic action). Concomitant use with other NSAIDs is not recommended.
Anticoagulants for oral administration, heparin for systemic use, thrombolytic agents. Concomitant use with meloxicam increases the risk of bleeding. In case of simultaneous use, careful monitoring of the blood coagulation system is necessary.
Antiplatelet drugs, serotonin reuptake inhibitors. Concomitant use with meloxicam increases the risk of bleeding due to inhibition of platelet function. In case of simultaneous use, careful monitoring of the blood coagulation system is necessary.
Lithium preparations. NSAIDs increase plasma lithium levels by decreasing renal excretion. The simultaneous use of meloxicam with lithium preparations is not recommended. If simultaneous use is necessary, careful monitoring of plasma lithium concentrations is recommended throughout the course of lithium use.
Methotrexate. NSAIDs reduce the secretion of methotrexate by the kidneys, thereby increasing its plasma concentration. The simultaneous use of meloxicam and methotrexate (at a dose of more than 15 mg per week) is not recommended. In case of simultaneous use, careful monitoring of renal function and blood count is necessary. Meloxicam may increase the hematological toxicity of methotrexate, especially in patients with impaired renal function.
Contraception. There is evidence that NSAIDs may reduce the effectiveness of intrauterine contraceptive devices, but this has not been proven. Mifepristone: Due to the theoretical risk of changes in the effectiveness of mifepristone under the influence of prostaglandin synthesis inhibitors, NSAIDs should not be prescribed earlier than 8-12 days after discontinuation of mifepristone.
Diuretics. The use of NSAIDs increases the risk of acute renal failure in patients with dehydration.
Antihypertensive drugs (beta-blockers, angiotensin-converting enzyme inhibitors, vasodilators, diuretics). NSAIDs reduce the effect of antihypertensive drugs due to inhibition of prostaglandins, which have vasodilating properties.
Angiotensin II receptor antagonists. When used together with NSAIDs, they increase the decrease in glomerular filtration, which can thereby lead to the development of acute renal failure, especially in patients with impaired renal function.
Cholestyramine, by binding meloxicam in the gastrointestinal tract, leads to its faster elimination.
Pemetrexed. When meloxicam and pemetrexed are used concomitantly in patients with a creatinine clearance of 45 to 79 ml/min, meloxicam should be discontinued 5 days before starting pemetrexed and possibly resumed 2 days after the end of treatment. If there is a need for concomitant use of meloxicam and pemetrexed, patients should be carefully monitored, especially for myelosuppression and the occurrence of gastrointestinal side effects.
In patients with creatinine clearance less than 45 ml/min, taking meloxicam with pemetrexed is not recommended.
NSAIDs, by acting on renal prostaglandins, may enhance the nephrotoxicity of cyclosporine.
When medicinal products known to inhibit CYP2C9 and/or CYP3A4 (or are metabolized by these enzymes), such as sulfonylureas or probenecid, are used with meloxicam, the potential for pharmacokinetic interaction should be taken into account.
When used concomitantly with oral antidiabetic agents (eg, sulfonylureas, nateglinide), interactions mediated by CYP2C9 are possible, which may lead to increased blood concentrations of both these drugs and meloxicam. Patients taking meloxicam concomitantly with a sulfonylurea or nateglinide should carefully monitor their blood sugar levels due to the possibility of hypoglycemia.
With simultaneous
the use of antacids, cimetidine, digoxin and furosemide are significant
no pharmacokinetic interactions were identified.
Overdose
Overdose
Symptoms: nausea, vomiting, epigastric pain, gastrointestinal bleeding, acute renal failure, liver failure, respiratory arrest, asystole, lethargy, drowsiness, changes in blood pressure, coma, convulsions, cardiovascular collapse, cardiac arrest, anaphylactoid reactions.
Treatment: specific antidote
absent. In case of drug overdose, carry out symptomatic
therapy. Forced diuresis, alkalization of urine, hemodialysis are ineffective
due to the high binding of the drug to blood proteins.
Storage conditions
Storage conditions
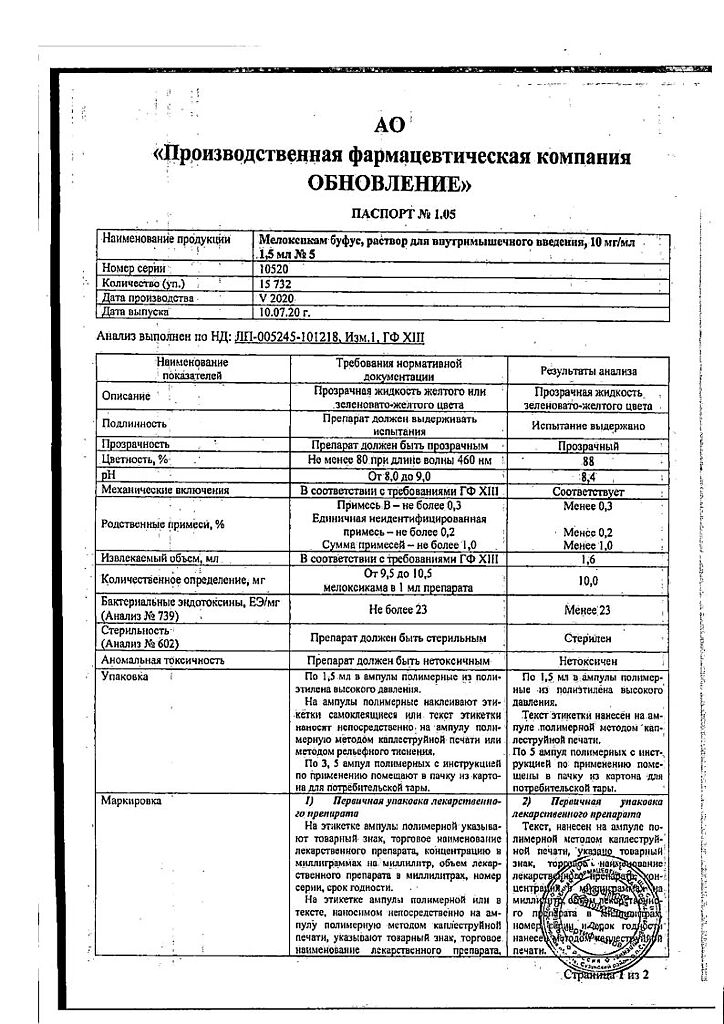
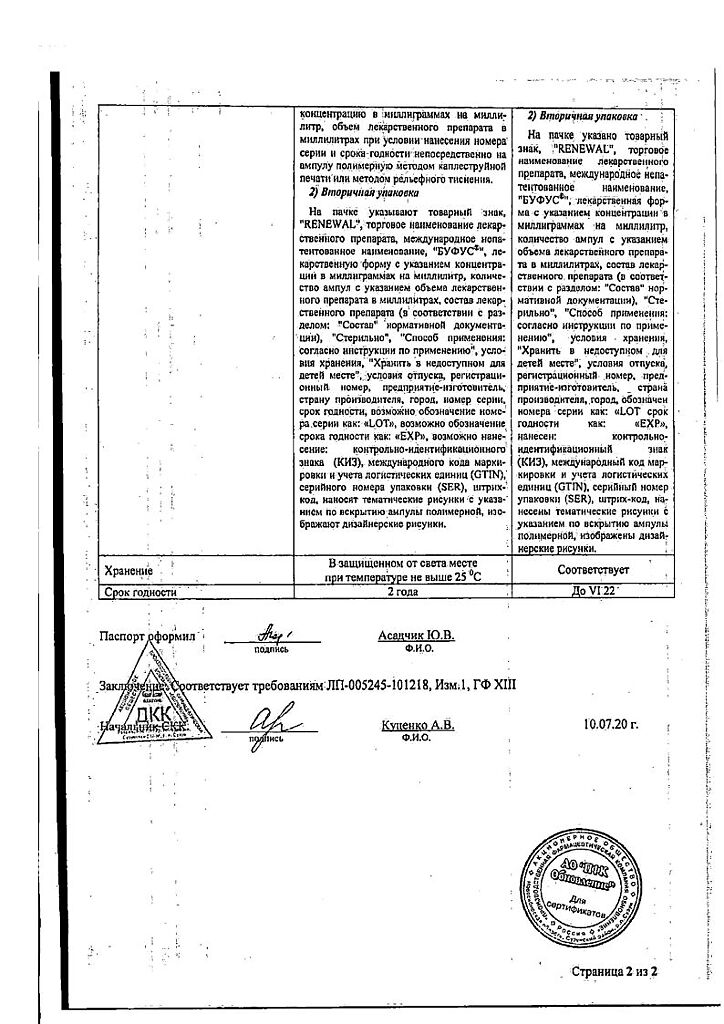
In a place protected from light at a temperature not exceeding 25 ° C.
Keep out of reach
place for children.
Shelf life
Shelf life
2 years.
Manufacturer
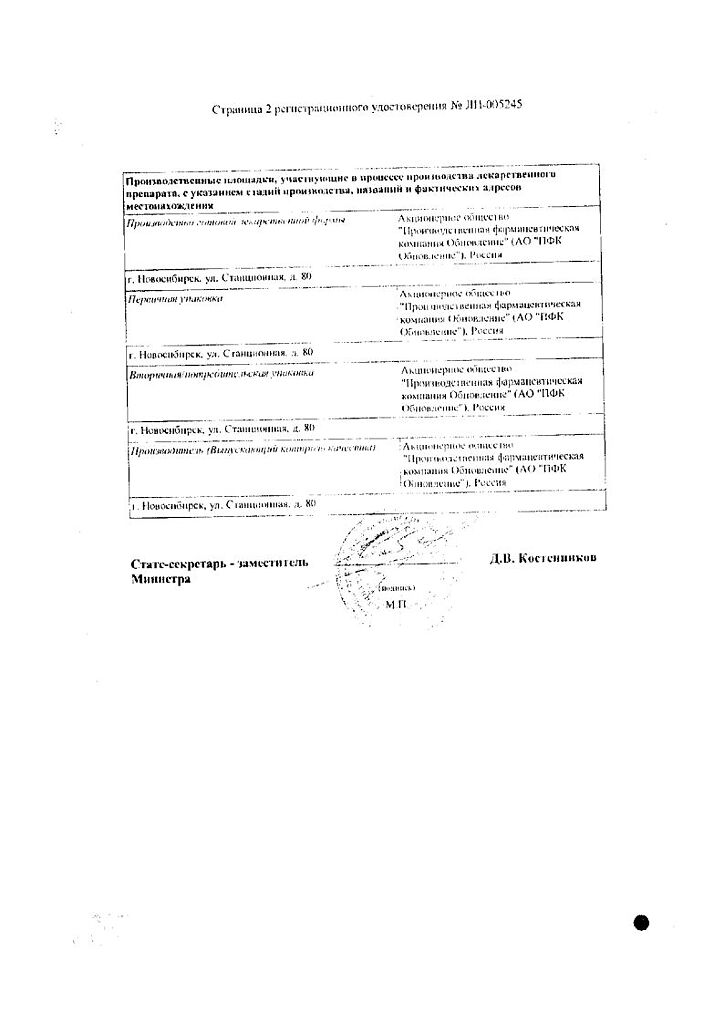
Manufacturer
Update of PFC JSC, Russia
Additional information
| Shelf life | 2 years. |
|---|---|
| Conditions of storage | In the dark place at a temperature not exceeding 25 °С. Contain out of reach of children. |
| Manufacturer | Update PFC AO, Russia |
| Medication form | solution |
| Brand | Update PFC AO |
Other forms…
Related products
Buy Meloxicam bufus, 10 mg/ml 1.5 ml 5 pcs with delivery to USA, UK, Europe and over 120 other countries.