No products in the cart.
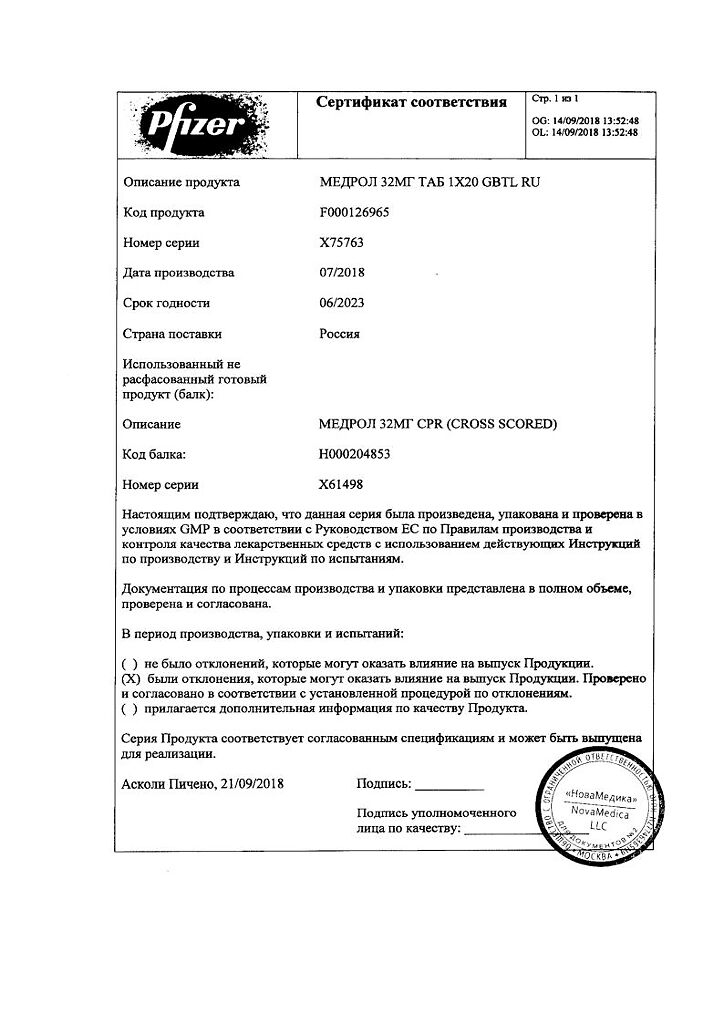
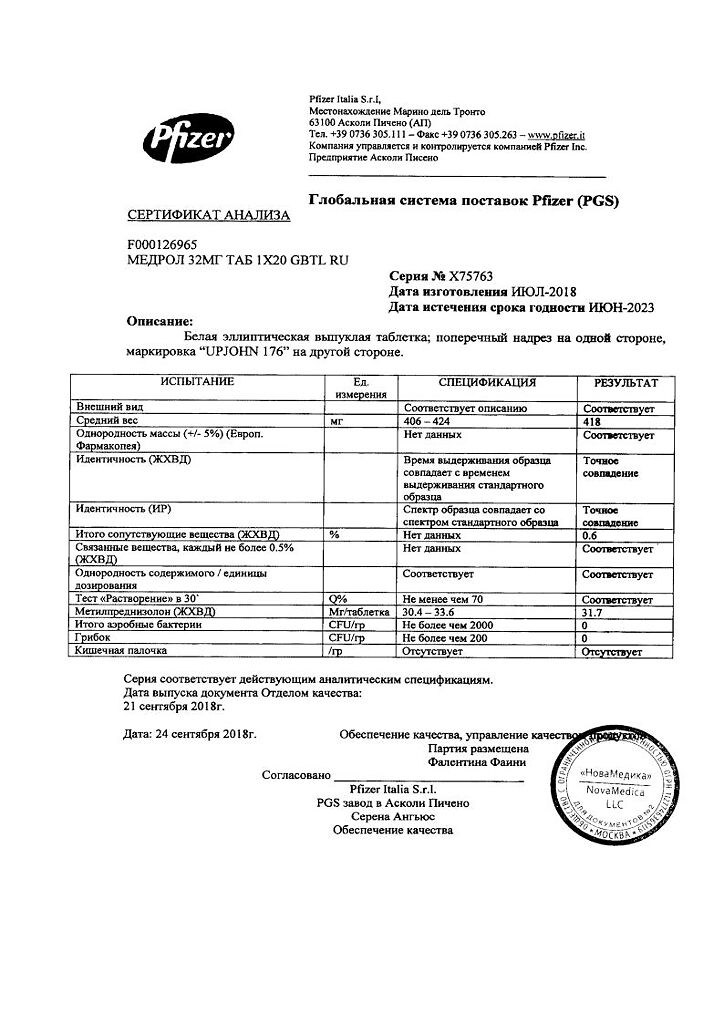
Medrol, 32 mg tablets 20 pcs
€1.00
Out of stock
(E-mail when Stock is available)
EAN: 4601951000697
SKU: 113566
Categories: Bronchial asthma, Corticosteroid hormones, Medicine, Pain and fever
Description
Medrol is a GCS. Penetrating through cell membranes it forms complexes with specific cytoplasmic receptors. Then these complexes penetrate into the cell nucleus, bind to DNA (chromatin) and stimulate mRNA transcription and subsequent synthesis of various enzymes, which explains the effect of GCS when used systemically. GCS not only have a significant effect on the inflammatory process and immune response, but also affect carbohydrate, protein and fat metabolism. They also affect the cardiovascular system, skeletal muscles and the central nervous system.
The effects on the inflammatory process and immune response. Methylprednisolone (like other GKS) has anti-inflammatory, immunosuppressive and anti-allergic properties. Due to these properties the following therapeutic effects are achieved: reduction of the number of immunoactive cells near the focus of inflammation; reduction of vasodilation; stabilization of lysosomal membranes; inhibition of phagocytosis; reduction of prostaglandin and related compounds production.
Methylprednisolone acetate at a dose of 4.4 mg (4 mg of methylprednisolone) has the same anti-inflammatory effect as hydrocortisone at a dose of 20 mg.
Methylprednisolone has only slight mineralocorticoid activity (200 mg of methylprednisolone is equivalent to 1 mg of deoxycorticosterone).
The effect on carbohydrate and protein metabolism. Methylprednisolone (like other GKS) has a catabolic effect on proteins. Released amino acids are converted into glucose and glycogen during gluconeogenesis in the liver. Glucose uptake in peripheral tissues decreases, which can lead to hyperglycemia and glucosuria, especially in patients at risk of developing diabetes.
The effect on fat metabolism. Methylprednisolone (like other GKS) has lipolytic effects, which are primarily seen in the extremities. It also has a lipogenetic effect, which is most pronounced in the chest, neck and head. All this leads to a redistribution of fat deposits.
The maximum pharmacological activity of GCS is not observed at peak plasma concentrations but only afterwards, therefore GCS activity is primarily determined by the effect on enzyme activity.
Pharmacokinetics
Absorption and distribution
Absorption of methylprednisolone occurs primarily in the proximal small intestine, where it is about 2 times greater than in the distal colon.
The binding of methylprednisolone to proteins (albumin and transcortin) is about 40-90%.
Metabolism
Metabolism of methylprednisolone occurs in the liver and is qualitatively similar to that of cortisol. The main metabolites are 20p-hydroxymethylprednisolone and 20p-hydroxy-6a-methylprednisolone.
Elimation
The metabolites are excreted mainly with the urine in unbound form and also in the form of glucuronides and sulfates, which are formed mainly in the liver and partially in the kidneys.
Methylprednisolone is a GCS with intermediate duration of action. Due to intracellular activity, there is a marked difference between T1/2 from blood plasma (approximately 3.3 hours) and T1/2 from the body as a whole (approximately 12-36 hours). The pharmacotherapeutic effect is maintained even when the level of active substance in blood is no longer determined.
Indications
Indications
Endocrine diseases:
primary and secondary adrenal insufficiency (the drugs of choice are hydrocortisone or cortisone; if necessary, synthetic analogues can be used in combination with mineralocorticoids; the addition of mineralocorticoids is of particular importance in pediatric practice);
congenital adrenal hyperplasia;
chronic and subacute thyroiditis;
hypercalcemia in malignant neoplasms.
Diseases of the musculoskeletal system (including rheumatic) (as an additional therapy for a short time to relieve an acute condition or during exacerbation):
psoriatic arthritis;
rheumatoid arthritis, including juvenile rheumatoid arthritis (in some cases, low-dose maintenance therapy may be required);
ankylosing spondylitis;
acute and subacute bursitis;
acute nonspecific tenosynovitis;
acute gouty arthritis;
post-traumatic osteoarthritis;
synovitis in osteoarthritis;
epicondylitis.
Systemic connective tissue diseases (during exacerbation or in some cases as maintenance therapy):
acute rheumatic carditis;
systemic lupus erythematosus;
systemic dermatomyositis (polymyositis);
polymyalgia rheumatica;
giant cell arteritis.
Skin diseases:
pemphigus;
bullous dermatitis herpetiformis;
severe erythema multiforme (Stevens-Johnson syndrome);
exfoliative dermatitis;
mycosis fungoides;
severe psoriasis;
severe seborrheic dermatitis.
Allergic reactions (severe or disabling conditions for which conventional therapy is ineffective):
seasonal or year-round allergic rhinitis;
serum sickness;
bronchial asthma;
contact dermatitis;
atopic dermatitis;
hypersensitivity reactions to drugs.
Eye diseases (severe acute and chronic allergic and inflammatory processes with eye damage):
allergic marginal corneal ulcers;
inflammation of the anterior segment of the eye;
diffuse posterior uveitis and choroiditis;
sympathetic ophthalmia;
allergic conjunctivitis;
keratitis;
chorioretinitis;
optic neuritis;
iritis and iridocyclitis.
Respiratory diseases:
symptomatic sarcoidosis;
Loeffler’s syndrome, which cannot be treated with other means;
berylliosis;
fulminant or disseminated pulmonary tuberculosis in combination with appropriate anti-tuberculosis chemotherapy;
aspiration pneumonitis.
Hematological diseases:
idiopathic thrombocytopenic purpura in adults;
secondary thrombocytopenia in adults;
acquired (autoimmune) hemolytic anemia;
erythroblastopenia (erythrocyte anemia);
congenital (erythroid) hypoplastic anemia.
Oncological diseases (as palliative therapy):
leukemia and lymphoma in adults;
acute leukemia in children.
Edema syndrome:
to stimulate diuresis and achieve remission of proteinuria in patients with nephrotic syndrome without uremia, idiopathic type, or caused by systemic lupus erythematosus.
Gastrointestinal diseases (to remove the patient from a critical condition):
ulcerative colitis;
regional enteritis.
Nervous system diseases:
exacerbation of multiple sclerosis;
swelling of the brain caused by a brain tumor.
Other indications for use:
tuberculous meningitis with subarachnoid block or threatened block (in combination with appropriate anti-tuberculosis chemotherapy);
trichinosis with damage to the nervous system or myocardium;
organ transplantation.
Pharmacological effect
Pharmacological effect
Medrol – GCS. Penetrating through cell membranes, it forms complexes with specific cytoplasmic receptors. Then these complexes penetrate the cell nucleus, bind to DNA (chromatin) and stimulate the transcription of mRNA and the subsequent synthesis of various enzymes, which explains the effect of GCS when used systemically. GCS not only have a significant effect on the inflammatory process and the immune response, but also affect carbohydrate, protein and fat metabolism. They also have effects on the cardiovascular system, skeletal muscles and the central nervous system.
Influence on the inflammatory process and immune response. Methylprednisolone (like other corticosteroids) has anti-inflammatory, immunosuppressive and antiallergic properties. Thanks to these properties, the following therapeutic effects are achieved: reducing the number of immunoactive cells near the site of inflammation; decreased vasodilation; stabilization of lysosomal membranes; inhibition of phagocytosis; decreased production of prostaglandins and related compounds.
Methylprednisolone acetate at a dose of 4.4 mg (4 mg methylprednisolone) has the same anti-inflammatory effect as hydrocortisone at a dose of 20 mg.
Methylprednisolone has only minor mineralocorticoid activity (200 mg methylprednisolone is equivalent to 1 mg deoxycorticosterone).
Effect on carbohydrate and protein metabolism. Methylprednisolone (like other corticosteroids) has a catabolic effect on proteins. The released amino acids are converted into glucose and glycogen during gluconeogenesis in the liver. Glucose uptake in peripheral tissues is reduced, which can lead to hyperglycemia and glycosuria, especially in patients at risk of developing diabetes mellitus.
Effect on fat metabolism. Methylprednisolone (like other corticosteroids) has a lipolytic effect, which primarily manifests itself in the extremities. It also has a lipogenetic effect, which is most pronounced in the chest, neck and head. All this leads to the redistribution of fat deposits.
The maximum pharmacological activity of GCS does not appear at the peak of plasma concentration, but after it; therefore, the effect of GCS is primarily due to its effect on enzyme activity.
Pharmacokinetics
Suction and distribution
Absorption of methylprednisolone occurs mainly in the proximal part of the small intestine, where it is approximately 2 times greater than in the distal part.
The binding of methylprednisolone to proteins (albumin and transcortin) is approximately 40-90%.
Metabolism
The metabolism of methylprednisolone occurs in the liver and is qualitatively similar to the metabolism of cortisol. The main metabolites are 20p-hydroxymethylprednisolone and 20p-hydroxy-6a-methylprednisone.
Removal
Metabolites are excreted mainly in the urine in unbound form, as well as in the form of glucuronides and sulfates, which are formed mainly in the liver and partly in the kidneys.
Methylprednisolone is a corticosteroid with an intermediate duration of action. Due to intracellular activity, a pronounced difference is revealed between T1/2 from blood plasma (approximately 3.3 hours) and T1/2 from the body as a whole (approximately 12-36 hours). The pharmacotherapeutic effect persists even when the level of the active substance in the blood is no longer determined.
Special instructions
Special instructions
Before starting treatment, the patient should be examined to identify possible contraindications. Clinical examination should include a study of the cardiovascular system, x-ray examination of the lungs, examination of the stomach and duodenum; urinary system, visual organs.
Before and during steroid therapy, it is necessary to monitor a general blood count, the concentration of glucose in the blood and urine, and electrolytes in the plasma. For intercurrent infections, septic conditions and tuberculosis, simultaneous antibiotic therapy is necessary. Immunizations should not be performed during treatment.
With sudden withdrawal, especially in the case of previous use of high doses, GCS “withdrawal” syndrome occurs: decreased appetite, nausea, lethargy, generalized musculoskeletal pain, asthenia. After discontinuation, relative insufficiency of the adrenal cortex persists for several months. If stressful situations arise during this period, GCS is prescribed (according to indications) for the duration, if necessary – in combination with MCS.
Children who during the treatment period were in contact with patients with measles or chickenpox are prescribed specific Ig prophylactically. To reduce side effects, it is justified to prescribe anabolic steroids and increase the intake of K+ from food. In Addison’s disease, simultaneous administration of barbiturates should be avoided – there is a risk of developing acute adrenal insufficiency (Addisonian crisis).
Use during pregnancy in the first trimester and during lactation: prescribed taking into account the expected therapeutic effect and negative effect on the fetus and child. With long-term therapy during pregnancy, fetal growth is impaired.
In the third trimester of pregnancy, there is a risk of atrophy of the adrenal cortex in the fetus, which may require replacement therapy in the newborn. In children during the growth period, GCS should be used only according to absolute indications and under the particularly careful supervision of the attending physician.
Active ingredient
Active ingredient
Methylprednisolone
Composition
Composition
1 tablet contains:
Active substance:
methylprednisolone 32 mg;
Excipients:
calcium stearate;
corn starch;
lactose;
sucrose.
Pregnancy
Pregnancy
The use of Medrol during pregnancy is possible if the expected effect of therapy outweighs the potential risk to the fetus (adequate and strictly controlled safety studies have not been conducted).
Women of childbearing age should be warned of the potential risk to the fetus (corticosteroids cross the placenta).
Breastfeeding women are advised to stop either breastfeeding or the use of drugs, especially in high doses (corticosteroids pass into breast milk and can inhibit the production of endogenous corticosteroids, suppress growth and cause undesirable effects in offspring).
Contraindications
Contraindications
Hypersensitivity to the components of the drug.
The drug should be used with caution in case of gastric and duodenal ulcers, esophagitis, gastritis, acute or latent peptic ulcers, intestinal anastomosis (in the immediate history), nonspecific ulcerative colitis with the threat of perforation or abscess, diverticulitis;
diabetes mellitus and predisposition to it; hyperlipidemia;
myasthenia gravis, osteoporosis, hypothyroidism, hyperthyroidism, acute psychosis, acute and subacute myocardial infarction, congestive heart failure, arterial hypertension, severe liver dysfunction (especially with concomitant hypoalbuminemia) or kidneys, open-angle glaucoma, herpes simplex (ocular form), chicken pox, measles, strongyloidiasis, AIDS, HIV infection;
for active and latent tuberculosis, severe bacterial or viral infectious diseases (increases the risk of developing superinfection, masks the symptoms of the disease), the use of the drug is permissible only against the background of specific therapy.
For systemic fungal infections, the use of the drug is not recommended.
Side Effects
Side Effects
From the metabolic side: sodium retention, chronic heart failure in patients with a corresponding predisposition, increased blood pressure, fluid retention in the body, potassium loss and hypokalemic alkalosis, negative nitrogen balance due to protein catabolism.
From the musculoskeletal system: steroid myopathy, muscle weakness, osteoporosis, pathological fractures, vertebral compression fractures, aseptic necrosis of the epiphyses of tubular bones, tendon ruptures, especially the Achilles tendon.
From the digestive system: peptic ulcer with possible perforation and bleeding, gastric bleeding, pancreatitis, esophagitis, intestinal perforation. After treatment with GCS, an increase in the activity of ALT, AST and alkaline phosphatase in the blood serum was observed. Usually these changes are minor, not associated with any clinical syndromes and are reversible after cessation of treatment.
Dermatological reactions: slow wound healing, petechiae and ecchymosis, thinning and decreased strength of the skin.
From the nervous system: increased intracranial pressure, pseudotumor cerebri, mental disorders, convulsions.
From the endocrine system: menstrual irregularities, hirsutism, development of Cushing’s syndrome, suppression of the pituitary-adrenal system, decreased tolerance to carbohydrates, manifestation of latent diabetes mellitus, increased need for insulin or oral hypoglycemic agents in patients with diabetes, growth retardation in children.
From the organ of vision: posterior subcapsular cataract, increased intraocular pressure with the risk of damage to the optic nerve, exophthalmos.
Allergic reactions: hypersensitivity reactions, including allergic systemic reactions, suppression of reactions during skin testing is possible.
Other: blurred clinical picture in infectious diseases, activation of latent infections, the occurrence of infections caused by opportunistic pathogens, GCS withdrawal syndrome.
Interaction
Interaction
Increases the toxicity of cardiac glycosides (due to the resulting hypokalemia, the risk of developing arrhythmias increases). Accelerates the elimination of ASA, reduces its concentration in the blood (when methylprednisolone is discontinued, the concentration of salicylates in the blood increases and the risk of side effects increases).
When used simultaneously with live antiviral vaccines and against the background of other types of immunization, it increases the risk of viral activation and the development of infections. Increases the metabolism of isoniazid, mexiletine (especially in “fast” acetylators), which leads to a decrease in their plasma concentrations. Increases the risk of developing hepatotoxic reactions of paracetamol (induction of “liver” enzymes and the formation of a toxic metabolite of paracetamol).
Increases (with long-term therapy) the content of folic acid. Hypokalemia caused by GCS can increase the severity and duration of muscle blockade due to muscle relaxants. In high doses, it reduces the effect of somatropin. Antacids reduce the absorption of corticosteroids. Reduces the effect of hypoglycemic drugs; enhances the anticoagulant effect of coumarin derivatives. Weakens the effect of vitamin D on the absorption of Ca2+ in the intestinal lumen.
Ergocalciferol and parathyroid hormone prevent the development of osteopathy caused by GCS. Reduces the concentration of praziquantel in the blood. Ketoconazole reduces the clearance and increases the toxicity of methylprednisolone. Combined use with cyclosporine causes mutual inhibition of metabolism – the risk of developing side effects of both drugs (cases of seizures have been reported when used together).
Thiazide diuretics, carbonic anhydrase inhibitors, other corticosteroids and amphotericin B increase the risk of hypokalemia, Na+-containing drugs – edema and increased blood pressure. NSAIDs and ethanol increase the risk of developing ulceration of the gastrointestinal mucosa and bleeding; in combination with NSAIDs for the treatment of arthritis, it is possible to reduce the dose of GCS due to the summation of the therapeutic effect. Indomethacin, displacing methylprednisolone from its association with albumin, increases the risk of developing its side effects.
Amphotericin B and carbonic anhydrase inhibitors increase the risk of osteoporosis. The therapeutic effect of GCS is reduced under the influence of phenytoin, barbiturates, ephedrine, theophylline, rifampicin and other inducers of “liver” microsomal enzymes (increased metabolic rate). Mitotane and other inhibitors of adrenal cortex function may necessitate an increase in the dose of GCS. The clearance of GCS increases against the background of thyroid hormones.
Immunosuppressants increase the risk of developing infections and lymphoma or other lymphoproliferative disorders associated with the Epstein-Barr virus. Estrogens (including oral estrogen-containing contraceptives) reduce the clearance of GCS, prolong T1/2 and their therapeutic and toxic effects.
The appearance of hirsutism and acne is facilitated by the simultaneous use of other steroid hormonal drugs – androgens, estrogens, anabolic steroids, oral contraceptives. Tricyclic antidepressants may increase the severity of depression caused by taking corticosteroids (not indicated for the treatment of these side effects). The risk of developing cataracts increases when used in conjunction with other corticosteroids, antipsychotic drugs (neuroleptics), carbutamide and azathioprine.
Simultaneous administration with m-anticholinergics (including antihistamines, tricyclic antidepressants), nitrates contributes to the development of increased intraocular pressure.
Overdose
Overdose
The clinical syndrome of acute drug overdose has not been described. Reports of cases of acute toxicity following an overdose of GCS are extremely rare.
Symptoms: frequent repeated use (daily or several times a week) for a long time can lead to the development of Cushing’s syndrome and other complications characteristic of long-term GCS therapy.
Treatment: symptomatic therapy. Methylprednisolone is eliminated by dialysis. There is no specific antidote.
Storage conditions
Storage conditions
At 20–25 °C
Shelf life
Shelf life
5 years
Manufacturer
Manufacturer
USA
Additional information
| Shelf life | 5 years |
|---|---|
| Conditions of storage | At a temperature of 20-25 °C |
| Manufacturer | Pfizer, Puerto Rico |
| Medication form | pills |
| Brand | Pfizer |
Other forms…
Related products
Buy Medrol, 32 mg tablets 20 pcs with delivery to USA, UK, Europe and over 120 other countries.