No products in the cart.
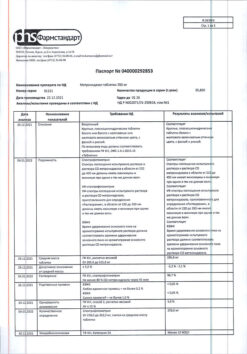
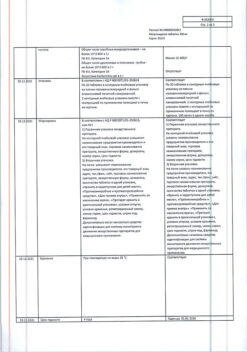
Mefloquine, tablets 250 mg 10 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Mefloquine is active against asexual intracellular erythrocytic forms of human malaria pathogens Plasmodium falciparum Plasmodium vivax against circulating schizonts Plasmodium malariae and Plasmodium ovale.
He is not active against hepatic stages of the parasites.
It is effective against malaria pathogens resistant to other antimalarial drugs such as chloroquine proguanil pyrimethamine and combination of pyrimethamine and sulfonamides.
For P. falciparum, resistance to mefloquine may have developed mainly in Southeast Asia. Cross-resistance between mefloquine and halofantrine mefloquine and quinine has been noted in some regions. National expert organizations should be consulted for up-to-date information on resistance in different geographic regions.
The drug does not cause hemolysis associated with glucose-6-phosphate dehydrogenase deficiency.
Pharmacokinetics:
Absorption
The absolute bioavailability of mefloquine after oral administration was not assessed (no intravenous form of release). The bioavailability of the tablet form is over 85% of that of the oral solution. Food intake significantly accelerates the rate and increases the degree of absorption by 40%.
The average time to reach the maximum concentration of Mefloquine after a single dose is 17 hours (6-24 hours). Maximum plasma concentrations in µg/L are approximately equal to the dose taken in mg (e.g., a single dose of 1000 mg gives a maximum concentration of about 1000 µg/L).
After administration of 250 mg once weekly, an equilibrium maximum plasma concentration of 1000-2000 µg/L is reached after 7-10 weeks. A blood concentration of mefloquine equal to 620 ng/ml is required to achieve 95% efficacy of prophylaxis.
Distribution
The volume of distribution of mefloquine is 20 l/kg which indicates penetration of the drug into many tissues. It accumulates in erythrocytes with malaria parasites inside at concentrations approximately twice as high as plasma concentrations. It penetrates through the placenta and into the breast milk.
The excretion with the breast milk seems to be minimal (see section “Administration during pregnancy and breast-feeding”).
The drug’s binding to plasma proteins is 98%.
Metabolism
Metabolism of Mefloquine is mainly carried out in the liver with the participation of cytochrome P450. In in vitro and in vivo studies it was shown that mefloquine is metabolized mainly by CYP3A4 isoenzyme to form 2 metabolites: the main metabolite – 28-bis-trifluoromethyl-4-quinoline carboxylic acid and alcohol.
The main metabolite is inactive against P. falciparum appears in plasma 2-4 hours after a single oral administration of the drug; its maximum concentrations in plasma are 50% higher than those of Mefloquine and are reached after 2 weeks. After that, plasma concentrations of the main metabolite and mefloquine decrease at the same rate. The area under the curve “concentration-time” of the main metabolite is 3-5 times greater than that of the original drug.
The other metabolite alcohol is present in very small amounts.
Excretion
The average half-life of mefloquine is 3 weeks (2 to 4 weeks) unchanged by long-term antimalarial prophylaxis. It is excreted as metabolic products mainly with bile and feces. Total clearance, most of which is hepatic, is 30 ml/min. The excretion of unchanged mefloquine and its main metabolite by the kidneys is about 9% and 4% respectively. Other metabolites are not detected in the urine.
Pharmacokinetics in special cases
In acute malaria changes in pharmacokinetic parameters may be observed.
Children and elderly patients
Age has no effect on the pharmacokinetics of mefloquine.
Renal failure
Pharmacokinetic studies in patients with renal failure have not been conducted because very small amounts of the drug are excreted with the kidneys. Mefloquine and its main metabolite are not excreted in any significant quantities by hemodialysis. No dose adjustment is required for patients on hemodialysis.
Hepatic impairment
In patients with impaired hepatic function, excretion of mefloquine may be delayed and therefore plasma concentrations of the drug are increased. Pregnancy has no clinically significant effect on the pharmacokinetics of mefloquine.
Race
Pharmacokinetic differences have very little clinical significance compared to the immune status of the infected patient and the sensitivity of the pathogen.
Indications
Indications
Treatment of mild and moderate forms of malaria caused by strains of P. falciparum resistant to other antimalarial drugs P. vivax and malaria of mixed etiology.
Given that the sensitivity of the pathogen may vary over time and depending on the geographical area, it is recommended that national and international guidelines be followed.
Prevention of malaria in persons traveling to malaria-prone regions, especially to regions with a high risk of infection by strains of P. falciparum resistant to other antimalarial drugs.
Emergency therapy (self-help): self-administration as emergency treatment for suspected malaria if immediate medical attention is not possible.
Pharmacological effect
Pharmacological effect
Mefloquine acts on the asexual intracellular erythrocyte forms of human malaria pathogens Plasmodium falciparum Plasmodium vivax on circulating schizonts Plasmodium malariae and Plasmodium ovale.
Not active against liver stages of parasites.
Effective against malaria pathogens resistant to other antimalarial drugs, such as chloroquine proguanil pyrimethamine and a combination of pyrimethamine with sulfonamides.
P. falciparum may develop resistance to mefloquine, mainly in Southeast Asia. In some regions, cross-resistance has been observed between mefloquine and halofantrine, mefloquine and quinine. National expert organizations should be consulted for up-to-date information on resistance in different geographic regions.
The drug does not cause hemolysis associated with glucose-6-phosphate dehydrogenase deficiency.
Pharmacokinetics:
Suction
The absolute bioavailability of mefloquine after oral administration has not been assessed (there is no intravenous release). The bioavailability of the tablet form is over 85% of that when taking the solution orally. Eating food significantly speeds up the rate and increases the degree of absorption by 40%.
The average time to reach the maximum concentration of mefloquine after a single dose is 17 hours (6-24 hours). Maximum plasma concentrations in mcg/l are approximately equal to the dose taken in mg (for example, a single dose of 1000 mg gives a maximum concentration of about 1000 mcg/l).
After taking 250 mg once a week, a steady-state maximum flame concentration of 1000-2000 mcg/L is achieved after 7-10 weeks. To achieve 95% effectiveness of prevention, a mefloquine blood concentration of 620 ng/ml is required.
Distribution
The volume of distribution of mefloquine is 20 l/kg, which indicates penetration of the drug into many tissues. It accumulates in red blood cells, which contain malaria parasites in concentrations approximately twice as high as plasma levels. Penetrates through the placenta and into breast milk.
Excretion into breast milk appears to be minimal (see section “Use during pregnancy and breastfeeding”).
The association of the drug with plasma proteins is 98%.
Metabolism
Mefloquine is metabolized mostly in the liver with the participation of cytochrome P450. In vitro and in vivo studies have shown that mefloquine is metabolized mainly by the CYP3A4 isoenzyme with the formation of 2 metabolites: the main metabolite is 28-bis-trifluoromethyl-4-quinoline carboxylic acid and alcohol.
The main metabolite is inactive against P. falciparum and appears in the plasma 2-4 hours after a single oral dose of the drug; its maximum plasma concentrations are 50% higher than those of mefloquine and are achieved after 2 weeks. After this, the concentrations of the main metabolite and mefloquine in plasma decrease at the same rate. The area under the concentration-time curve of the main metabolite is 3-5 times higher than that of the parent drug.
Another metabolite, alcohol, is present in very small quantities.
Removal
The average half-life of mefloquine is 3 weeks (range 2 to 4 weeks) and does not change during long-term antimalarial prophylaxis. It is excreted in the form of metabolic products mainly with bile and feces. The total clearance, most of which is hepatic, is 30 ml/min. Renal excretion of unchanged mefloquine and its main metabolite is about 9% and 4%, respectively. Other metabolites are not detected in urine.
Pharmacokinetics in special cases
In acute malaria, changes in pharmacokinetic parameters may be observed.
Children and elderly patients
Age does not affect the pharmacokinetics of mefloquine.
Kidney failure
Pharmacokinetic studies have not been conducted in patients with renal failure since very small amounts of the drug are excreted by the kidneys. Mefloquine and its main metabolite are not excreted in any significant quantities by hemodialysis. No dose adjustment is required for patients on hemodialysis.
Liver failure
In patients with impaired liver function, the elimination of mefloquine may slow down, resulting in increased plasma concentrations of the drug. Pregnancy does not have a clinically significant effect on the pharmacokinetics of mefloquine.
Race
Pharmacokinetic differences are of very little clinical significance when compared with the immune status of the infected patient and the susceptibility of the pathogen.
Special instructions
Special instructions
Mefloquine may increase the risk of seizures in patients with epilepsy. Therefore, in such patients the drug can be prescribed only for the purpose of treatment and if there are absolute indications for its use (see also section “Interaction with other drugs”).
After taking quinine or quinidine, you can take mefloquine no earlier than 12 hours later.
In patients with impaired liver function, the elimination of mefloquine may be delayed, which may lead to increased concentrations of the latter in the blood plasma and an increased risk of adverse reactions.
When prescribed prophylactically for a long time (taking the drug for more than 1 year is undesirable), periodic analysis of liver function indicators and an ophthalmological examination are necessary.
The safety profile of mefloquine when used prophylactically is characterized by a predominance of neuropsychiatric reactions such as anxiety, depression, anxiety or confusion. If these adverse events occur, therapy with Mefloquine should be discontinued and another drug should be prescribed.
Due to the long half-life of mefloquine, adverse reactions may develop or persist for up to several weeks after the last dose of the drug. In a small number of patients, cases of psychoneurotic disorders (including depression, dizziness and vertigo, and loss of balance) were described that were observed for several months or more after discontinuation of the drug and continued for several months after discontinuation of the drug.
Cases of visual impairment, including optic neuropathy and retinal damage (including maculopathy), have been reported with the use of mefloquine. If visual impairment occurs, you should contact your doctor to consider the possibility of continuing treatment with Mefloquine.
If symptoms of polyneuropathy develop, including pain, burning, tingling, numbness and/or weakness, treatment with the drug should be discontinued. The choice of drug for the prevention of malaria depends on the resistance of P. falciparum to it in a particular region (see section “Pharmacological action”).
Cases of agranulocytosis and aplastic anemia have been reported when using the drug (see section “Side effects”).
The release of medicinal products into the environment should be minimized. Mefloquine should not be disposed of with wastewater or household waste. Where possible, special systems should be used to dispose of medications.
Impact on the ability to drive vehicles. Wed and fur.:
During treatment, it is necessary to refrain from driving vehicles and engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Mefloquine
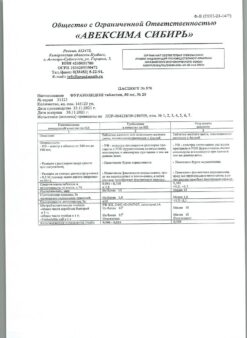
Composition
Composition
For one tablet:
Active ingredient: mefloquine hydrochloride – 274.09 mg (in terms of base – 250.00 mg).
Excipients: microcrystalline cellulose – 193.41 mg, povidone K-25 – 25 mg, crospovidone – 2.5 mg, magnesium stearate – 2.5 mg, colloidal silicon dioxide – 2.5 mg.
Pregnancy
Pregnancy
Pregnancy
When mefloquine was administered in doses 5-20 times higher than therapeutic doses for humans, it had a teratogenic effect in mice and rats and an embryotoxic effect in rabbits. However, the experience of clinical use of the drug Mefloquine did not reveal any embryotoxic or teratogenic effects. However, Mefloquine should be prescribed in the first trimester of pregnancy only if the expected benefit to the mother outweighs the potential risk to the fetus.
Women of reproductive age should be treated only if they use reliable contraception while taking mefloquine and for 3 months after the last dose. But if pregnancy occurs during chemoprophylaxis of malaria with the drug Mefloquine, there are no indications for its termination.
When prescribing mefloquine to pregnant women, they should refer to current international guidelines (eg WHO).
Breastfeeding period
The activity of small amounts of mefloquine passed into breast milk is unknown. No adverse reactions were noted in breastfed children whose mothers took the drug Mefloquine.
When prescribing mefloquine to nursing mothers, current international guidelines (eg WHO) should be referred to.
Contraindications
Contraindications
Hypersensitivity to mefloquine to any components of the drug or related drugs (quinine, quinidine).
Combined use with halofantrine: taking halofantrine after mefloquine therapy for 15 weeks after discontinuation of the latter.
Combined use with ketoconazole: taking ketoconazole after mefloquine therapy for 15 weeks after discontinuation of the latter.
Use for prophylactic purposes in active forms of depression and severe mental disorders, seizures (including history).
Children under 3 months of age or weighing less than 5 kg (experience with the drug is limited).
Lactose intolerance, lactase deficiency, glucose-galactose malabsorption (due to the presence of lactose in the drug).
With caution:
Liver failure epilepsy mental illness heart disease age over 65 years.
In combination with quinine and quinidine.
Side Effects
Side Effects
Adverse reactions were classified according to organ system classes and absolute incidence according to MedDRA.
The frequency of occurrence was determined as follows: very common (>1/10) common (>1/100 and 1/1000 and 1/10000 and <1/1000) very rare (<1/10000) frequency unknown (it is impossible to determine the frequency based on the available data).
Due to the long presence of the drug on the market, the data presented in the list of adverse reactions below reflects the frequency of occurrence based on the frequency of reports received and not on the frequency of cases observed in controlled studies.
Blood and lymphatic system disorders
Common: thrombocytopenia.
Uncommon: leukopenia leukocytosis.
Frequency unknown: agranulocytosis and aplastic anemia.
Metabolic and nutritional disorders
Common: anorexia.
Mental disorders
Very common: sleep disturbances (insomnia, nightmares).
Common: agitation anxiety anxiety depression aggression emotional lability panic attacks confusion hallucinations bipolar disorder psychotic reactions including delusional disorder depersonalization and mania paranoia. Infrequently, these symptoms persist for a long time after discontinuation of mefloquine.
Cases of suicide have been reported: suicidal thoughts and behaviors with a risk of harming oneself, such as suicide attempts.
Nervous system disorders
Very common: dizziness, loss of balance, headache, drowsiness.
Common: fainting, memory impairment, sensory and motor neuropathies (including paresthesia, tremor, ataxia), convulsions.
Uncommon: encephalopathy.
Visual disorders
Common: visual disturbances.
Frequency unknown: blurred vision, cataracts, retinal lesions and optic neuropathy with the possibility of delayed onset both during and after completion of therapy.
Hearing and labyrinth disorders
Very common: vergigo.
Common: hearing loss, vestibular disorders including tinnitus.
Heart disorders
Often: tachycardia, palpitations, bradycardia, arrhythmia, extrasystoles, other transient cardiac conduction disorders.
Uncommon: AV block.
Vascular disorders
Common: circulatory disorders (decreased blood pressure, hot flashes).
Disorders of the respiratory system of the chest and mediastinum
Common: shortness of breath.
Very rare: pneumonia pneumonitis (possibly of allergic etiology).
Gastrointestinal disorders
Very common: nausea, diarrhea, abdominal pain, vomiting.
Common: dyspepsia.
Disorders of the liver and biliary tract
Frequency unknown: liver dysfunction associated with the use of the drug (from asymptomatic transient increase in transaminase activity to liver failure).
Skin and subcutaneous tissue disorders
Common: skin rash, exanthema, erythema, urticaria, itching, alopecia, hyperhidrosis.
Uncommon: erythema multiforme Stevens-Johnson syndrome.
Musculoskeletal and connective tissue disorders
Common: muscle weakness, muscle cramps, myalgia, arthralgia.
Laboratory and instrumental data
Often: transient increase in transaminase activity.
General and administration site disorders
Common: swelling chest pain weakness feeling unwell fatigue chills fever.
Interaction
Interaction
Concomitant use of Mefloquine and quinine, quinidine and chloroquine may cause changes in the ECG and increase the risk of seizures (see section “Dosage and Administration”).
The use of halofantrine simultaneously with Mefloquine and also within 15 weeks after the last dose of Mefloquine leads to a significant prolongation of the QTc interval (the QT interval corrected for heart rate is calculated by the formula:
QTc=QT/RR1/2 where
RR – the time interval between adjacent R waves on the ECG is equal to the duration of the cardiac cycle) (see section “Special instructions”).
Concomitant use of Mefloquine and ketoconazole increases plasma concentrations of mefloquine and its half-life.
Prescribing ketoconazole concurrently with Mefloquine and within 15 weeks after the last dose of Mefloquine may result in a prolongation of the QTc interval. There is no clinically significant QTc prolongation with mefloquine therapy.
Concomitant use of other drugs that affect cardiac conduction (antiarrhythmic drugs, beta-blockers, slow calcium channel blockers, antihistamines, in particular H1-histamine receptor blockers, tricyclic antidepressants and phenothiazines) can also theoretically play a role in prolonging the QTc interval. The effect of simultaneous use of mefloquine and the above drugs on cardiac function has not been fully established.
Reduces the effectiveness of anticonvulsants (valproic acid, carbamazepine, phenobarbital or phenytoin) by reducing their plasma concentrations. It is necessary to monitor the concentration of drugs in plasma. In some cases, the dose of anticonvulsants may need to be adjusted.
Mefloquine may reduce the immunogenicity of oral live typhoid vaccines when administered concomitantly; therefore, vaccination with live attenuated vaccines should be completed at least 3 days before the first dose of Mefloquine.
Other drug interactions with Mefloquine are unknown. But persons receiving other drugs, in particular anticoagulants or hypoglycemic agents, must undergo medical control before leaving for an endemic region.
Other possible interactions
Mefloquine is not an inhibitor or inducer of cytochrome P450. Therefore, it can be expected that the metabolism of drugs prescribed concomitantly with mefloquine will remain unchanged.
However, inhibitors of the CYP3A4 isoenzyme may alter the pharmacokinetics and metabolism of mefloquine, which may lead to increased plasma concentrations of mefloquine and the possible development of adverse reactions. In this regard, caution should be exercised when using mefloquine and CYP3A4 isoenzyme inhibitors simultaneously.
Inducers of the CYP3A4 isoenzyme may also alter the pharmacokinetics and metabolism of mefloquine, which may result in decreased plasma concentrations of mefloquine.
CYP3A4 isoenzyme inhibitors
A study involving healthy volunteers showed that simultaneous administration of ketoconazole, a strong inhibitor of the CYP3A4 isoenzyme, and mefloquine led to an increase in plasma concentrations of the latter and its half-life.
Inducers of the CYP3A4 isoenzyme
Long-term use of rifampicin, a powerful inducer of the CYP3A4 isoenzyme, led to a decrease in the plasma concentration of mefloquine and its half-life.
P-glycoprotein substrates and inhibitors
Mefloquine is a P-gp inhibitor based on in vitro studies. Therefore, the possibility of drug interaction between mefloquine and drugs that are substrates of P-glycoprotein or have the ability to change the expression of this transporter cannot be excluded. The clinical significance of this interaction is currently unknown. In clinical studies, rigonavir, a potent inhibitor of P-glycoprotein and CYP3A4, did not affect the pharmacokinetics of mefloquine in healthy volunteers.
Overdose
Overdose
Symptoms: see section “Side effects”, however, more pronounced. Treatment: in case of overdose, symptomatic and supportive therapy is recommended. There is no specific antidote.
Storage conditions
Storage conditions
In a dry place, protected from light, at a temperature not exceeding 25 ° C.
Keep out of the reach of children.
Shelf life
Shelf life
3 years.
Manufacturer
Manufacturer
FSUE Pharmzaschita NPC, Russia
Additional information
| Shelf life | 3 years. |
|---|---|
| Conditions of storage | In a dry place protected from light at a temperature not exceeding 25 ° C. Contain out of reach of children. |
| Manufacturer | FGUP Pharmzaschita NPC, Russia |
| Medication form | pills |
| Brand | FGUP Pharmzaschita NPC |
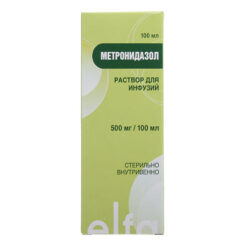
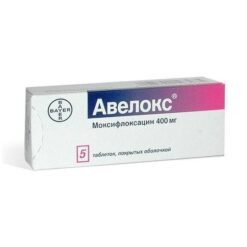
Related products
Buy Mefloquine, tablets 250 mg 10 pcs with delivery to USA, UK, Europe and over 120 other countries.