No products in the cart.
Maruksa, 10 mg 30 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Stroke sequelae, Attention and memory disorders, Alcoholism, Concussion and other brain injuries, Alzheimer’s disease, Acquired dementia
Treatment of patients with moderate to severe Alzheimer’s disease.
Indications
Indications
Treatment of patients with moderate to severe Alzheimer’s disease.
Pharmacological effect
Pharmacological effect
dementia treatment
Special instructions
Special instructions
Epilepsy, thyrotoxicosis, predisposition to the development of seizures, simultaneous use of NMDA receptor antagonists (amantadine, ketamine, dextromethorphan), factors that increase urine pH (sudden change of diet, for example, switching to vegetarianism, heavy intake of alkaline gastric buffers), renal tubular acidosis, severe urinary tract infections caused by Proteus spp., myocardial infarction (history), heart failure III-IV functional class according to the NYHA classification, uncontrolled arterial hypertension, renal failure, liver failure.
Contraindicated for persons under 18 years of age.
Elderly patients (over 65 years old)
No dose adjustment is required.
Renal dysfunction
In patients with a creatinine clearance (CC) of 50-80 ml/min, no dose adjustment is required. For patients with moderate renal failure (creatinine clearance 30-49 ml/min), 10 mg/day is recommended. If the drug is well tolerated within 7 days, the dose can be increased to 20 mg/day according to the standard regimen. In patients with severe renal failure (creatinine clearance 5-29 ml/min), the daily dose should be 10 mg/day.
Liver dysfunction
In patients with mild to moderate liver dysfunction (Class A and B on the Child-Pugh scale), no dose adjustment is required.
It is recommended to use with caution in patients with epilepsy, a history of seizures, or in patients with a predisposition to epilepsy.
Concomitant use of memantine and NMDA receptor antagonists such as amantadine, ketamine or dextromethorphan should be avoided. These compounds act on the same receptor system as memantine, therefore adverse reactions (mainly related to the central nervous system) may occur more frequently and be more severe.
The presence of factors in the patient that influence the increase in urine pH (abrupt dietary changes, for example, a transition from a diet that includes animal products to a vegetarian diet or intensive consumption of alkaline gastric buffers), as well as renal tubular acidosis or severe urinary tract infections caused by Proteus spp., require careful monitoring of the patient’s condition.
From most clinical studies, patients with a history of myocardial infarction, decompensated chronic heart failure (NYHA functional class III-IV) or uncontrolled arterial hypertension were excluded. Therefore, data on the use of memantine in such patients is limited; the drug should be taken under close medical supervision.
Patients with Alzheimer’s disease in the stages of moderate to severe dementia usually have impaired ability to drive vehicles and operate complex machinery. In addition, memantine may cause changes in the reaction rate, so patients should refrain from driving vehicles or operating complex machinery.
Active ingredient
Active ingredient
Memantine
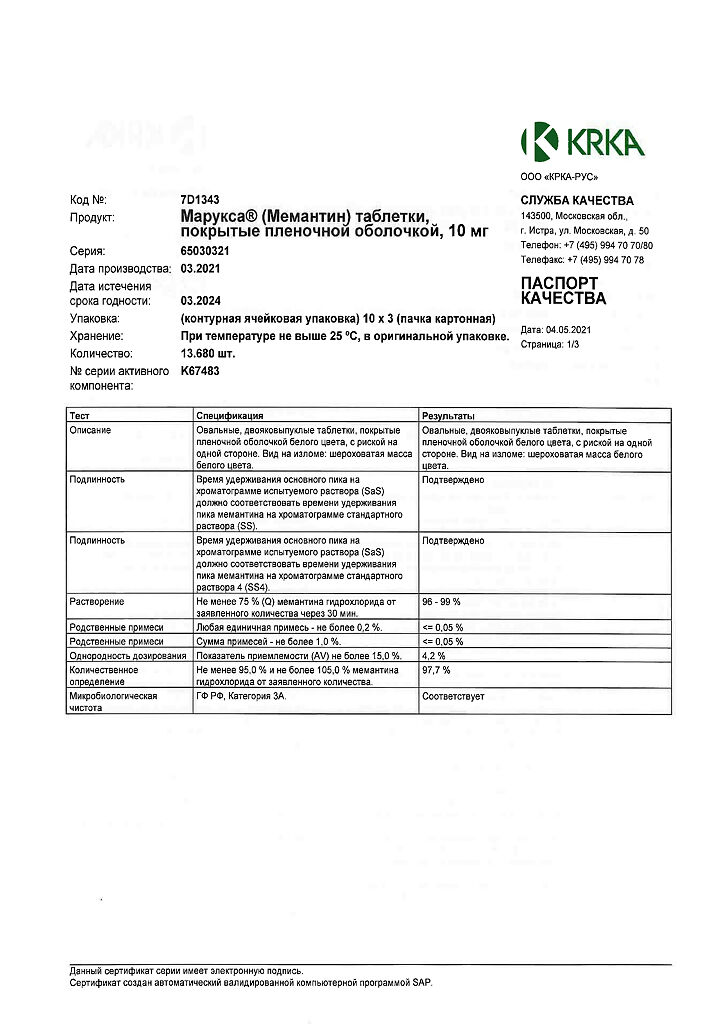
Composition
Composition
for 1 tablet
Core:
Active ingredient:
Memantine hydrochloride 10.00 mg
Excipients: lactose monohydrate, microcrystalline cellulose, colloidal silicon dioxide, talc, magnesium stearate
Film shell: methacrylic acid and ethyl acrylate copolymer (1: 1), 30% aqueous dispersion1, talc, triacetin, simethicone
1 30% aqueous dispersion contains, in addition to methacrylic acid and ethyl acrylate copolymer, also sodium lauryl sulfate and polysorbate-80 as emulsifiers.
Pregnancy
Pregnancy
Due to possible intrauterine growth retardation, Maruxa® is not used during pregnancy.
There is no information about the excretion of memantine in breast milk. However, given the lipophilicity of memantine, isolation is possible. Therefore, breastfeeding should be stopped during treatment with Maruxa®.
Contraindications
Contraindications
Hypersensitivity to memantine and other components of the drug.
Severe liver failure (class C on the Child-Pugh scale).
Pregnancy and breastfeeding period.
Age up to 18 years (efficacy and safety have not been established).
Lactase deficiency, lactose intolerance, glucose-galactose malabsorption syndrome, since Maruxa® contains lactose.
Side Effects
Side Effects
World Health Organization (WHO) side effect frequency classification:
very common ≥ 1/10
often ≥ 1/100 to < 1/10
uncommon ≥ 1/1000 to < 1/100
rarely from ≥ 1/10000 to < 1/1000
very rare <1/10000
frequency unknown cannot be estimated from available data.
In clinical studies involving 1,784 patients treated with memantine and 1,595 patients treated with placebo, the overall incidence of adverse reactions did not differ between memantine and placebo. They were generally mild to moderate in severity. The most common adverse reactions in the memantine group compared with placebo were: dizziness (6.3% vs. 5.6%, respectively), headache (5.2% vs. 3.9%), constipation (4.6% vs. 2.6%), somnolence (3.4% vs. 2.2%, respectively), and hypertension (4.1% vs. 2.8%, respectively).
Side effects are presented in table form according to the MedDRA classification:
Infectious and parasitic diseases
Uncommon
Fungal infections
Blood and lymphatic system disorders
Frequency unknown
Agranulocytosis, leukopenia (including neutropenia), pancytopenia, thrombocytopenia, thrombocytopenic purpura
Immune system disorders
Often
Hypersensitivity to the components of the drug
Mental disorders
Often
Drowsiness
Uncommon
Confusion
Hallucinations1
Frequency unknown
Psychotic reactions
Nervous system disorders
Often
Dizziness, imbalance
Uncommon
Gait disturbance
Very rarely
Convulsions
Heart disorders
Uncommon
Heart failure
Vascular disorders
Often
Increased blood pressure
Uncommon
Venous thrombosis/thromboembolism
Respiratory, thoracic and mediastinal disorders
Often
Dyspnea
Digestive system disorders
Often
Constipation
Uncommon
Nausea, vomiting
Frequency unknown
Pancreatitis
Disorders of the liver and biliary tract
Often
Increased activity of liver enzymes
Frequency unknown
Hepatitis
Renal and urinary tract disorders
Frequency unknown
Acute renal failure
Skin and subcutaneous tissue disorders
Frequency unknown
Stevens-Johnson syndrome
General and administration site disorders
Often
Headache
Uncommon
Fatigue
1Hallucinations have been observed mainly in patients with Alzheimer’s disease at the stage of severe dementia.
With post-registration use, the following adverse reactions have been reported: dizziness, drowsiness, increased excitability, increased fatigue, anxiety, increased intracranial pressure, nausea, hallucinations, headache, impaired consciousness, muscle hypertonicity, gait disturbance, depression, convulsions, psychotic reactions, suicidal thoughts, constipation, nausea, pancreatitis, candidiasis, increased blood pressure, vomiting, cystitis, increased libido, venous thrombosis, thromboembolism and allergic reactions.
Interaction
Interaction
The effects of levodopa, dopamine receptor agonists and anticholinergic drugs are potentiated.
The effectiveness of barbiturates and antipsychotic (neuroleptic) drugs decreases with the simultaneous use of memantine.
The simultaneous use of memantine with dantrolene and baclofen, as well as with antispasmodics, may be accompanied by a change in their effect, which requires dose adjustment of these drugs.
The simultaneous use of memantine and amantadine should be avoided due to the risk of developing psychosis. Memantine and amantadine belong to the group of NMDA receptor antagonists. The risk of developing psychosis is also increased when memantine is used concomitantly with phenytoin, ketamine and dextromethorphan.
When used simultaneously with cimetidine, ranitidine, procainamide, quinidine, quinine and nicotine, the risk of increasing the concentration of memantine in the blood plasma increases.
When taken simultaneously with hydrochlorothiazide, it is possible to reduce the concentration of hydrochlorothiazide in the blood plasma due to an increase in its excretion from the body.
It is possible to increase the international normalized ratio (INR) in patients simultaneously taking oral indirect anticoagulants (warfarin). It is recommended to regularly monitor prothrombin time or INR. Concomitant use with antidepressants, selective serotonin reuptake inhibitors and monoamine oxidase inhibitors requires careful monitoring of patients.
No drug interactions were observed with single simultaneous use of memantine with glibenclamide/metformin or donepezil in healthy volunteers.
When used simultaneously with memantine, there were no changes in the pharmacokinetics of galantamine in healthy volunteers.
In vitro, memantine does not inhibit CYP isoenzymes 1A2, 2A6, 2C9, 2D6, 2E1, 3A, flavin-containing monooxygenase, epoxide hydrolase, or sulfation.
Overdose
Overdose
Symptoms: increased severity of side effects, such as fatigue, weakness, diarrhea, confusion, drowsiness, dizziness, agitation, hallucinations, gait disturbance, nausea.
In the most severe case of overdose (2000 mg of memantine), the patient survived, but adverse reactions from the nervous system were observed (coma for 10 days, then diplopia and agitation). The patient received symptomatic treatment and plasmapheresis. The patient recovered without further complications. In another case of severe overdose (400 mg), the patient also survived and recovered. Adverse reactions from the central nervous system have been described: anxiety, psychosis, visual hallucinations, convulsive readiness, drowsiness, stupor and loss of consciousness.
Treatment: in case of overdose, treatment is symptomatic. There is no specific antidote. It is necessary to carry out standard therapeutic measures aimed at removing the active substance from the stomach, for example, gastric lavage, taking activated charcoal, acidifying urine, and possibly forced diuresis.
Clinical pharmacology
Clinical pharmacology
Pharmacodynamics
Adamantane derivative. It is a non-competitive antagonist of N-methyl-D-aspartate (NMDA) receptors and has a modulating effect on the glutamatergic system. Regulates ion transport, blocks calcium channels, normalizes membrane potential, improves the process of nerve impulse transmission. Improves cognitive processes, increases daily activity.
Pharmacokinetics
Suction
Quickly and completely absorbed after oral administration. The maximum concentration (Cmax) in blood plasma is achieved within 3-8 hours after oral administration. In patients with normal renal function, no accumulation of memantine was observed.
Distribution
When taken daily at a dose of 20 mg per day, the equilibrium concentrations of memantine in the blood plasma are 70-150 ng/ml. When using a daily dose of 5-30 mg, the ratio of the average concentration in the cerebrospinal fluid to the concentration in the blood plasma was calculated to be 0.52. The volume of distribution is approximately 10 l/kg. About 45% of memantine binds to blood plasma proteins.
Metabolism
About 80% of memantine taken orally is excreted unchanged. The main metabolites N-3,5-dimethyl-gludantan, an isomeric mixture of 4- and 6-hydroxy-memantine and 1-nitroso-3-5-dimethyl-adamantane do not have their own pharmacological activity. Under in vitro conditions, metabolism carried out by isoenzymes of the cytochrome P450 system was not detected. In a study of oral 14C-memantine, an average of 84% of the oral dose was eliminated within 20 days, with more than 99% excreted by the kidneys.
Withdrawal
Excreted from the body mono-exponentially. The half-life (T½) of the terminal phase ranges from 60 to 100 hours. It is excreted by the kidneys. In volunteers with normal renal function, the total clearance is 170 ml/min/1.73 m2, part of the total renal clearance is achieved through tubular secretion. Renal excretion also involves tubular reabsorption, possibly mediated by cationic transport proteins. The rate of renal elimination of memantine in conditions of alkaline urine reaction can be reduced by 7-9 times. Alkalinization of urine can be caused by a sudden change in diet, such as switching from a diet containing animal products to a vegetarian diet, or due to intensive use of alkaline gastric buffers.
Linearity
Studies conducted in volunteers showed linearity of pharmacokinetics in the dose range of 10-40 mg.
Pharmacokinetic/pharmacodynamic dependence
When using memantine at a dose of 20 mg/day, the concentration level in the cerebrospinal fluid corresponds to the value of the inhibition constant (ki), which for memantine is 0.5 µmol in the area of the frontal cortex.
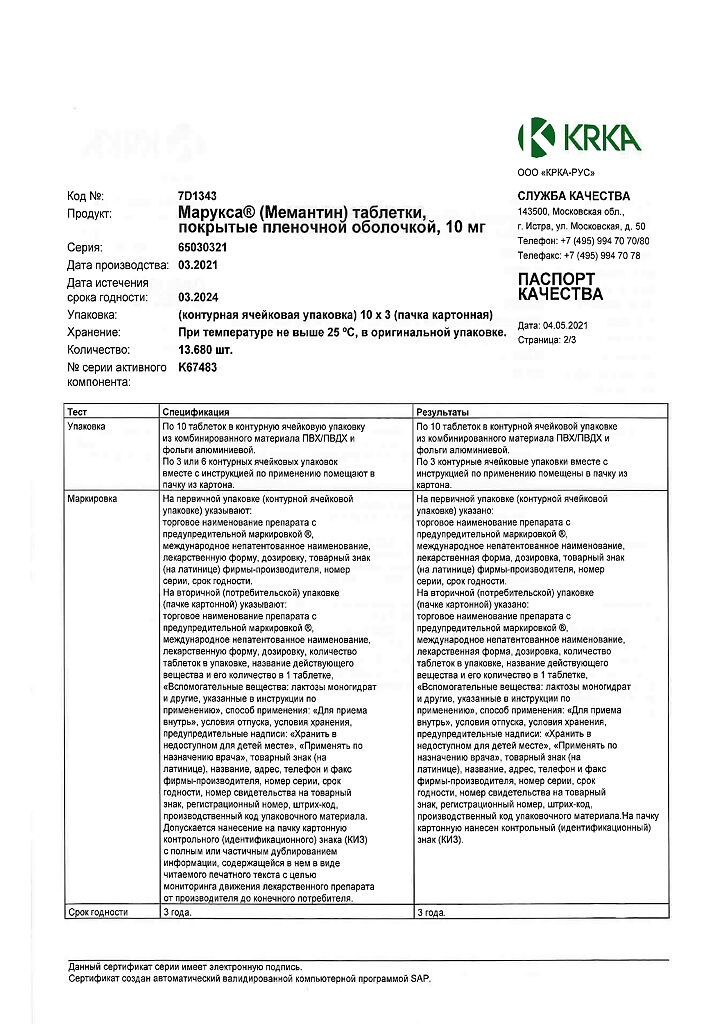
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C, in the original packaging.
Keep out of the reach of children.
Shelf life
Shelf life
2 years.
Do not use the drug after the expiration date.
Manufacturer
Manufacturer
KRKA-RUS, Russia
Additional information
| Shelf life | 2 years. Do not use the drug after the expiration date. |
|---|---|
| Conditions of storage | At the temperature not more than 25 °С, in the original package. Keep out of reach of children. . |
| Manufacturer | KRKA-RUS, Russia |
| Medication form | pills |
| Brand | KRKA-RUS |
Other forms…
Related products
Buy Maruksa, 10 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.