No products in the cart.
Lorista, 50 mg 60 pcs.
€1.00
Out of stock
(E-mail when Stock is available)
Description
Heart failure, Hypertension (high blood pressure), Prevention of heart attacks and strokes, Diabetic nephropathy
- Arterial hypertension.
- Risk reduction in associated cardiovascular morbidity and mortality in patients with arterial hypertension and left ventricular hypertrophy, manifested by a combined reduction in cardiovascular mortality, stroke and myocardial infarction.
- Kidney protection in patients with type 2 diabetes mellitus with proteinuria – slowing the progression of renal failure, manifested by decreased incidence of hypercreatininemia, incidence of terminal chronic renal failure requiring hemodialysis or renal transplantation, mortality rates, and decreased proteinuria.
- Cronic heart failure with ineffective treatment with ACE inhibitors or intolerance to ACE inhibitors. It is not recommended to transfer patients with heart failure and stable hemodynamic parameters while taking ACE inhibitors to therapy with losartan.
.
Active ingredient
Active ingredient
Composition
Composition
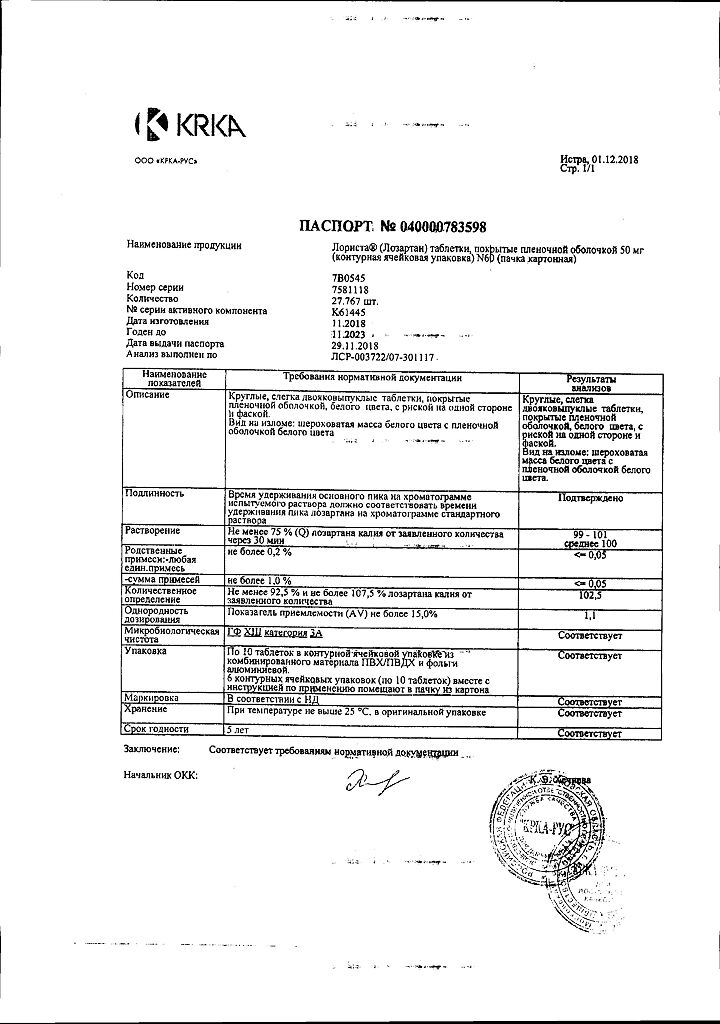
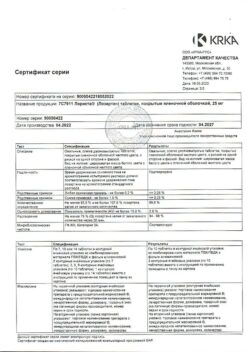
for 1 tablet 12.5 mg/25 mg/50 mg/100 mg
Core:
Active substance:
Potassium losartan 12.50 mg/25.00 mg/50.00 mg/100.00 mg
Supplementary substances:
Cellactose 801, pregelatinized starch, corn starch, microcrystalline cellulose, colloidal silicon dioxide, magnesium stearate
Film shell:
Hypromellose, talc, propylene glycol, quinoline yellow dye (E104) (for 12.5 mg and 25 mg tablets), titanium dioxide (E171)
1Cellactose 80: lactose monohydrate, cellulose.
How to take, the dosage
How to take, the dosage
The drug Lorista® is taken orally regardless of the time of meals. Lorista® can be taken in combination with other hypotensive agents.
Arterial hypertension
The standard starting and maintenance dose for most patients is 50 mg of Lorista® once daily. The maximum antihypertensive effect is achieved after 3-6 weeks from the beginning of therapy. In some patients the dose may be increased up to maximal dose of 100 mg of Lorista® once daily for more effect.
In patients with decreased blood circulation (e.g., when taking high doses of diuretics), the starting dose of Lorista® should be reduced to 25 mg once daily (see section “Special Precautions”).
There is no need to adjust the starting dose of Lorista® for elderly patients and patients with impaired renal function, including dialysis patients.
Patients with a history of liver disease are recommended to use lower doses of Lorista® (see section “Special Precautions”).
Risk reduction for associated cardiovascular morbidity and mortality in patients with AH and left ventricular hypertrophy
The standard initial dose of Lorista® is 50 mg once daily. Later on, it is recommended to add hydrochlorothiazide at low doses to therapy or to increase Lorista® up to maximum dose 100 mg once daily with regard to the lowering of BP.
Kidney protection in patients with type 2 diabetes mellitus and proteinuria
The standard starting dose of Lorista® is 50 mg once daily. Later the dose of the preparation Lorista® may be increased up to maximum dose of 100 mg once a day with regard to the degree of blood pressure decrease. The drug Lorista® may be used in combination with other hypotensive agents (e.g., diuretics, slow calcium channel blockers (SCBs), alpha- and beta-adrenoblockers, centrally acting hypotensive agents), insulin and other hypoglycemic agents (e.g., sulfonylurea derivatives, glitazones and glucosidase inhibitors).
chronic heart failure
The starting dose of Lorista® for patients with CHF is 12.5 mg once daily. Typically, the dose is adjusted at weekly intervals (i.e., 12.5 mg/day, 25 mg/day, 50 mg/day, 100 mg/day to a maximum dose [for this indication only] of 150 mg once daily), depending on individual tolerability.
Interaction
Interaction
Other hypotensive drugs may increase the antihypertensive effect of losartan. Concomitant use with other drugs that may cause arterial hypotension (such as tricyclic antidepressants, neuroleptics, baclofen and amifostine) may increase the risk of arterial hypotension.
No clinically significant interactions of losartan with hydrochlorothiazide, digoxin, warfarin, cimetidine and phenobarbital were found in clinical studies of pharmacokinetic drug interactions. Rifampicin, as an inducer of drug metabolism, reduces the plasma concentration of the active metabolite losartan. Two CYP3A4 isoenzyme inhibitors, ketoconazole and erythromycin, have been studied in clinical trials. Ketoconazole had no effect on the metabolism of losartan to the active metabolite after intravenous administration of losartan. Erythromycin had no clinically significant effect with oral administration of losartan. Fluconazole, a CYP2C9 isoenzyme inhibitor, reduces plasma concentrations of the active metabolite of losartan, but the pharmacodynamic significance of concomitant use of losartan and CYP2C9 isoenzyme inhibitors has not been studied. Patients who do not metabolize losartan to an active metabolite have been shown to have a very rare and specific defect in the CYP2C9 isoenzyme. These data suggest that the metabolism of losartan to the active metabolite is performed by the CYP2C9 isoenzyme rather than the CYP3A4 isoenzyme.
Simultaneous use of losartan, as well as other drugs that block angiotensin II or its effects, with potassium-saving diuretics (e.g., spironolactone, eplerenone, triamterene, amiloride), potassium-containing supplements or potassium salts may result in increased serum potassium levels.
As with other drugs that affect sodium ion excretion, losartan may decrease lithium excretion, so serum lithium levels should be carefully monitored when concomitant use of lithium and ARA II drugs.
Nonsteroidal anti-inflammatory drugs (NSAIDs), including selective cyclooxygenase-2 (COX-2) inhibitors, may decrease the effect of diuretics and other hypotensive agents. Due to this, the antihypertensive effect of ARA II or ACE inhibitors may be weakened when concomitantly used with NSAIDs, including selective COX-2 inhibitors.
In some patients with impaired renal function (e.g., elderly patients or patients with dehydration, including those taking diuretics) receiving NSAID therapy, including selective COX-2 inhibitors, concurrent use of ARA II or ACE inhibitors may cause further impairment of renal function, including development of acute renal failure. These effects are usually reversible. Simultaneous use of these drugs should be conducted with caution in patients with impaired renal function.
Dual RAAS blockade with ARA II, ACE inhibitors or aliskiren (renin inhibitor) is associated with an increased risk of arterial hypotension, syncope, hyperkalemia and renal function impairment (including acute renal failure) compared to monotherapy. Regular monitoring of BP, renal function and plasma electrolyte levels is necessary in patients taking concomitantly Lorist® and other drugs that affect the RAAS. Concomitant administration of ARA II with drugs containing aliskiren is contraindicated in patients with diabetes mellitus and/or moderate to severe renal insufficiency (FFR less than 60 ml/min/1.73 m2 of body surface area) and is not recommended in other patients. Concomitant use of ARA II with ACE inhibitors is contraindicated in patients with diabetic nephropathy and is not recommended in other patients.
Special Instructions
Special Instructions
Bilateral renal artery stenosis or stenosis of the artery of a single kidney, hyperkalemia, post kidney transplantation (no experience), aortic or mitral stenosis, hypertrophic obstructive cardiomyopathy (HOCMP), heart failure with concomitant severe renal impairment, severe heart failure (NYHA functional class IV), heart failure with life-threatening arrhythmias, coronary heart disease (CHD), cerebrovascular disease, primary hyperaldosteronism, history of angioedema.
In patients with decreased circulating blood volume (CBC) (e.g., patients treated with high doses of diuretics), symptomatic arterial hypotension may develop.
Persons under 18 years of age are contraindicated (efficacy and safety of use have not been established).
There is no need to select the initial dose of Lorista® for elderly patients and patients with impaired renal function, including dialysis patients.
Contraindicated in patients with severe liver dysfunction (no experience of use).
Patients with a history of liver disease are recommended to use lower doses of Lorista® (see section “Special Precautions”).
Hypersensitivity reactions
. Patients with a history of angioedema (swelling of the face, lips, pharynx/larynx and/or tongue) must be under close medical supervision when using Lorist® . see section “Side effects”).
Embryotoxicity
The use of drugs acting on the RAAS in the second and third trimesters of pregnancy reduces renal function in the fetus and increases fetal and neonatal morbidity and mortality. Oligohydramnios can be associated with fetal lung hypoplasia and skeletal deformities. Possible NS in newborns include skull bone hypoplasia, anuria, arterial hypotension, renal failure, and mortality. If pregnancy is diagnosed, Lorista® should be withdrawn immediately (see section “Use in pregnancy and during breastfeeding”).
Arterial hypotension and impaired water-electrolyte balance or decreased CIC
. Symptomatic arterial hypotension may develop in patients with decreased blood pressure (e.g., those treated with high doses of diuretics). Correction of these conditions should be performed prior to the use of Lorista® or treatment should be started with a lower dose of Lorista® (see section “Dosage and administration”).
Disruption of the water-electrolyte balance is characteristic of patients with impaired renal function with or without diabetes mellitus; therefore, close monitoring of these patients is necessary. In clinical trials involving patients with type 2 diabetes mellitus with proteinuria, the incidence of hyperkalemia was greater in the group taking losartan than in the group taking placebo. Several patients discontinued therapy due to the occurrence of hyperkalemia (see section “Side effects”, subsection “Laboratory and instrumental data”).
When treated with Lorist®, it is not recommended to take potassium-saving diuretics, potassium preparations or potassium-containing table salt substitutes.
Aortic or mitral stenosis, GOCMP
. As with all drugs with vasodilatory effects, ARA II should be used with caution in patients with aortic or mitral stenosis or GOCMP.
IBS and cerebrovascular disease
. As with all drugs with a vasodilator effect, APA II should be used with caution in patients with CHD or cerebrovascular disease, as a pronounced decrease in BP in this group of patients may lead to myocardial infarction or stroke.
CHF
. As with other drugs acting on the RAAS, patients with CHF and with or without impaired renal function are at risk of developing severe arterial hypotension or acute renal dysfunction.
Because there is insufficient experience with the use of Lorista® in patients with heart failure and concomitant severe renal impairment, in patients with severe heart failure (NYHA functional class IV) and in patients with heart failure and symptomatic life-threatening arrhythmias, Lorista® should be used with caution in these groups.
Primary Hyperaldosteronism
. Because patients with primary hyperaldosteronism generally do not have a positive response to therapy with hypotensive agents that act by inhibiting the RAAS, the use of Lorista® is not recommended in this patient group.
Hepatic dysfunction
. Data from pharmacokinetic studies indicate that plasma concentrations of losartan are significantly increased in patients with cirrhosis, so patients with a history of hepatic impairment should use Lorista® at a lower dose. There is no experience with losartan in patients with severe hepatic impairment; therefore, Lorista® should not be used in this group of patients (see sections “Pharmacological Properties [subsection “Pharmacokinetics”], “Contraindications”, “Dosage and administration”).
Kidney function impairment
Kidney function changes, including the development of renal failure, have been observed in some predisposed patients due to RAAS inhibition. These changes in renal function may return to normal after discontinuation of treatment.
Some drugs that affect the RAAS may increase serum concentrations of urea and creatinine in patients with bilateral renal artery stenosis or renal artery stenosis of the single kidney. Similar effects have been reported with losartan. Such renal dysfunction may be reversible after discontinuation of therapy. Losartan should be used with caution in patients with bilateral renal artery stenosis or renal artery stenosis of the solitary kidney.
Special patient groups
Ethnic characteristics
Analysis of data from the entire patient population enrolled in a clinical trial examining the effect of losartan on reducing the incidence of the main composite criterion of the study evaluation in patients with AH and left ventricular hypertrophy showed that the ability of losartan compared with atenolol to reduce the risk of stroke and myocardial infarction and to reduce cardiovascular mortality in patients with AH and left ventricular hypertrophy (by 13.0%) did not extend to non-HG patients, although both modes of therapy were effective In this study, losartan compared with atenolol reduced cardiovascular morbidity and mortality in patients with AH and left ventricular hypertrophy of all races except the non-Hispanic race. However, in this study, patients of the non-Hispanic race who received atenolol had a lower risk of developing the main composite criterion of the study evaluation (that is, a lower combined incidence of cardiovascular mortality, stroke, and myocardial infarction) compared with patients of the same race who took losartan.
Children and adolescents
The efficacy and safety of losartan in children and adolescents younger than 18 years have not been established.
If neonates whose mothers have taken losartan during pregnancy develop oliguria or arterial hypotension, symptomatic therapy to maintain BP and renal perfusion is necessary. Blood transfusion or dialysis may be required to prevent the development of arterial hypotension and/or to maintain renal function.
Elderly patients
Clinical studies have not demonstrated any specific safety and efficacy of losartan in elderly patients (>65 years).
There have been no studies to evaluate the effect of losartan on driving and operating machinery, but caution should be exercised when using hypotensive therapy and driving or operating machinery as dizziness and somnolence may occur, especially at the start of therapy or when increasing the dose of Lorist®.
Synopsis
Synopsis
Tablets 12.5 mg: Oval, slightly biconvex, film-coated tablets from light yellow to yellow, with bevel.
Break appearance: a rough white mass with light yellow to yellow film coating.
Tablets 25 mg: Oval, slightly biconvex, film-coated tablets, yellow, with a rib on one side and a bevel.
Breakage appearance: a rough mass of white color with yellow film coating.
Tablets 50 mg: Circular, slightly biconvex, film-coated white tablets, with a ridge on one side and a bevel.
Breakage appearance: rough white mass with white film coating.
Tablets 100 mg: Oval, slightly biconvex, white film-coated tablets.
Breakage appearance: a rough mass of white color with white film coating.
Contraindications
Contraindications
Overdose
Overdose
The information on overdose is limited.
Symptoms:The most likely manifestation of overdose is a marked decrease in BP and tachycardia, bradycardia may occur due to parasympathetic (vagus) stimulation. If symptomatic arterial hypotension develops, supportive therapy is indicated.
Treatment:symptomatic therapy. Losartan and its active metabolite are not excreted by hemodialysis.
Pregnancy use
Pregnancy use
Drugs acting directly on the RAAS may cause serious damage and death to the developing fetus, therefore, when diagnosed with pregnancy, Lorista® should be immediately withdrawn and, if necessary, an alternative hypotensive therapy should be prescribed.
The therapy with Lorista® should not be started during pregnancy. If continuation of hypotensive therapy with losartan is deemed necessary in patients planning pregnancy, losartan should be replaced with alternative hypotensive agents that have an established safety profile for use in pregnancy.
While there is no experience with the use of losartan in pregnant women, preclinical animal studies have shown that administration of losartan causes serious fetal and neonatal damage and death to the fetus or offspring. The mechanism of these events is thought to be due to effects on the RAAS.
Fetal renal perfusion dependent on the development of RAAS appears in the second trimester, so the risk to the fetus is increased if Lorista® is used in the second or third trimester of pregnancy.
The use of drugs affecting the RAAS in the second and third trimesters of pregnancy reduces fetal renal function and increases fetal and neonatal morbidity and mortality. The development of oligohydramnios may be associated with fetal lung hypoplasia and skeletal deformities. Possible adverse events (AEs) in neonates include skull bone hypoplasia, anuria, arterial hypotension, renal failure, and death.
The above adverse outcomes are usually due to the use of drugs affecting the RAAS in the second and third trimesters of pregnancy. Most epidemiological studies of fetal abnormalities after the use of hypotensive drugs in the first trimester of pregnancy have found no difference between the drugs acting on the RAAS and other hypotensive agents. When using hypotensive therapy in pregnant women, it is important to optimize possible outcomes for the mother and fetus.
If no alternative therapy can be selected to replace therapy with drugs acting on the RAAS, the patient should be informed about the possible risks of therapy for the fetus. Periodic ultrasound examinations should be performed to assess the intra-amniotic space. If oligohydramnion is detected, Lorist® should be discontinued unless it is vital for the mother. Depending on the gestational age, appropriate tests should be performed on the fetus. Patients and physicians should be aware that oligohydramnios may not be detected until irreversible fetal damage has occurred. Careful monitoring of newborns whose mothers have taken Lorista® during pregnancy should be done to control arterial hypotension, oliguria, and hyperkalemia.
It is not known whether losartan is excreted with breast milk. Because many medications are excreted with breast milk and there is a risk of possible adverse effects in a breastfed infant, a decision should be made to discontinue breastfeeding or to discontinue the drug in light of the mother’s need for it.
Similarities
Similarities
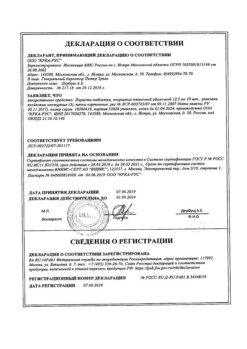
Additional information
| Shelf life | 5 years. Do not use the product after the expiration date. |
|---|---|
| Conditions of storage | At temperature no higher than 25ºC, in original packaging. Store out of reach of children. |
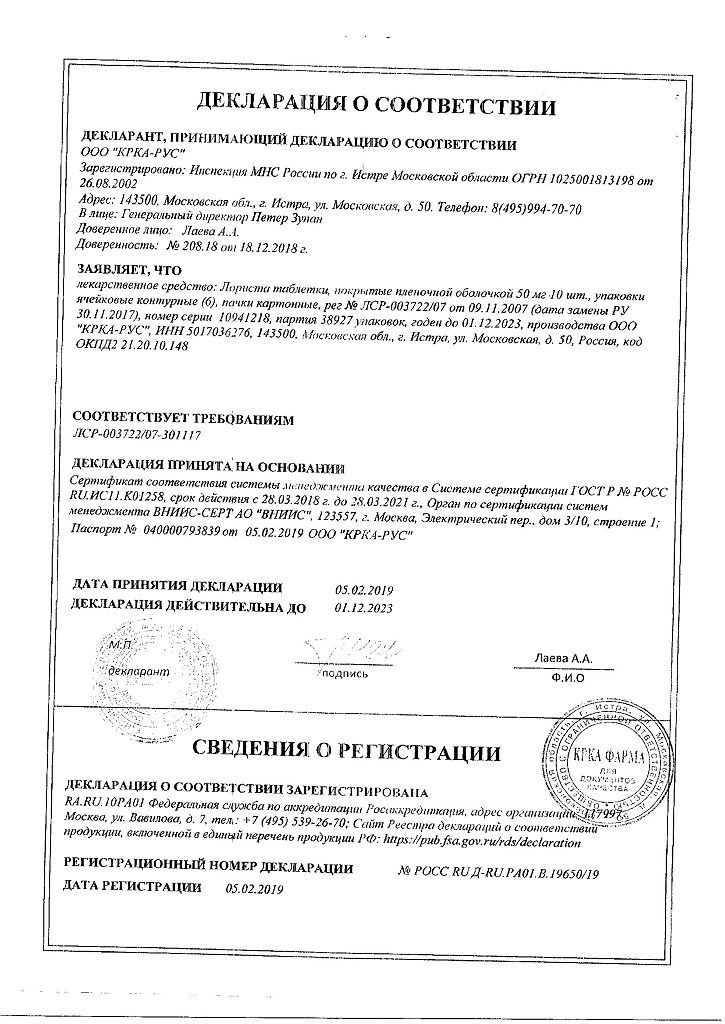
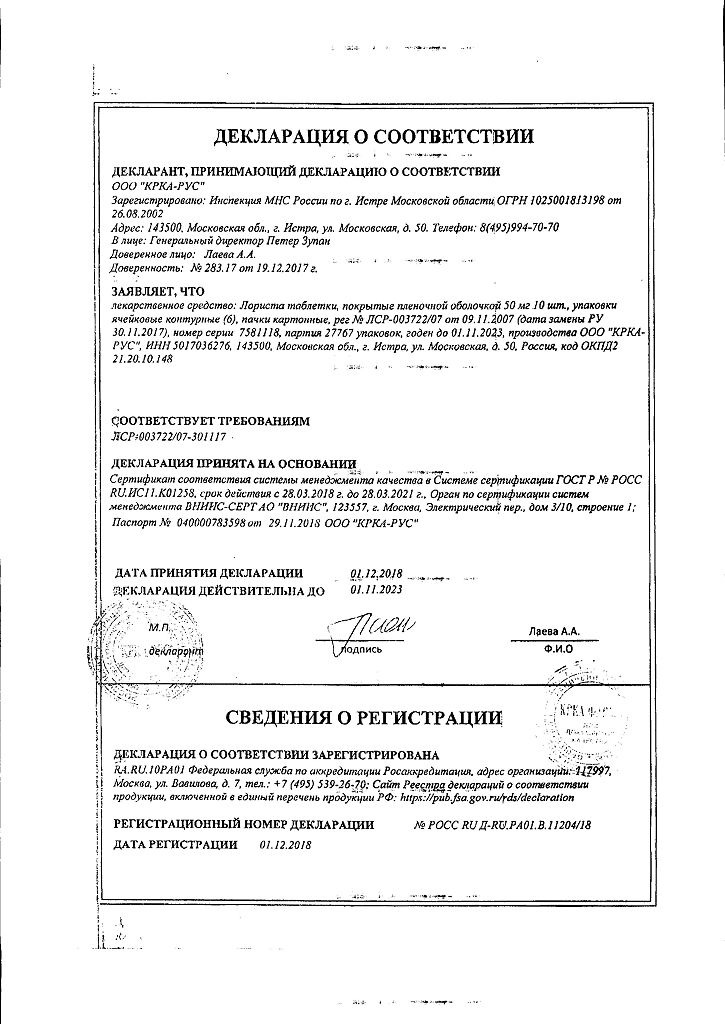
| Manufacturer | KRKA-RUS, Russia |
| Medication form | pills |
| Brand | KRKA-RUS |
Other forms…
Related products
Buy Lorista, 50 mg 60 pcs. with delivery to USA, UK, Europe and over 120 other countries.