No products in the cart.
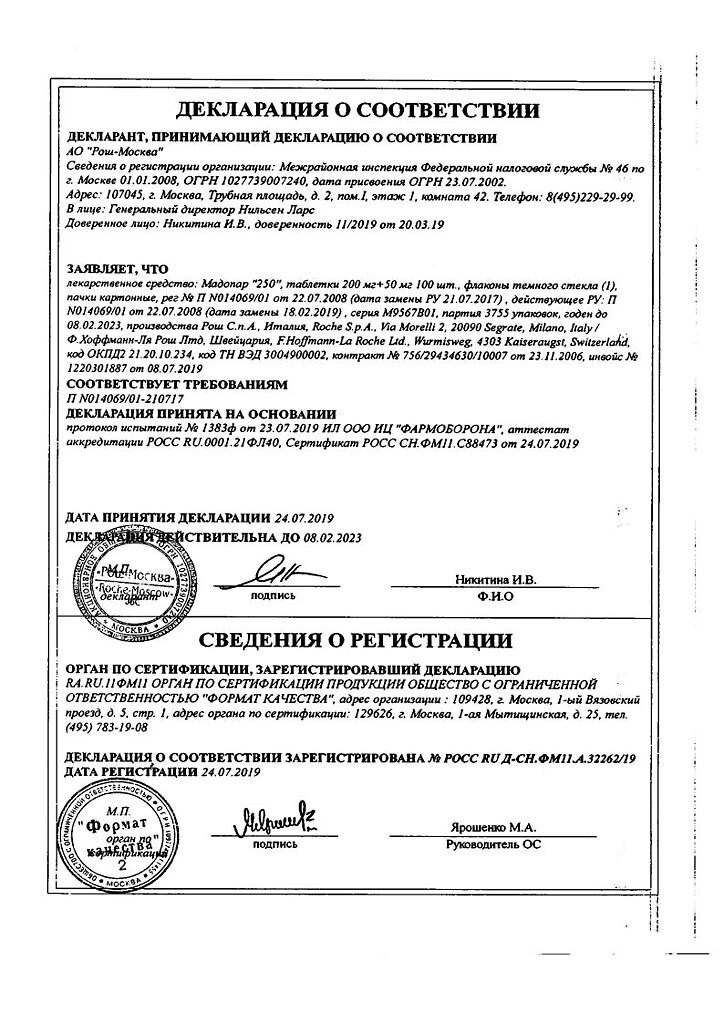
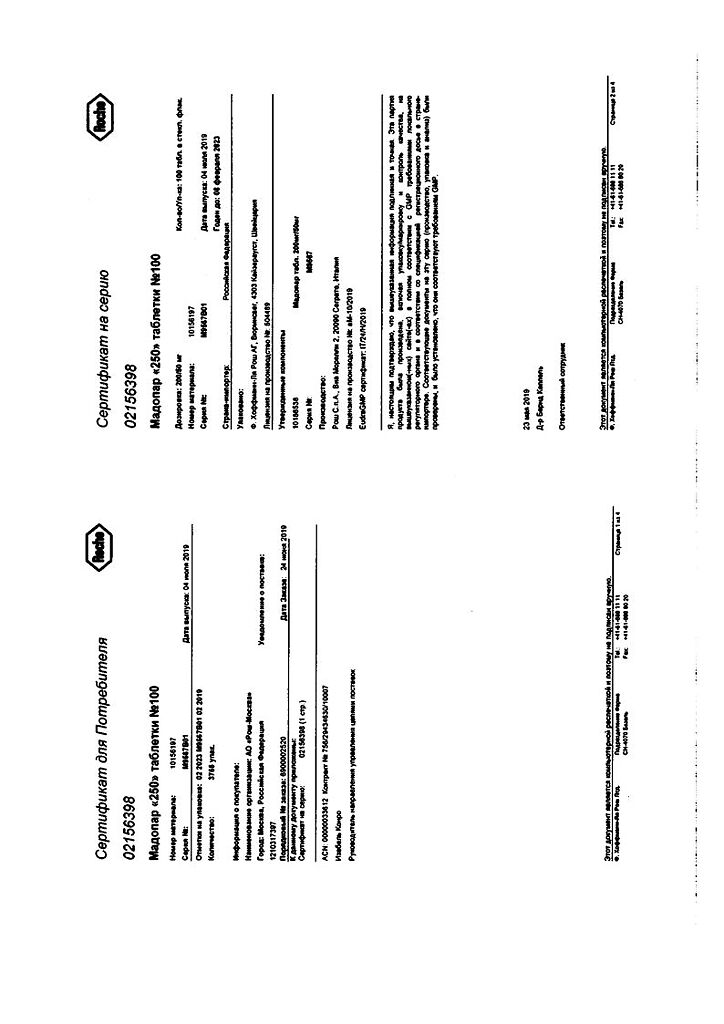
Madopar, tablets 250 mg, 100 pcs.
€1.00
Out of stock
(E-mail when Stock is available)
Description
A combined anti-Parkinsonian drug containing dopamine precursor and peripheral decarboxylase inhibitor.
In parkinsonism, the brain neurotransmitter dopamine is produced in insufficient amounts in the basal ganglia. Levodopa, or L-DOPA – (3,4-dihydrophenylalanine), is a metabolic precursor of dopamine and, unlike the latter, penetrates well through the BBB. After levodopa penetrates the CNS, it is converted to dopamine by aromatic acid decarboxylase.
Parkinson’s disease
After ingestion, levodopa is rapidly decarboxylated to dopamine in both cerebral and extracerebral tissues. As a result, most of the levodopa administered does not reach the basal ganglia, and peripheral dopamine often causes adverse reactions. Consequently, it is necessary to block extracerebral decarboxylation of levodopa. This is achieved by simultaneous administration of levodopa and benserazide, a peripheral decarboxylase inhibitor.
Madopar is a 4:1 combination of these agents, which is optimal and has the same efficacy as levodopa at high doses.
The fast acting (dispersible) tablets are especially indicated for patients with dysphagia and those who need a quicker onset of action.
The GSS capsules are a special dosage form with delayed release of the active ingredients in the stomach. Maximum plasma concentrations are 20-30% lower than those of Madopar “125” capsules and Madopar “250” tablets and are reached 3 hours after intake.
Restless Leg Syndrome
The exact mechanism of Restless Leg Syndrome is unknown, but the dopaminergic system plays an important role in the pathogenesis of this syndrome.
Indications
Indications
Parkinson’s disease, including:
– in patients with dysphagia, early morning and afternoon akinesia, patients with phenomena of “single dose effect depletion” or “increased latency period before onset of clinical drug effect” (Madopar “125” fast acting tablets (dispersible));
– in patients with any type of levodopa action variation, namely “peak dose dyskinesia” and “end-of-dose phenomenon,” such as immobility at night (Madopar GSS “125”).
Troubled legs syndrome:
– Idiopathic restless legs syndrome;
– Restless legs syndrome in patients with chronic renal failure on dialysis.
Active ingredient
Active ingredient
Composition
Composition
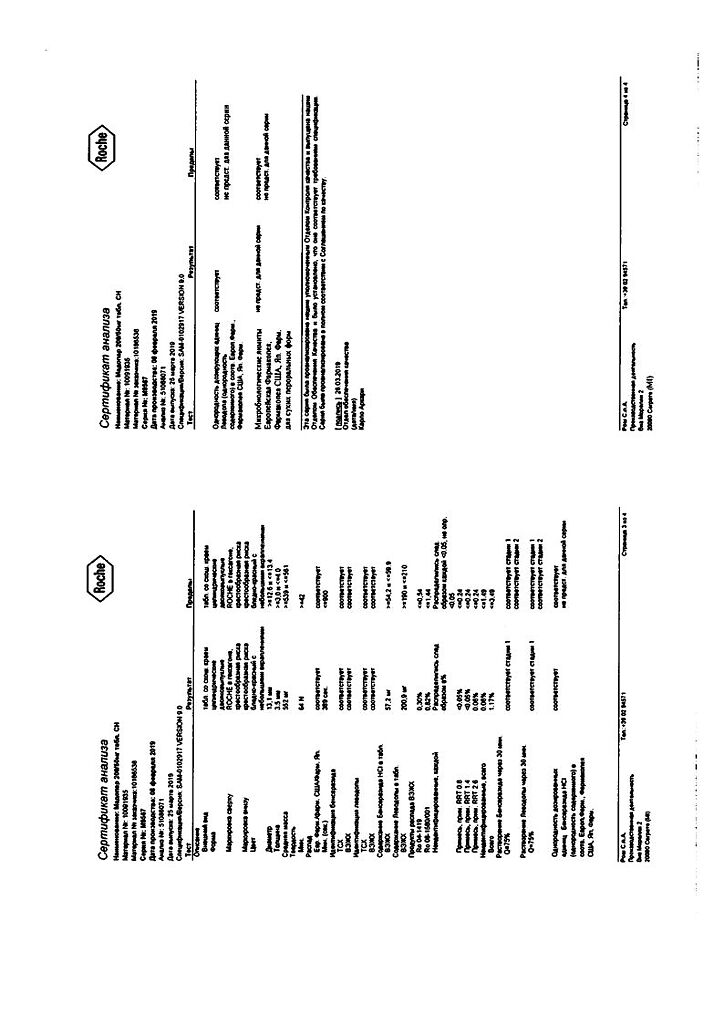
Levodopa – 200 mg, benserazide hydrochloride – 57 mg, which corresponds to the content of benserazide – 50 mg
Auxiliary substances:
mannitol – 103.2 mg,
calcium hydrophosphate – 100 mg,
microcrystalline cellulose – 38.6 mg,
corn starch pregelatinized – 20 mg,
crospovidone – 20 mg,
How to take, the dosage
How to take, the dosage
Treatment should be started gradually, adjusting doses individually until optimal therapeutic effect is achieved.
Madopar “250” tablets can be crushed to make swallowing easier.
Parkinson’s disease
Standard dosing regimen
Orally, at least 30 minutes before or 1 hour after meals.
Initial therapy
In the early stage of Parkinson’s disease, it is recommended to start treatment with Madopar at a dose of 62.5 mg (50 mg levodopa + 12.5 mg benserazide 3-4 times daily). If tolerated well, the dose should be gradually increased, depending on the patient’s response.
The optimal effect is usually achieved with a daily dose of 300-800 mg levodopa + 75-200 mg benserazide, taken in 3 or more doses. It may take 4 to 6 weeks to achieve optimal effect. Further increases in the daily dose, if necessary, should be made at 1-month intervals.
Supportive therapy
The average maintenance dose is 125 mg (100 mg levodopa + 25 mg benserazide) of Madopar 3-6 times daily. The frequency of administration (at least 3 times) during the day should be distributed to ensure optimal effect. To optimize the effect, Madopar “125” in the form of regular capsules and Madopar “250” in the form of regular tablets may need to be replaced with Madopar “125” fast acting tablets (dispersible) or Madopar GSS “125”.
Troubled legs syndrome
The drug should be taken 1 h before bedtime, with a small amount of food. The maximum daily dose is 500 mg of Madopar (400 mg of levodopa + 100 mg of benserazide).
Idiopathic restless legs syndrome with sleep disturbances
Madopar “125” capsules or Madopar “250” tablets are recommended.
The starting dose is 62.5-125 mg. If the effect is insufficient, the dose of Madopar should be increased to 250 mg (200 mg levodopa + 50 mg benserazide).
Idiopathic restless legs syndrome with sleep and sleep disorders
The initial dose is 1 capsule of Madopar GSS “125” and 1 capsule of Madopar “125” 1 h before sleep. If the effect is insufficient, the dose of Madopar GSS “125” should be increased to 250 mg (2 capsules).
Idiopathic restless legs syndrome with disorders of falling asleep and sleep, as well as disorders during the day
Optional: 1 tablet dispersible or 1 capsule of Madopar “125”, maximum daily dose of Madopar is 500 mg (400 mg levodopa and 100 mg benserazide).
Troubled Leg Syndrome in patients with chronic renal failure receiving dialysis
The drug is prescribed in dose of 125 mg (1 dispersible tablet or 1 capsule of Madopar “125”) 30 min before dialysis.
Dosing regimen in special cases
Parkinson’s disease
Madopar may be combined with other anti-Parkinsonian agents. However, as treatment continues, it may be necessary to reduce the dose of other medications or to phase them out gradually.
Madopar “125” fast acting tablets (dispersible) are a special dosage form for patients with dysphagia or akinesia in the early morning and afternoon hours or for patients with “single dose effect attrition” or “increased latency period before onset of clinical effect of the drug” phenomenon.
If a patient has severe motor fluctuations throughout the day (single-dose attrition, on-off phenomenon), either more frequent and correspondingly lower single doses or, preferably, Madopar GSS “125” are recommended.
The switch to Madopar GSS “125” is best made from one day to the next, starting with the morning dose. You should keep the same daily dose and dosing regimen as with Madopar “125” and Madopar “250”.
After 2-3 days, the dose is gradually increased by about 50%. Patients should be warned that their condition may worsen temporarily. Because of the peculiarities of the dosage form, Madopar GSS “125” starts to work somewhat later.
The clinical effect can be achieved more quickly by prescribing Madopar GSS “125” together with Madopar “125” capsules or Madopar “125” fast acting tablets (dispersible). This may be optimal as a first morning dose, which should be slightly higher than subsequent doses.
The dose of Madopar GSS “125” should be adjusted slowly and carefully, with an interval of at least 2-3 days between dose changes.
In patients with nighttime symptoms, a positive effect was achieved by gradually increasing the evening dose of Madopar GSS “125” to 250 mg (2 capsules) before bedtime.
In severe Madopar GSS “125” effects (dyskinesia), increasing the intervals between doses is more effective than decreasing the single dose.
If Madopar GSS “125” is not effective enough, then it is recommended to return to the previous treatment with Madopar “125”, Madopar “250” or Madopar “125” fast acting tablets (dispersible).
In prolonged therapy, episodes of “freezing”, “depletion phenomenon” of the “on-off” phenomenon may occur. In case of “freezing” episodes and “phenomenon of exhaustion” the drug dose is split (reduction of the single dose or reduction of the interval between doses of the drug), and in case of “on-off” phenomenon – to increase the single dose while reducing the number of doses. Subsequently, we may try increasing the dose again to increase efficacy.
In patients with mild to moderate renal insufficiency, no dose adjustment is required. Madopar is well tolerated by patients receiving hemodialysis sessions.
Troubled Leg Syndrome
To rule out an increase in restless leg syndrome symptoms (early onset during the day, increased severity and involvement of other body parts), the daily dose should not exceed the recommended maximum dose of Madopar of 500 mg (400 mg levodopa + 100 mg benserazide).
If clinical symptoms increase, the dose of levodopa should be reduced or levodopa withdrawn gradually and other therapy prescribed.
Interaction
Interaction
Pharmacokinetic interaction
Concomitant use of trihexyphenidyl (an anticholinergic drug) decreases the rate, but not the degree of absorption of levodopa. Administration of trihexyphenidyl together with Madopar GSS “125” does not affect the pharmacokinetics of levodopa.
The degree of absorption of levodopa is reduced by 32% when concomitant use of antacids with Madopar GSS.
Iron sulfate decreases plasma Cmax and AUC values of levodopa by 30-50%; these changes are clinically significant in some cases.
Methoclopramide increases the rate of absorption of levodopa.
Levodopa does not interact pharmacokinetically with bromocriptine, amantadine, selegiline and domperidone.
Pharmacodynamic interactions
Neuroleptics, opioids and antihypertensive drugs containing reserpine inhibit the effects of Madopar.
If it is necessary to prescribe Madopar to patients receiving non-reversible non-selective MAOI inhibitors, at least 2 weeks should elapse between stopping the MAOI inhibitor and starting Madopar.
Selective type B MAO inhibitors (including selegiline, rasagiline) and selective type A MAO inhibitors (moclobemide) may be prescribed against treatment with Madopar. At that, it is recommended to adjust levodopa dose depending on individual patient’s need in terms of efficacy and tolerability. The combination of MAO type A and MAO type B inhibitors is equivalent to taking a non-selective MAO inhibitor, therefore this combination should not be prescribed simultaneously with Madopar.
Madopar should not be prescribed concomitantly with sympathomimetics (adrenaline, norepinephrine, isoproterenol, amphetamine) because levodopa may potentiate their effects. If concomitant administration is still necessary, the cardiovascular status should be monitored carefully and the dose of sympathomimetics should be reduced if necessary.
The drug may be combined with other anti-Parkinsonian drugs (anticholinergic agents, amantadine, dopamine agonists), which may increase not only desirable but also undesirable effects. It may be necessary to reduce the dose of Madopar or another drug.
If Madopar is used concomitantly with a COMT inhibitor, it may be necessary to reduce the dose of Madopar. If treatment with Madopar is initiated, anticholinergic medications should not be abruptly withdrawn because levodopa does not take effect immediately.
Because patients receiving Madopar may experience BP fluctuations and arrhythmias during halothane anesthesia, Madopar should be discontinued 12-48 h before surgical intervention.
Levodopa may affect the results of laboratory determination of catecholamines, creatinine, uric acid and glucose, and a false positive Coombs test is possible.
In patients receiving Madopar, taking the drug concomitantly with protein-rich foods may impair gastrointestinal absorption of levodopa.
Special Instructions
Special Instructions
In persons with hypersensitivity to the drug, appropriate reactions may develop.
Gastrointestinal adverse reactions, which may occur at the beginning of treatment, are largely eliminated if Madopar® is taken with small amounts of food or liquids and if the dose is increased slowly.
Patients with open-angle glaucoma should have their intraocular pressure measured regularly because, in theory, levodopa may increase intraocular pressure.
In patients taking levodopa, periodic monitoring of blood count, liver function, and renal function is recommended.
Patients with diabetes mellitus should frequently monitor blood glucose levels and adjust the dose of hypoglycemic drugs.
If possible, administration of Madopar should be continued as long as possible before general anesthesia, with the exception of halothane anesthesia. Because patients receiving Madopar® may experience BP fluctuations and arrhythmias during halothane anesthesia, Madopar should be discontinued 12-48 h before the surgical intervention. After surgery, treatment is resumed, gradually increasing the dose to the previous level.
Madopar® should not be abruptly withdrawn. Abrupt withdrawal of the drug may lead to the development of a malignant neuroleptic syndrome (fever, muscle rigidity, and possible psychiatric changes and increase in serum CPK), which may take a life-threatening form. If these symptoms occur, the patient should be monitored by a physician (hospitalization if necessary) and receive appropriate symptomatic therapy, which may include re-prescribing Madopar after appropriate evaluation of the patient’s condition.
Depression may be a clinical manifestation of an underlying disease (parkinsonism, restless legs syndrome) and may also occur with Madopar therapy. Patients taking Madopar® should be closely monitored for possible psychiatric adverse reactions.
In some patients with Parkinson’s disease, behavioral and cognitive impairment have been noted as a result of uncontrolled use of increasing doses of the drug despite physician recommendations and significant exceeding of therapeutic doses of the drug.
The effect on driving and operating machinery
In case of drowsiness, sudden episodes of somnolence, the patient should refrain from driving or operating machinery. If these symptoms occur, dose reduction or discontinuation of therapy should be considered.
Contraindications
Contraindications
– Decompensated disorders of the endocrine system;
– decompensated liver function disorder;
– decompensated renal function disorder (except for patients with the syndrome “restless legs” receiving dialysis);
– cardiovascular system diseases in decompensation stage;
– mental illness with a psychotic component;
– Closed-angle glaucoma;
– concomitant use with non-selective MAO inhibitors, combination of MAO type A and MAO type B inhibitors;
– aged up to 25 years;
– Women of childbearing age who do not use reliable contraceptive methods;
– Pregnancy;
– Lactation (breastfeeding);
– Hypersensitivity to the preparation components.
Side effects
Side effects
CNS and peripheral nervous system disorders: agitation, anxiety, insomnia, hallucinations, delirium, temporary disorientation (especially in elderly patients and in patients with indication of these symptoms in the anamnesis), depression, headache, dizziness, in later stages of treatment sometimes – spontaneous movements (like chorea or athetosis), episodes of “freezing”, weakening of the effect by the end of the dose period (phenomenon of “exhaustion”), “on-off” phenomenon, pronounced somnolence, episodes of sudden somnolence, increased manifestations of “restless legs” syndrome.
Digestive system disorders: nausea, vomiting, diarrhea; in some cases – loss or change of taste sensation, dryness of the oral mucosa.
Cardiovascular system: arrhythmias, orthostatic hypotension (weakens after reduction of the dose of Madopar), arterial hypertension.
Respiratory system: rhinitis, bronchitis.
Hematopoietic system disorders: rarely – hemolytic anemia, transient leukopenia, thrombocytopenia.
Dermatological reactions: rare – itching, rash.
Laboratory parameters: sometimes – transient increase of liver transaminases activity, alkaline phosphatase, increase of gamma-glutamyl transpeptidase, increase of blood urea nitrogen, change of urine color to red, darker when standing.
Body in general: anorexia.
Others: febrile infection.
Overdose
Overdose
Symptoms: worsening manifestations of side effects – arrhythmia, confusion, insomnia, nausea and vomiting, abnormal involuntary movements. When taking the drug form with modified release of active substances (Madopar GSS “125”) in the stomach, the appearance of symptoms may be delayed.
Treatment:Symptomatic therapy – respiratory analeptics, antiarrhythmic agents, neuroleptics; vital functions should be monitored. When using the dosage form with modified release of active substances (Madopar GSS “125”) further absorption of the drug should be prevented.
.
Pregnancy use
Pregnancy use
Madopar is contraindicated in pregnancy and in women of childbearing age who do not use reliable methods of contraception because of the possible disturbance of skeletal development in the fetus.
If pregnancy occurs during treatment with Madopar, the drug should be stopped immediately as recommended by the treating physician.
It is not known whether benserazide is excreted with the breast milk. If it is necessary to use Madopar during lactation, breastfeeding should be stopped, because skeletal development disorders in the child cannot be excluded.
Additional information
| Shelf life | 4 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C |
| Manufacturer | F. Hoffmann-La Roche Ltd, Switzerland |
| Medication form | pills |
| Brand | F. Hoffmann-La Roche Ltd |
Related products
Buy Madopar, tablets 250 mg, 100 pcs. with delivery to USA, UK, Europe and over 120 other countries.