No products in the cart.
Lozartan 100 mg, 90 pcs.
€1.00
Out of stock
(E-mail when Stock is available)
Description
Angiotensin II is a potent vasoconstrictor, the main active hormone of the renin-angiotensin-aldosterone system (RAAS), and a crucial pathophysiological link in the development of arterial hypertension (AH).
Angiotensin II binds to AT1 receptors located in many tissues (vascular smooth muscle tissues, adrenal glands, kidneys and heart) and has several important biological functions including vasoconstriction and aldosterone release. In addition, angiotensin II stimulates smooth muscle cell overgrowth. AT1 receptors are the second type of receptors that angiotensin II binds to, but its role in the regulation of cardiovascular function is unknown.
Lozartan is a selective angiotensin II AT1-receptor antagonist that is highly effective when taken orally. Losartan and its pharmacologically active carboxylated metabolite (E-3174) both in vitro and in vivo block all physiological effects of angiotensin II regardless of its source or synthesis pathway. Unlike some peptide angiotensin II antagonists, Losartan has no agonist properties.
Lozartan selectively binds to AT1 receptors and does not bind to or block receptors of other hormones and ion channels that play an important role in the regulation of cardiovascular function. In addition, losartan does not inhibit angiotensin-converting enzyme (ACE, kininase II), which is responsible for bradykinin degradation.
Therefore, effects not directly related to AT1-receptor blockade, such as increased bradykinin-mediated effects or development of edema (losartan 1.7%, placebo 1.9%) are unrelated to the action of losartan.
Lozartan suppresses the increase in systolic and diastolic blood pressure (BP) with angiotensin II infusion. The above effect of angiotensin II is inhibited by approximately 85% at the time of reaching maximum plasma concentration (Cmax) of losartan after administration of 100 mg, and by 26-39% after 24 hours of single and multiple doses.
While taking losartan, the elimination of the negative feedback of angiotensin II suppression of renin secretion leads to an increase in plasma renin activity (ARP). An increase in ARP leads to an increase in plasma angiotensin II concentration.
In long-term (6-week) treatment of patients with AH with losartan at a dose of 100 mg/day, a 2-3-fold increase in plasma angiotensin II concentrations at the time of reaching the Cmax of losartan was observed.
In some patients, even greater increases in angiotensin II concentrations were observed, especially with a short duration of treatment (2 weeks). Despite this, during treatment, antihypertensive effect and decrease of plasma aldosterone concentration were manifested after 2 and 6 weeks of therapy, indicating effective blockade of angiotensin II receptors. After discontinuation of losartan, ARP and angiotensin II concentrations decreased within 3 days to values observed before starting losartan.
Because losartan is a specific angiotensin II AT1-receptor antagonist, it does not inhibit ACE (kininase II), the enzyme that inactivates bradykinin.
A study comparing the effects of losartan at doses of 20 mg and 100 mg with those of an ACE inhibitor for effects on angiotensin I, angiotensin II, and bradykinin showed that losartan blocks the effects of angiotensin I and angiotensin II without affecting the effects of bradykinin. This is due to the specific mechanism of action of losartan. The ACE inhibitor blocked the response to angiotensin I and increased the severity of bradykinin-induced effects without affecting the severity of the response to angiotensin II, demonstrating the pharmacodynamic difference between losartan and ACE inhibitors.
Indications
Indications
– Arterial hypertension;
– Reducing the risk of associated cardiovascular morbidity and mortality in patients with arterial hypertension and left ventricular hypertrophy, as manifested by cumulative reductions in cardiovascular mortality, stroke and myocardial infarction rates;
– Renal protection in patients with type 2 diabetes mellitus with proteinuria – slowing the progression of renal failure, manifested by a decrease in the rate of hypercreatininemia, the rate of development of end-stage chronic renal failure requiring hemodialysis or kidney transplantation, mortality rates, and a decrease in proteinuria;
– chronic heart failure with ineffective treatment with ACE inhibitors or intolerance to ACE inhibitors. It is not recommended to transfer patients with heart failure and stable values while taking ACE inhibitors to therapy with losartan.
Active ingredient
Active ingredient
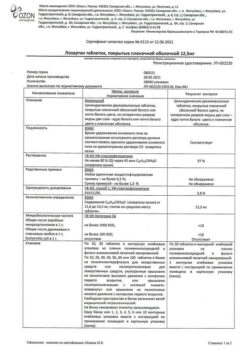
Composition
Composition
Active substance:
Potassium losartan – 100.0 mg;
Auxiliary substances:
Lactose monohydrate – 115.0 mg;
Microcrystalline cellulose – 40.0 mg;
croscarmellose sodium – 11.2 mg;
povidone K-17 (polyvinylpyrrolidone low molecular weight) – 9.0 mg;
silicon dioxide colloid – 2.0 mg;
Magnesium stearate – 2.8 mg;
Film coating:
[hypromellose – 4.8 mg, talc – 1.6 mg, titanium dioxide – 0.826 mg, macrogol 4000 (polyethylene glycol 4000) – 0.72 mg, iron oxide yellow dye – 0.054 mg] or [dry film coating mixture, containing hypromellose (60%), talc (20%), titanium dioxide (10.33%), macrogol 4000 (polyethylene glycol 4000) (9%), iron oxide yellow dye (0.67%)] – 8.0 mg.
How to take, the dosage
How to take, the dosage
Ingestion, regardless of the time of meals.
The drug can be taken in combination with other hypotensive drugs.
Hypertension
The standard starting and maintenance dose for most patients is 50 mg once daily. The maximum antihypertensive effect is reached after 3-6 weeks of therapy.
In some patients the dose may be increased to a maximum daily dose of 100 mg once daily for a greater effect.
In patients with reduced circulating blood volume (RBC) (e.g., when taking high-dose diuretics), the starting dose of losartan should be reduced to 25 mg once daily (see section “Special Precautions”).
There is no need to adjust the starting dose in elderly patients and in patients with impaired renal function, including patients on hemodialysis.
Patients with a history of liver disease are recommended to be prescribed lower doses of losartan.
Risk reduction of associated cardiovascular morbidity and mortality in patients with arterial hypertension and left ventricular hypertrophy
The standard starting dose of the drug is 50 mg once daily. Subsequently, it is recommended to add a low dose of hydrochlorothiazide or to increase the drug dose to a maximum daily dose of 100 mg once daily, taking into account the degree of BP reduction.
Renal protection in patients with type 2 diabetes mellitus and proteinuria
The standard initial dose of the drug is 50 mg once daily. Thereafter, the dose can be increased to a maximum daily dose of 100 mg once daily, taking into account the degree of BP reduction.
The drug may be prescribed in combination with other hypotensive agents (e.g., diuretics, slow calcium channel blockers, alpha- and beta-adrenoblockers, hypotensive agents of central action), insulin and other hypoglycemic agents (e.g., sulfonylurea derivatives, glitazones and glucosidase inhibitors).
Chronic Heart Failure
The starting dose of losartan for patients with chronic heart failure is 12.5 mg once daily. Generally, the dose is increased at weekly intervals (i.e., 12.5 mg/day, 25 mg/day, 50 mg/day, 100 mg/day to a maximum (for this indication only) dose of 150 mg once daily) depending on individual tolerance.
Interaction
Interaction
In clinical studies on pharmacokinetic drug interactions, there have been no clinically significant interactions of losartan with hydrochlorothiazide, digoxin, warfarin, cimetidine and phenobarbital.
Rifampicin, as an inducer of drug metabolism, reduces the blood concentration of the active metabolite losartan.
The use of two P450 3A4 isoenzyme inhibitors, ketoconazole and erythromycin, has been studied in clinical trials.
Ketoconazole had no effect on the metabolism of losartan to the active metabolite after intravenous administration of losartan, and erythromycin had no clinically significant effect when losartan was taken orally.
Fluconazole, a P450 2C9 isoenzyme inhibitor, reduces the concentration of the active metabolite of losartan, but the pharmacodynamic significance of concomitant use of losartan and P450 2C9 isoenzyme inhibitors has not been studied.
It has been shown that patients who do not metabolize losartan to an active metabolite have a very rare and specific defect in the P450 2C9 isoenzyme. These data suggest that the metabolism of losartan to the active metabolite is by the P450 2C9 isoenzyme rather than the P450 3A4 isoenzyme.
The concomitant use of losartan, as well as other drugs that block angiotensin II or its effects, with potassium-saving diuretics (e.g., spironolactone, eplerenone, triamterene, amiloride), potassium supplements or potassium salts may result in increased serum potassium levels.
Non-steroidal anti-inflammatory drugs (NSAIDs), including selective cyclooxygenase-2 (COX-2) inhibitors, may decrease the effect of diuretics and other hypotensive agents. Consequently, the antihypertensive effect of ARA II or ACE inhibitors may be weakened when used simultaneously with NSAIDs, including selective COX-2 inhibitors.
In some patients with impaired renal function (e.g., elderly patients or patients with dehydration, including those taking diuretics) receiving NSAID therapy, including selective COX-2 inhibitors, concomitant use of ARA II or ACE inhibitors may cause further impairment of renal function, including development of acute renal failure. These effects are usually reversible, so concomitant use of these drugs should be conducted with caution in patients with impaired renal function.
Simultaneous use of losartan with ACE inhibitors is contraindicated in patients with diabetic nephropathy and is not recommended in other patients.
Special Instructions
Special Instructions
Hypersensitivity reactions
In patients with a history of angioedema (edema of the face, lips, pharynx/larynx and/or tongue), monitoring of the drug is necessary.
Embryotoxicity
The use of drugs acting on the RAAS in the second and third trimesters of pregnancy reduces fetal renal function and increases morbidity and mortality of the fetus and newborns. The development of oligohydramnios may be associated with fetal lung hypoplasia and skeletal deformities. Possible adverse events in neonates include skull bone hypoplasia, anuria, arterial hypotension, renal failure, and death. If pregnancy is diagnosed, the drug should be withdrawn immediately.
Hypotension and electrolyte balance disorders or decreased circulating blood volume
Patients with decreased RBC (e.g., those treated with high doses of diuretics) may have symptomatic arterial hypotension. These conditions should be corrected prior to prescribing losartan or treatment should be initiated with a lower dose of losartan.
Electrolyte disturbances are common in patients with impaired renal function with or without diabetes mellitus, so close monitoring of these patients is necessary. In clinical trials involving patients with type 2 diabetes mellitus with proteinuria, the incidence of hyperkalemia was greater in the group taking losartan than in the group taking placebo. Several patients discontinued therapy due to the occurrence of hyperkalemia.
Potassium-saving diuretics, potassium preparations, or potassium-containing salt substitutes are not recommended during treatment with losartan.
Aortic or mitral stenosis, hypertrophic obstructive cardiomyopathy
As with all drugs with vasodilatory effects, APA II should be prescribed with caution in patients with aortic or mitral stenosis or hypertrophic obstructive cardiomyopathy.
Ischemic Heart Disease and Cerebrovascular Disease
As with all drugs with a vasodilator effect, APA II should be prescribed with caution in patients with ischemic heart disease or cerebrovascular disease because excessive BP reduction in this group of patients may lead to myocardial infarction or stroke.
Chronic Heart Failure
As with other drugs acting on the RAAS, patients with CHF and with or without impaired renal function are at risk of developing severe arterial hypotension or acute renal impairment.
As there is insufficient experience with the use of losartan in patients with heart failure and concomitant severe renal impairment, in patients with severe heart failure (NYHA functional class IV), and in patients with heart failure and symptomatic life-threatening arrhythmias, losartan should be prescribed with caution.
Primary Hyperaldosteronism
Because patients with primary hyperaldosteronism generally do not respond favorably to therapy with hypotensive agents that act by inhibiting RAS, the use of losartan is not recommended in this group of patients.
Hepatic impairment
The data from pharmacokinetic studies indicate that plasma concentrations of losartan are significantly increased in patients with cirrhosis, so a lower dose of losartan should be administered to patients with a history of hepatic impairment. There is no experience with losartan in patients with severe hepatic impairment, so the drug should not be used in this group of patients.
Renal dysfunction
In some predisposed patients, changes in renal function, including the development of renal failure, have been observed due to inhibition of the RAAS. These changes in renal function may return to normal after discontinuation of treatment.
Some drugs with an effect on the RAAS may increase blood urea and serum creatinine concentrations in patients with bilateral renal artery stenosis or arterial stenosis of the sole kidney. Similar effects have been reported with losartan. Such changes in renal function may be reversible after discontinuation of therapy.
Lozartan should be used with caution in patients with bilateral renal artery stenosis or renal artery stenosis of the single kidney.
Particular patient populations
Race
Children and Adolescents
The efficacy and safety of losartan in children and adolescents younger than 18 years have not been established.
If neonates whose mothers have taken losartan during pregnancy develop oliguria or arterial hypotension, symptomatic therapy to maintain BP and renal perfusion should be given. Blood transfusion or dialysis may be required to prevent the development of arterial hypotension and/or to maintain renal function.
Patients in the Elderly
Clinical studies have not demonstrated any specific safety and efficacy of losartan in elderly patients (over 65 years of age).
No studies have been performed to evaluate the effect on driving and mechanic ability, but caution should be exercised when using hypotensive therapy and driving or operating machinery as dizziness and somnolence may occur especially at the beginning of therapy or when increasing the dose.
Contraindications
Contraindications
– Hypersensitivity to losartan and other drug components;
– concomitant use with angiotensin-converting enzyme (ACE) inhibitors in patients with diabetic nephropathy;
– hereditary lactose intolerance, lactase deficiency, glucose-galactose malabsorption syndrome;
– severe hepatic impairment (no experience of use);
– pregnancy and breastfeeding;
– children under 18 years of age (efficacy and safety of use have not been established).
– Bilateral renal artery stenosis or artery stenosis of the sole kidney; hyperkalemia;
– Conditions after renal transplantation (no experience with use);
– Aortic or mitral stenosis;
– hypertrophic obstructive cardiomyopathy;
– heart failure with concomitant severe renal impairment;
– severe heart failure (NYHA functional class IV);
– heart failure with life-threatening arrhythmias;
– ischemic heart disease;
– cerebrovascular disease;
– primary hyperaldosteronism;
– history of angioedema;
– patients with decreased circulating blood volume (e.g., those treated with high doses of diuretics) – symptomatic arterial hypotension may occur.
Side effects
Side effects
Classification of the frequency of side effects according to World Health Organization (WHO) recommendations:
very often â¥1/10;
often from â¥1/100 to < 1/10;
infrequently from â¥1/1000 to < 1/100;
rarely from â¥1/10000 to < 1/1000;
very rarely < 1/10000, including individual reports;
frequency is unknown – it is not possible to determine the frequency of occurrence from the available data.
In general, losartan is well tolerated in patients with AH. Adverse events (AEs) are mild and transient and do not require withdrawal. The cumulative incidence of NIH when taking losartan is comparable to placebo. In controlled trials, the rate of therapy withdrawal due to clinically significant NSCs was 2.3% in losartan and 3.7% in placebo.
In controlled clinical trials of losartan in patients with AH, the following NIHs have been observed.
Nervous system disorders:
frequently, dizziness;
infrequently, drowsiness, headache, and sleep disturbances.
Hearing and labyrinth disorders:
often – systemic dizziness (vertigo).
Cardiac disorders:
infrequent – palpitations, angina pectoris.
Vascular disorders:
infrequent – (orthostatic) hypotension (including dose-mediated orthostatic effects) (especially in patients with decreased RBC, such as patients with severe heart failure or patients receiving high-dose diuretic treatment).
Gastrointestinal disorders:
Infrequent – abdominal pain, constipation.
Skin and subcutaneous tissue disorders:
Infrequent – skin rash.
General disorders and reactions at the site of administration:
infrequent – weakness, increased fatigue, edema.
Laboratory and instrumental data:
frequently – hyperkalemia;
rarely – increased alanine aminotransferase (ALT) activity (usually returned to normal after withdrawal of therapy).
Controlled clinical trials have shown that losartan is generally well tolerated in patients with AH and left ventricular hypertrophy. The following NNDs were observed in these studies:
Nervous system disorders:
often dizziness.
Hearing and labyrinth disorders:
often – systemic vertigo (vertigo).
General disorders and reactions at the site of administration:
infrequent – weakness, increased fatigue.
In the LIFE study, patients without a history of diabetes mellitus had a lower incidence of new diabetes mellitus with losartan compared with atenolol (p < 0.001). Because this study did not include a group of patients taking placebo, it is unknown whether this is a beneficial effect of losartan or an adverse event of atenolol. Controlled clinical trials have shown that losartan is generally well tolerated in patients with type 2 diabetes mellitus and proteinuria. The following NNDs were observed in these studies:
Nervous system disorders:
often dizziness.
Vascular disorders:
often – (orthostatic) hypotension (including dose-mediated orthostatic effects) (especially in patients with decreased RBC, such as patients with severe heart failure or patients treated with high-dose diuretics).
General disorders and reactions at the site of administration:
Infrequent – weakness, increased fatigue.
Laboratory and instrumental findings:
often – hyperkalemia (in a clinical trial involving patients with type 2 diabetes mellitus and nephropathy, hyperkalemia (greater than 5.5 mmol/L) was observed in 9.9% of patients taking losartan and 3.4% of patients taking placebo), hypoglycemia.
Overdose
Overdose
There is limited information on overdose.
The most likely manifestation of overdose
A pronounced decrease in BP and tachycardia; bradycardia may occur due to parasympathetic (vagus) stimulation. If symptomatic arterial hypotension develops, supportive therapy is indicated.
Treatment
Symptomatic therapy.
Lozartan and its active metabolite are not excreted by hemodialysis.
Similarities
Similarities
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | Store in the dark place at a temperature not exceeding 25 °С. Store out of the reach of children. |
| Manufacturer | Vertex, Russia |
| Medication form | pills |
| Brand | Vertex |
Other forms…
Related products
Buy Lozartan 100 mg, 90 pcs. with delivery to USA, UK, Europe and over 120 other countries.