No products in the cart.
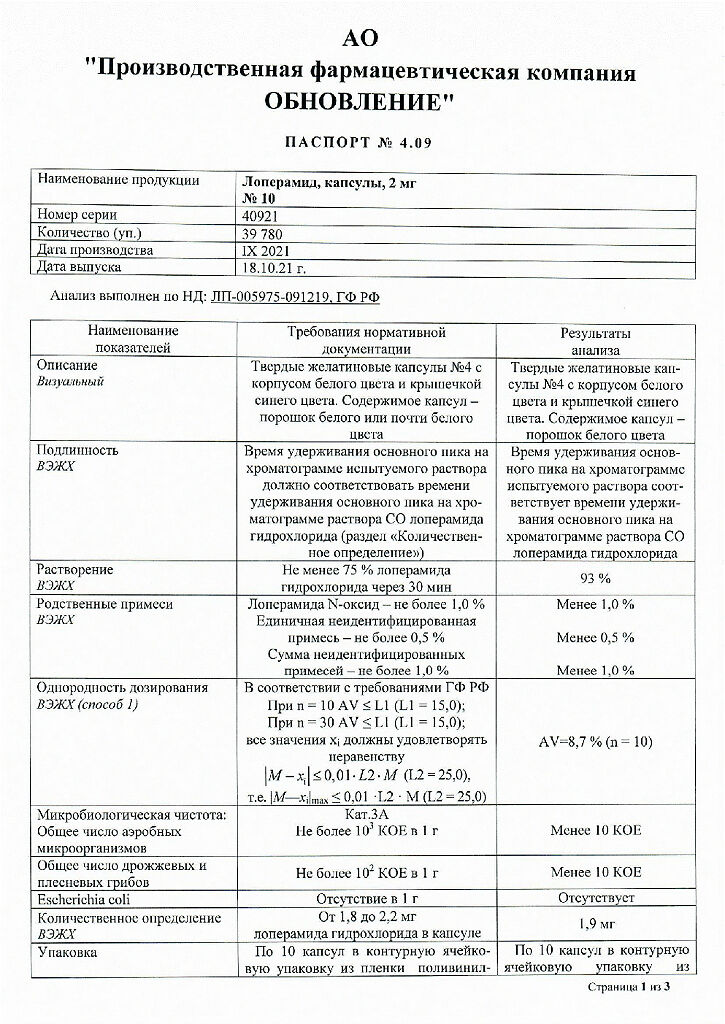
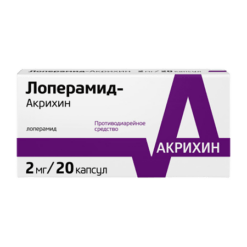
Loperamide, 2 mg capsules 10 pcs
€1.64 €1.49
Description
Pharmacotherapeutic group: Antidiarrheal.
TAC code: A07DA03.
Pharmacological properties.
Binding to opioid receptors of the intestinal wall (stimulation of cholinergic and adrenergic neurons through guanine nucleotides), reduces tone and motility of intestinal smooth muscle, slows the passage of intestinal contents, reduces excretion of fluid and electrolytes with feces. Increases the tone of the anal sphincter, helps to retain feces and reduce urges to defecation. The action comes on quickly and lasts 4-6 hours.
.
Indications
Indications
symptomatic treatment of acute and chronic diarrhea of various origins (including allergic, emotional, medicinal, radiation; with changes in diet and quality food composition, with metabolic and absorption disorders);
as an auxiliary drug for diarrhea of infectious origin;
regulation of stool in patients with ileostomy.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: Antidiarrheal agent.
ATX code: A07DA03.
Pharmacological properties.
By binding to opioid receptors of the intestinal wall (stimulation of cholinergic and adrenergic neurons through guanine nucleotides), it reduces the tone and motility of intestinal smooth muscles, slows down the passage of intestinal contents, and reduces the excretion of fluid and electrolytes in feces. Increases the tone of the anal sphincter, promotes fecal retention and reduces the urge to defecate. The action occurs quickly and lasts 4-6 hours.
Special instructions
Special instructions
If there is no effect after 2 days of using loperamide, you should consult a doctor. If constipation or bloating develops during treatment, loperamide should be discontinued.
In patients with impaired liver function, careful monitoring for signs of toxic damage to the central nervous system (stupor, incoordination, drowsiness, miosis, muscle hypertonicity, respiratory depression, increased fatigue, drowsiness, dizziness) is necessary.
Treatment with loperamide does not replace the correction of water and electrolyte balance that develops with diarrhea. During the treatment of diarrhea (especially in children), it is necessary to replace the loss of fluid and electrolytes. Dehydration may contribute to altered response to loperamide.
In some cases, in AIDS patients with infectious colitis of both a viral and bacterial nature, toxic dilatation of the colon may develop when treated with loperamide.
Impact on the ability to drive vehicles and operate machinery
During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Loperamide
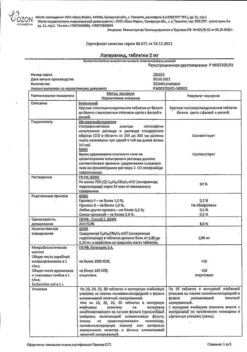
Composition
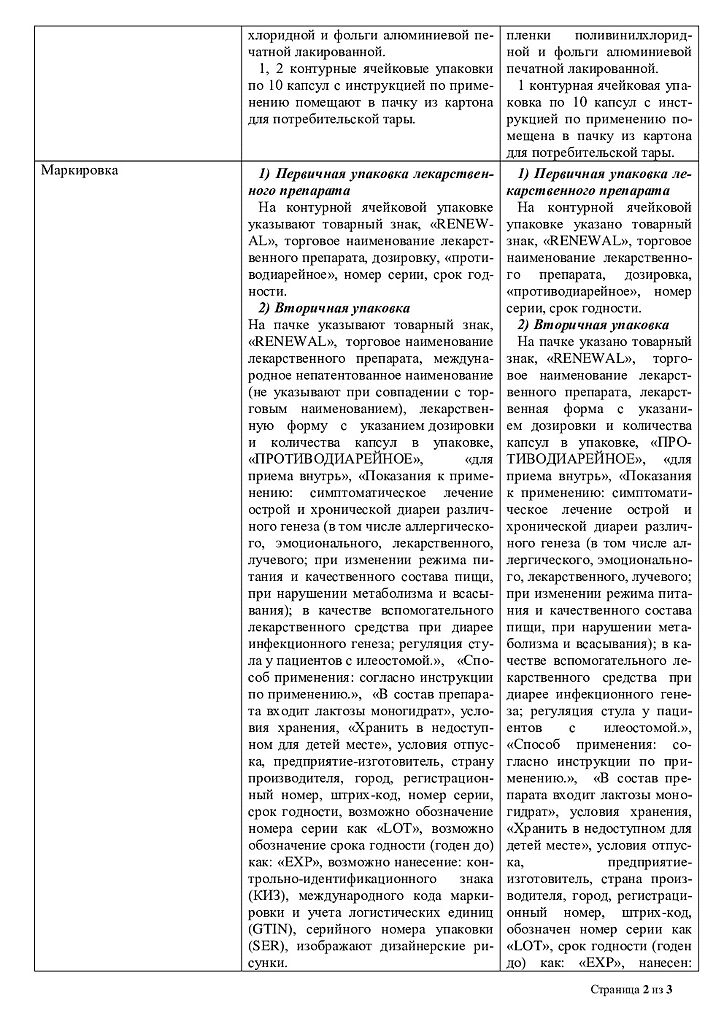
Composition
1 capsule contains:
active substance: loperamide hydrochloride – 2 mg;
excipients:
lactose monohydrate – 104.5 mg,
corn starch – 30.0 mg,
talc – 1.4 mg,
magnesium stearate – 1.4 mg,
colloidal silicon dioxide (Aerosil) – 0.7 mg;
hard gelatin capsules
(capsule body composition): titanium dioxide – 2.0000%, gelatin – up to 100%,
composition of the capsule cap: patented blue dye
Pregnancy
Pregnancy
Early embryonic lethality and teratogenicity were observed in preclinical studies of favipiravir at doses similar to or lower than clinical doses.
AREPLIVIR is contraindicated in pregnant women, as well as in men and women planning pregnancy. When prescribing AREPLIVIR to women capable of childbearing (including those less than 2 years postmenopausal), it is necessary to confirm a negative pregnancy test result before starting treatment. A repeat pregnancy test must be performed after stopping the drug.
It is necessary to use effective methods of contraception (condom with spermicide) while taking the drug and after its completion: for 1 month for women and for 3 months for men.
When prescribing AREPLIVIR, lactating women must stop breastfeeding while taking the drug and for 7 days after finishing it, since the main metabolite of favipiravir passes into breast milk.
Contraindications
Contraindications
hypersensitivity to loperamide and/or any of the components of the drug;
lactase deficiency, lactose intolerance, glucose-galactose malabsorption;
pregnancy (first trimester);
breastfeeding period;
children under 6 years of age;
acute dysentery, characterized by bloody stool and high fever;
ulcerative colitis in the acute stage;
bacterial enterocolitis caused by pathogenic microorganisms, including Salmonella, Shigella and Campylobacter;
pseudomembranous colitis associated with broad-spectrum antibiotic therapy;
intestinal obstruction (including in cases where suppression of intestinal motility should be avoided due to the risk of severe consequences, such as megacolon or toxic megacolon). Loperamide should be discontinued immediately if constipation, bloating or intestinal obstruction occurs.
Side Effects
Side Effects
Allergic reactions: skin rash, itching, angioedema, in some cases – erythema multiforme, Stevens-Johnson syndrome and toxic epidermal necrolysis.
From the digestive system: dryness of the oral mucosa, pain or discomfort in the abdomen, nausea, vomiting, constipation, bloating, intestinal colic, and in some cases, intestinal obstruction.
From the central nervous system and peripheral nervous system: fatigue, drowsiness, dizziness.
Other: urinary retention.
Interaction
Interaction
According to preclinical studies, loperamide is a substrate of P-glycoprotein. With the simultaneous use of loperamide (single dose of 16 mg) and quinidine or ritonavir, which are P-glycoprotein inhibitors, the concentration of loperamide in the blood plasma increased 2-3 times. The clinical significance of the described pharmacokinetic interaction with P-glycoprotein inhibitors when loperamide is used at recommended doses is unknown.
The simultaneous use of loperamide (single dose of 4 mg) and itraconazole, an inhibitor of the CYP3A4 isoenzyme and P-glycoprotein, led to an increase in the concentration of loperamide in the blood plasma by 3-4 times. In the same study, the use of the CYP2C8 isoenzyme inhibitor, gemfibrozil, led to an approximately 2-fold increase in plasma concentrations of loperamide. When using a combination of itraconazole and gemfibrozil, the peak plasma concentration of loperamide increased by 4 times and the total concentration by 13 times. This increase was not associated with CNS effects as assessed by psychomotor tests (i.e., subjective sleepiness rating and digit substitution test). The simultaneous use of loperamide (single dose of 16 mg) and ketoconazole, an inhibitor of the CYP3A4 isoenzyme and P-glycoprotein, led to a fivefold increase in the concentration of loperamide in the blood plasma. This increase was not associated with an increase in pharmacodynamic effect assessed by pupil size.
With simultaneous oral administration of desmopressin, the concentration of desmopressin in the blood plasma increased 3-fold, probably due to a slowdown in gastrointestinal motility.
It is expected that drugs with similar pharmacological properties may increase the effect of loperamide, and drugs that increase the rate of passage through the gastrointestinal tract may decrease the effect of loperamide.
Overdose
Overdose
Symptoms: depression of the central nervous system (stupor, loss of coordination, drowsiness, miosis, muscle hypertonicity, respiratory depression), urinary retention, intestinal obstruction. Children may be more sensitive to the CNS effects of loperamide than adults.
Cardiac complications such as QT prolongation, torsade de pointes (TdP), other serious ventricular arrhythmias, cardiac arrest, and syncope have been reported in patients with loperamide hydrochloride overdose. Deaths have also been reported.
Treatment: antidote – naloxone; Given that the duration of action of loperamide is longer than that of naloxone, repeated administration of naloxone is possible. Medical supervision is required for at least 48 hours.
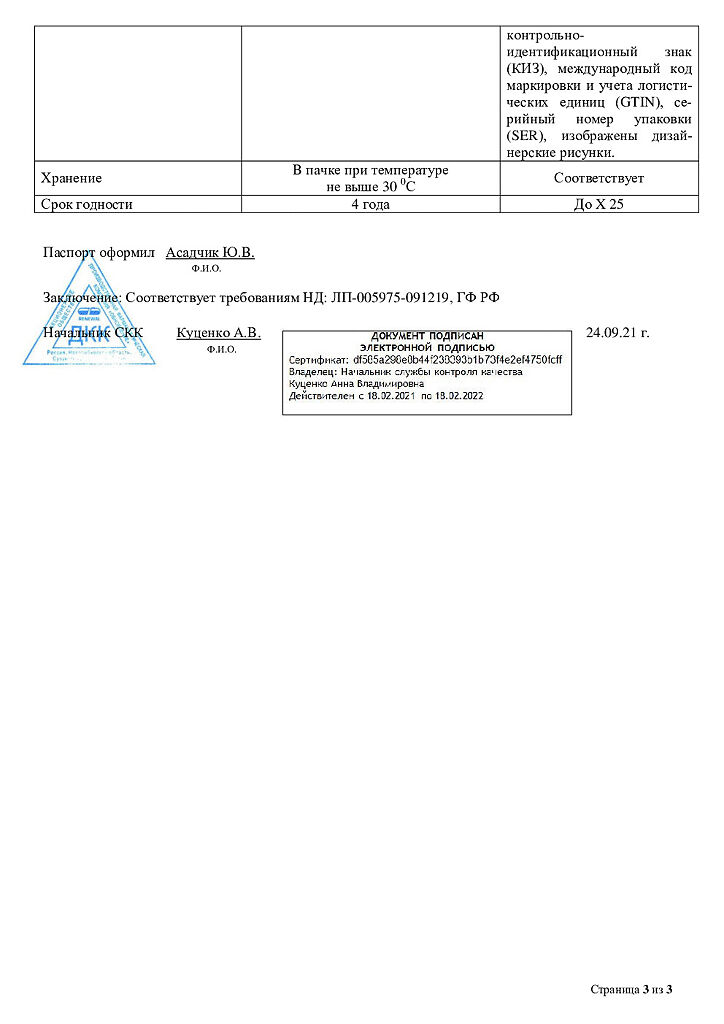
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C in consumer packaging (cardboard pack).
Keep out of the reach of children.
Shelf life
Shelf life
3 years.
Do not use after the expiration date stated on the package.
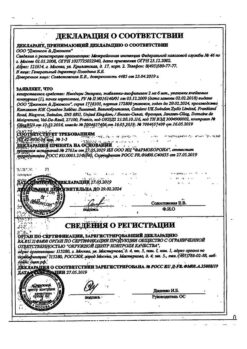
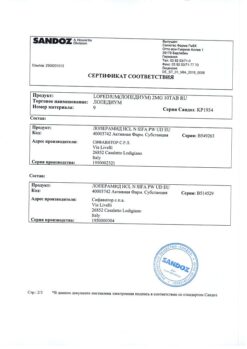
Manufacturer
Manufacturer
Update of PFC JSC, Russia
Additional information
| Shelf life | 3 years. Do not use after the expiration date printed on the package. |
|---|---|
| Conditions of storage | At the temperature not more than 25 ° C in the consumer package (carton pack). Store out of reach of children. |
| Manufacturer | Update PFC AO, Russia |
| Medication form | capsules |
| Brand | Update PFC AO |
Other forms…
Related products
Buy Loperamide, 2 mg capsules 10 pcs with delivery to USA, UK, Europe and over 120 other countries.