No products in the cart.
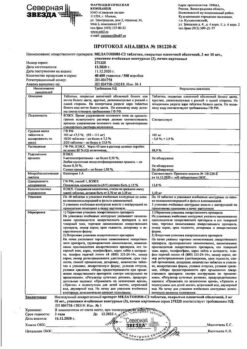
Melatonin-SZ, 3 mg 60 pcs.
€13.98 €11.65
EAN: 4690655019050
SKU: 327651
Categories: Medicine, Neurology and Psychiatry, Sedatives and hypnotics
Description
Synthetic analog of the pineal body hormone (epiphysis); it has adaptogenic, sedative and hypnotic effects.
Normalizes circadian rhythms. Increases the concentration of GABA and serotonin in the midbrain and hypothalamus, changes the activity of pyridoxal kinase, involved in the synthesis of GABA, dopamine and serotonin.
It regulates the sleep-wake cycle, daily changes in locomotor activity and body temperature, has a positive effect on the intellectual and mental functions of the brain and the emotional-personal sphere.
It helps to organize the biological rhythm and normalize night sleep. Improves the quality of sleep, speeds up falling asleep and regulates neuroendocrine functions. It adapts the body of people sensitive to changes in weather conditions.
Indications
Indications
Sleep disorders, incl. caused by a disturbance in the sleep-wake rhythm, such as desynchronosis (sudden change of time zones).
Pharmacological effect
Pharmacological effect
A synthetic analogue of the pineal gland hormone (epiphysis); has an adaptogenic, sedative, hypnotic effect.
Normalizes circadian rhythms. Increases the concentration of GABA and serotonin in the midbrain and hypothalamus, changes the activity of pyridoxal kinase, which is involved in the synthesis of GABA, dopamine and serotonin.
Regulates the sleep-wake cycle, daily changes in locomotor activity and body temperature, has a positive effect on the intellectual and mnestic functions of the brain, the emotional and personal sphere.
Helps organize biological rhythm and normalize night sleep. Improves sleep quality, speeds up falling asleep, regulates neuroendocrine functions. Adapts the body of weather-sensitive people to changes in weather conditions.
Special instructions
Special instructions
During the period of use of the drug Melatonin-SZ, it is recommended to avoid exposure to bright light.
It is necessary to inform women who want to become pregnant that the drug has a weak contraceptive effect. There are no clinical data on the use of melatonin in patients with autoimmune diseases, and therefore use in this category of patients is not recommended.
Influence on the ability to drive vehicles and operate machinery. The drug Melatonin-SZ causes drowsiness; therefore, during the treatment period, you should refrain from driving vehicles and engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Melatonin
Composition
Composition
Film-coated tablets
1 table
active substance:
melatonin
3 mg
excipients: MCC – 48.5 mg; sodium carboxymethyl starch – 6.5 mg; calcium hydrogen phosphate dihydrate – 41 mg; magnesium stearate – 1 mg
film shell: hypromellose – 1.53 mg; polysorbate80 (Tween80) – 0.64 mg; talc – 0.51 mg; titanium dioxide (E171) – 0.32 mg
Contraindications
Contraindications
hypersensitivity to the components of the drug;
autoimmune diseases;
liver failure;
severe renal failure;
pregnancy;
breastfeeding period;
children under 18 years of age.
With caution: patients with varying degrees of renal failure.
Side Effects
Side Effects
Classification of the frequency of side effects according to WHO recommendations: very often (≥1/10); often (from ≥1/100 to <1/10); uncommon (from ≥1/1000 to <1/100); rare (from ≥1/10000 to <1/1000); very rare (<1/10000), including isolated reports; frequency unknown (it is not possible to determine the frequency of occurrence based on available data).
Infectious and parasitic diseases: rarely – herpes zoster.
From the blood and lymphatic system: rarely – leukopenia, thrombocytopenia.
From the immune system: frequency unknown – hypersensitivity reactions.
Metabolism and nutrition: rarely – hypertriglyceridemia, hypokalemia, hyponatremia.
Mental disorders: infrequently – irritability, nervousness, anxiety, insomnia, unusual dreams, nightmares, anxiety; rarely – mood swings, aggression, agitation, tearfulness, symptoms of stress, disorientation, early morning awakening, increased libido, decreased mood, depression.
From the nervous system: infrequently – migraine, headache, lethargy, psychomotor hyperactivity, dizziness, drowsiness; rarely – fainting, memory impairment, impaired concentration, delirium, restless leg syndrome, poor quality of sleep, paresthesia.
From the organ of vision: rarely – decreased visual acuity, blurred vision, increased lacrimation.
From the organ of hearing and labyrinthine disorders: rarely – vertigo, positional vertigo.
From the cardiovascular system: infrequently – arterial hypertension; rarely – angina pectoris, palpitations, hot flashes.
From the gastrointestinal tract: uncommon – abdominal pain, abdominal pain in the upper abdomen, dyspepsia, ulcerative stomatitis, dry mouth, nausea; rarely – GERD, gastrointestinal disorder or disorder, bullous stomatitis, ulcerative glossitis, vomiting, increased peristalsis, bloating, hypersecretion of saliva, bad breath, abdominal discomfort, gastric dyskinesia, gastritis.
From the liver and biliary tract: rarely – hyperbilirubinemia.
From the skin and subcutaneous tissues: uncommon – dermatitis, night sweats, itching and generalized itching, rash, dry skin; rarely – eczema, erythema, hand dermatitis, psoriasis, generalized rash, itchy rash, nail damage; frequency unknown – Quincke’s edema, swelling of the oral mucosa, swelling of the tongue.
From the musculoskeletal system and connective tissue: infrequently – pain in the extremities; rarely – arthritis, muscle spasms, neck pain, night cramps.
From the kidneys and urinary tract: infrequently – glucosuria, proteinuria; rarely – polyuria, hematuria, nocturia.
From the genital organs and mammary gland: infrequently – menopausal symptoms; rarely – priapism, prostatitis; frequency unknown – galactorrhea.
General disorders and disorders at the injection site: uncommon – asthenia, chest pain; rarely – fatigue, pain, thirst.
Laboratory and instrumental data: infrequently – deviation from the norm in laboratory parameters of liver function, increase in body weight; rarely – increased activity of liver transaminases, abnormal levels of electrolytes in the blood, abnormal results of laboratory tests.
Interaction
Interaction
Pharmacokinetic interaction
– it is known that in concentrations significantly exceeding therapeutic levels, melatonin induces the CYP3A isoenzyme in vitro. The clinical significance of this phenomenon is not fully understood. If signs of induction develop, consider reducing the dose of concomitantly used drugs;
– at concentrations significantly higher than therapeutic levels, melatonin does not induce CYP1A isoenzymes in vitro. Therefore, the interaction of melatonin with other drugs due to the effect of melatonin on isoenzymes of the CYP1A group is apparently insignificant;
– Melatonin metabolism is mainly mediated by CYP1A isoenzymes. Therefore, it is possible that melatonin may interact with other drugs due to the effect of melatonin on isoenzymes of the CYP1A group;
– Caution should be exercised in patients taking fluvoxamine, which increases the concentration of melatonin (increase in AUC by 17 times and Cmax by 12 times) due to inhibition of its metabolism by cytochrome P450 isoenzymes: CYP1A2 and CYP2C19. This combination should be avoided;
– Caution should be exercised in patients taking 5- and 8-methoxypsoralen, which increases melatonin concentrations due to inhibition of its metabolism;
– Caution should be exercised in patients taking cimetidine (an inhibitor of CYP2D isoenzymes), since it increases plasma melatonin levels by inhibiting the latter;
– smoking can reduce the concentration of melatonin due to the induction of the CYP1A2 isoenzyme;
– Caution should be exercised in patients taking estrogens (for example, contraceptives or hormone replacement therapy), which increase melatonin concentrations by inhibiting their metabolism by CYP1A1 and CYP1A2 isoenzymes;
– inhibitors of CYPA2 isoenzymes, such as quinolones, can increase melatonin exposure;
– inducers of the CYP1A2 isoenzyme, such as carbamazepine and rifampicin, can reduce the plasma concentration of melatonin;
– in modern literature there is a lot of data regarding the effect of agonists/antagonists of adrenergic and opioid receptors, antidepressants, PG inhibitors, benzodiazepines, tryptophan and alcohol on the secretion of endogenous melatonin. There have been no studies of the mutual influence of these drugs on the dynamics or kinetics of melatonin.
Pharmacodynamic interaction
– while taking melatonin you should not drink alcohol, because… it reduces the effectiveness of the drug;
Melatonin potentiates the sedative effect of benzodiazepine and non-benzodiazepine hypnotics such as zaleplon, zolpidem and zopiclone. In a clinical study, clear evidence of a transient pharmacodynamic interaction between melatonin and zolpidem was observed one hour after administration. Combined use may lead to progressive impairment of attention, memory and coordination compared to zolpidem monotherapy;
– During the studies, melatonin was prescribed together with thioridazine and imipramine, drugs that affect the central nervous system. In none of the cases was there a clinically significant pharmacokinetic interaction. However, concomitant use with melatonin resulted in increased feelings of calmness and difficulty performing certain tasks compared with imipramine monotherapy, as well as increased feelings of brain fog compared with thioridazine monotherapy.
Overdose
Overdose
Symptoms: according to available literature data, the use of melatonin in a daily dose of up to 300 mg did not cause clinically significant adverse reactions. Flushing, abdominal cramps, diarrhea, headache and scotoma have been observed with melatonin doses of 3000–6600 mg for several weeks. When very high doses of melatonin (up to 1 g) were used, involuntary loss of consciousness was observed. In case of overdose, drowsiness may develop.
Treatment: gastric lavage and use of activated carbon, symptomatic therapy. Clearance of the active substance is expected within 12 hours after oral administration.
Recommendations for use
Recommendations for use
Inside, 30–40 minutes. For sleep disturbances – 3 mg 1 time per day.
For desynchrosis, as an adaptogen when changing time zones – 1 day before the flight and in the next 2-5 days – 3 mg. The maximum daily dose is 6 mg.
Elderly patients. With age, melatonin metabolism decreases, which must be taken into account when choosing a dosage regimen for elderly patients. Taking this into account in elderly patients, it is possible to take the drug 60–90 minutes before bedtime.
Kidney failure. The effect of varying degrees of renal impairment on the pharmacokinetics of melatonin has not been studied, so melatonin should be taken with caution in such patients. The use of the drug is not recommended for patients with severe renal failure.
Functional features
Functional features
Absorption. Melatonin after oral administration is quickly absorbed into the gastrointestinal tract. In elderly people, the rate of absorption may be reduced by 50%. The kinetics of melatonin in the range of 2–8 mg is linear. When administered orally at a dose of 3 mg, Cmax in blood plasma and saliva is achieved after 20 and 60 minutes, respectively. Serum Tmax is 60 min (normal range 20–90 min). Following administration of 3–6 mg melatonin, serum Cmax is typically 10 times that of endogenous serum melatonin at night.
Concomitant meals delay the absorption of melatonin.
Bioavailability. The oral bioavailability of melatonin ranges from 9 to 33% (approximately 15%).
Distribution. In in vitro studies, the binding of melatonin to plasma proteins is 60%. Melatonin binds primarily to albumin, α1-acid glycoprotein, and HDL. Vd about 35 l. It is quickly distributed into saliva and passes through the blood-brain barrier, and is detected in the placenta. The concentration in cerebrospinal fluid is 2.5 times lower than in plasma.
Biotransformation. Melatonin is metabolized primarily in the liver. After oral administration, melatonin undergoes significant transformation during its initial passage through the liver, where it is hydroxylated and conjugated with sulfate and glucuronide to form 6-sulfatoxymelatonin; the level of first-pass metabolism can reach 85%. Experimental studies suggest that isoenzymes CYP1A1, CYP1A2 and, possibly, CYP2C19 of the cytochrome P450 system are involved in the metabolism of melatonin. The main metabolite of melatonin, 6-sulfatoxymelatonin, is inactive.
Selection. Melatonin is excreted from the body by the kidneys. The average T1/2 of melatonin is 45 minutes. Excretion is carried out in the urine, about 90% in the form of sulfate and glucuronic conjugates of 6-hydroxymelatonin, and about 2–10% was excreted unchanged.
Pharmacokinetic parameters are affected by age, caffeine intake, smoking, and oral contraceptives. In critically ill patients, accelerated absorption and impaired elimination are observed.
Old age. Melatonin metabolism is known to slow down with age. At different doses of melatonin, higher AUC and Cmax values were obtained in the elderly, reflecting reduced melatonin metabolism in this group of patients.
Renal dysfunction. With long-term treatment, no accumulation of melatonin was observed. These data are consistent with the short T1/2 of melatonin in humans.
Liver dysfunction. The liver is the main organ involved in melatonin metabolism, so liver diseases lead to increased concentrations of endogenous melatonin. In patients with liver cirrhosis, plasma melatonin concentrations increased significantly during the daytime.
Manufacturer
Manufacturer
North Star NAO, Russia
Additional information
| Manufacturer | North Star NAO, Russia |
|---|---|
| Medication form | pills |
| Brand | North Star NAO |
Other forms…
Related products
Buy Melatonin-SZ, 3 mg 60 pcs. with delivery to USA, UK, Europe and over 120 other countries.