No products in the cart.
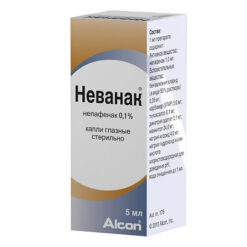
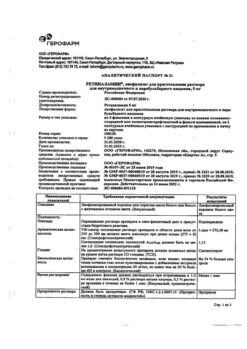
Maxiflox, eye drops 5 mg/ml 5 ml
€1.00
Out of stock
(E-mail when Stock is available)
Description
An antibacterial drug of the group of IV generation fluoroquinolones. It inhibits DNA-phase and topoisomerase IV, which in the bacterial cell carry out DNA replication, recombination and repair.
Moxifloxacin is active against most strains of microorganisms (both in vitro and in vivo).
Gram-positive bacteria: Corynebacterium spp, including Corynebacterium diphtheriae; Micrococcus luteus (including strains insensitive to erythromycin, gentamicin, tetracycline and/or trimethoprim); Staphylococcus aureus (including strains insensitive to methicillin, erythromycin, gentamicin, ofloxacin, tetracycline and/or trimethoprim); Staphylococcus epidermidis (including strains insensitive to methicillin, erythromycin, gentamicin, ofloxacin, tetracycline and/or trimethoprim); Staphylococcus haemolyticus (including strains insensitive to methicillin, erythromycin, gentamicin, ofloxacin, tetracycline and/or trimethoprim); Staphylococcus hominis (including strains insensitive to methicillin, erythromycin, tetracycline and/or trimethoprim); Staphylococcus warneri (including strains insensitive to erythromycin); Streptococcus mitis (including strains insensitive to penicillin, erythromycin, tetracycline and/or trimethoprim); Streptococcus pneumoniae (including strains insensitive to penicillin, gentamicin, erythromycin, tetracycline and/or trimethoprim); Streptococcus viridians group (including strains insensitive to penicillin, erythromycin, tetracycline and/or trimethoprim).
Gram-negative bacteria: Acinetobacter lwoffii, Haemophilus influenzae (including ampicillin-insensitive strains); Haemophilus parainfluenzae; Klebsiella spp.
Other microorganisms: Chlamydia trachomatis.
Moxifloxacin acts in vitro against most of the microorganisms listed below, but the clinical significance of these data is unknown.
Gram-positive bacteria: Listeria monocytogenes, Staphylococcus saprophyticus, Streptococcus agalactiae, Streptococcus mitis, Streptococcus pyogenes, Streptococcus groups C, G, F.
Gram-negative bacteria: Acinetobacter baumannii, Acinetobacter calcoaceticus, Citrobacter freundii, Citrobacter koseri, Enterobacter aerogenes, Enterobacter cloacae, Escherichia coli, Klebsiella oxytoca, Klebsiella pneumonia, Moraxella catarrhalis, Morganella morganii, Neisseria gonorrhoeae, Proteus mirabilis, Proteus vulgaris, Pseudomonas stutzeri.
Anaerobic microorganisms: Clostridium perfringens, Fusobacterium spp, Prevotella spp, Propionibacterium acnes.
Other microorganisms: Chlamydia pneumoniae, Legionella pneumophila, Mycobacterium avium, Mycobacterium marinum, Mycoplasma pneumoniae.
There are no data on the relationship between the clinical and bacteriological outcome of infectious diseases of the eye against the background of moxifloxacin therapy.
According to epidemiological data of the European Committee for the determination of sensitivity to antimicrobial agents, the threshold values of inhibitory concentration of moxifloxacin for various microorganisms are as follows:
Corynebacterium – no data;
Staphylococcus aureus – 0.25 mg/l;
Staphylococcus, coag-neg. – 0.25 mg/l;
Streptococcus pneumoniae – 0.5 mg/l;
Streptococcus pyogenes – 0.5 mg/l;
Streptococcus, viridans group – 0.5 mg/l;
Enterobacter spp. – 0.25 mg/l;
Haemophilus influenzae – 0.125 mg/l;
Klebsiella spp. – 0.25 mg/L;
Moraxella catarrhalis – 0.25 mg/L;
Morganella morganii – 0.25 mg/L;
Neisseria gonorrhoeae – 0.032 mg/l;
Pseudomonas aeruginosa – 4 mg/l;
Serratia marcescens – 1 mg/l.
Mechanisms of resistance development
Resistance to antibiotics of fluoroquinolone series, including moxifloxacin, develops through chromosomal mutations in the genes encoding DNA-phase and topoisomerase IV. In Gram-negative bacteria resistance to moxifloxacin is associated with mutations in the system of multiple resistance to antibiotics and resistance to quinolones.
The development of resistance is also associated with the expression of efflux proteins and inactivating enzymes. Cross-resistance with antibiotics of the macrolide, aminoglycoside and tetracycline groups is not expected due to differences in the mechanism of action.
The development of resistance can have significant geographic variation, and also varies significantly over time, so it is important to have local knowledge of microbial resistance before initiating therapy, which is of particular importance in the treatment of severe infections.
Pharmacokinetics
Absorption and distribution
When applied topically moxifloxacin is systemic absorption. Plasma concentration of moxifloxacin was determined in 21 male and female patients who received moxifloxacin in dosage form of eye drops in both eyes – 1 drop 3 times per day for 4 days.
The mean plasma Cmax of moxifloxacin at equilibrium was 2.7 ng/ml, the AUC was 41.9 ng×h/ml. These values are approximately 1,600 and 1,200 times less than the average Cmax and AUC after oral therapeutic dose of moxifloxacin 400 mg.
The T1/2 of moxifloxacin is about 13 h.
.
Indications
Indications
Bacterial conjunctivitis caused by microorganisms sensitive to moxifloxacin.
Active ingredient
Active ingredient
Composition
Composition
1 ml:
Excipients:
boric acid – 3 mg,
sodium chloride – 6.5 mg,
Hydrochloric acid solution 1M/sodium hydroxide solution 1M – to pH 6.7-7.0,
purified water – to 1 ml.
How to take, the dosage
How to take, the dosage
The drug is intended for local application in ophthalmic practice only. It is not intended for use as subconjunctival injections or for injection into the anterior chamber of the eye.
The official recommendations for antibiotic therapy should be considered when treating.
Adults (including elderly patients over 65 years of age) are prescribed 1 drop 3 times daily in the affected eye. Improvement of condition comes after 5 days of therapy, but treatment should be continued for another 2-3 days.
If there is no therapeutic effect after 5 days of therapy, it is recommended to reconsider the diagnosis and the choice of therapeutic strategy.
The duration of therapy depends on the severity of the patient’s condition and the clinical and bacteriological characteristics of the infectious process.
In children, no dosing adjustment is required.
In patients with hepatic and renal insufficiency no dose adjustment is required.
To prevent microbial contamination of the tip of the dropper bottle and the drug, contact with the eyelids, periorbital skin and other surfaces should be avoided.
In order to prevent absorption of the drug through the nasal mucosa, the nasolacrimal duct should be squeezed with a finger for 2-3 minutes after instillation.
If several topical ophthalmic products are used, the interval between applications should be at least 5 minutes; eye ointments should be used last.
Interaction
Interaction
Special studies of interaction of the drug Maxiflox with other medicinal products have not been conducted. Due to the low systemic concentration after topical application in the form of instillation, interactions with other drugs are unlikely.
Special Instructions
Special Instructions
In patients receiving quinolone drugs for systemic use, severe and in some cases fatal hypersensitivity reactions (anaphylaxis) may be observed, in some cases after the first dose.
Some reactions have been accompanied by collapse, loss of consciousness, Quincke’s edema (including swelling of the larynx, pharynx or face), airway obstruction, shortness of breath, urticaria and skin itching.
In case of an allergic reaction, the drug should be discontinued. Severe acute reactions of hypersensitivity to moxifloxacin and other components of the drug may require immediate resuscitation: oxygen therapy with monitoring of airway patency may be conducted by indications.
In prolonged use of the drug an overgrowth of non-susceptible microorganisms, including fungi, is possible. If superinfection occurs, the drug should be withdrawn and appropriate therapy should be prescribed.
Inflammation and tendon rupture have been reported with systemic use of fluoroquinolones, primarily in elderly patients, and in patients receiving corticosteroids along with fluoroquinolones.
While systemic concentrations of moxifloxacin after topical administration in ophthalmology are significantly lower than those of oral administration, the drug should be discontinued at the first signs of tendon inflammation.
There is insufficient data to support a conclusion regarding the efficacy and safety of Maxiflox in the treatment of bacterial conjunctivitis in infants; therefore, use in patients in this age group is not recommended.
Maxiflox is not recommended for prophylactic use or ex juvantibus therapy (empirical treatment) of gonococcal conjunctivitis, including gonococcal ophthalmia in infants, due to the large number of Neisseria gonorrhoeae strains resistant to moxifloxacin.
Patients with infectious diseases of the eye caused by Neisseria gonorrhoeae should receive appropriate systemic therapy.
The use of Maxiflox in the treatment of ocular infections caused by Chlamydia trachomatis in patients less than 2 years of age is not recommended because there are no data on the study of the drug in this category of patients.
The use of Maxiflox in patients over 2 years of age with ocular diseases caused by Chlamydia trachomatis should be combined with systemic therapy.
In cases of neonatal ophthalmia, patients should receive appropriate treatment for their condition; for example, if conjunctivitis develops with a chlamydial or gonorrheic etiology, this would be systemic therapy.
Infectious diseases of the anterior eye are not recommended for contact lens wear.
Impact on driving and operating machinery
As with instillations of other drugs, temporary blurring of vision is possible after use of the drug. It is not recommended to drive or operate machinery until visual acuity is restored.
Contraindications
Contraindications
Children under 1 year of age;
Individual hypersensitivity to the components of the drug;
hypersensitivity to antibiotics of the quinolone group.
Side effects
Side effects
In clinical trials of moxifloxacin in dosage form for use in ophthalmology, 2,252 patients received the study drug at 1 drop up to 8 times/day, 1,900 of whom received moxifloxacin in a 1-drop regimen 3 times/day.
The population for the safety evaluation included 1,389 patients in the United States and Canada, 586 patients in Japan and 277 patients in India. No serious adverse events have been reported in the clinical trials, either in the visual organ or in the body as a whole.
The most common adverse reactions associated with treatment were eye irritation and eye pain, with a cumulative incidence ranging from 1% to 2%.
In 96% of patients, the severity of these reactions was mild, while in one patient participating in the study, the severity of the adverse event led to the termination of participation in the study.
The following adverse reactions are classified according to the following frequency gradation: Very common (>1/10); common (>1/100, <1/10); infrequent (>1/1000, <1/100), rare (>1/10 000, <1/1000), and very rare (less than 1/10 000).
Hematopoietic system: rare – decrease in hemoglobin.
The immune system: frequency is unknown – hypersensitivity.
Nervous system disorders: infrequent – headache; rare – paresthesia; frequency unknown – dizziness.
An organ of vision: frequent – eye pain, eye irritation; infrequent – pitting keratitis, dry eye syndrome, subconjunctival hemorrhage, eye itching, conjunctival injection, eyelid edema, eye discomfort; rare – corneal epithelium defect, corneal disorders, conjunctivitis, blepharitis, conjunctival edema, blurred vision, reduced visual acuity, asthenopia, erythema of eyelids; frequency unknown – endophthalmitis, ulcerative keratitis, corneal erosion, increased intraocular pressure, corneal opacity, corneal edema, corneal infiltrates, corneal deposits, allergic eye symptoms, keratitis, corneal edema, photophobia, lacrimation, eye discharge, foreign body feeling in eyes.
Cardiovascular system: frequency is unknown – feeling of palpitations.
Respiratory system: rare – nasal discomfort, pain in the throat and pharynx, feeling of a foreign body in the throat; frequency unknown – shortness of breath.
The digestive system: infrequent – dysgeusia; rare – vomiting, increased aminotransferase activity and GGT; frequency unknown – nausea.
Skin and subcutaneous fatty tissue: frequency unknown – erythema, rash, urticaria, itching.
Description of individual adverse reactions
There have been reports of tears of the tendons of the shoulder joint, hand joints, Achilles tendon, and other tendons, which resulted in long-term disability or required surgical intervention.
These phenomena have been noted in patients receiving systemic therapy with fluoroquinolones. According to clinical studies and post-registration use, the risk of tendon ruptures during systemic therapy with fluoroquinolones may increase when corticosteroids are included in the therapy regimen, and elderly patients are at particular risk. Most often, damage affects tendons of supporting joints, including Achilles tendons.
Performance in children
In clinical trials with children, including infants, the safety profile of moxifloxacin in the form of instillation was demonstrated to be similar to the adult population. In patients under 18 years of age the most frequently observed were eye pain and eye irritation with an incidence of about 0.9%.
The results of clinical studies in the pediatric population showed no differences from the adult population in the profile of adverse events and their severity.
Overdose
Overdose
Due to the small capacity of the conjunctival cavity the possibility of local overdose when using the drug in the form of instillation is virtually absent.
The total moxifloxacin content of the drug is too low to develop adverse events if the contents of the bottle are accidentally swallowed.
Similarities
Similarities
Additional information
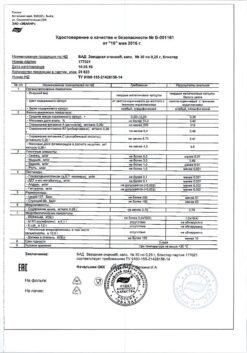
| Manufacturer | C.O.Rompharm Company S.R.L., Romania |
|---|---|
| Medication form | eye drops |
| Brand | C.O.Rompharm Company S.R.L. |
Related products
Buy Maxiflox, eye drops 5 mg/ml 5 ml with delivery to USA, UK, Europe and over 120 other countries.