No products in the cart.
Lokren, 20 mg 28 pcs.
€26.69 €22.24
Description
Locren is a selective beta 1 -adrenoblocker without intrinsic sympathomimetic activity.
In high doses (at concentrations higher than therapeutic) it has a weak membrane stabilizing effect.
Indications
Indications
– Arterial hypertension.
– Prevention of angina attacks.
Pharmacological effect
Pharmacological effect
Lokren is a selective beta 1-blocker without internal sympathomimetic activity.
In high doses (at concentrations exceeding therapeutic levels) it has a weak membrane-stabilizing effect.
Special instructions
Special instructions
Use with caution in case of liver failure.
Use with caution in chronic renal failure and during hemodialysis. In patients with renal failure, the dose must be adjusted depending on the concentration of creatinine in the blood or creatinine clearance (CC).
Treatment of patients with angina should never be interrupted abruptly; sudden discontinuation can lead to severe cardiac arrhythmias, myocardial infarction or sudden death.
Patients taking Lokren require monitoring, which should include monitoring heart rate and blood pressure (daily at the beginning of treatment, then once every 3-4 months), glucose levels in patients with diabetes mellitus (once every 4-5 months), and monitoring of kidney function in elderly patients (once every 4-5 months). The patient should be taught how to calculate heart rate and instructed about the need for medical consultation if the heart rate is less than 50 beats/min.
In patients with coronary artery disease, the dose should be reduced gradually (over 1-2 weeks) and, if necessary, replacement therapy should be started simultaneously to avoid progression of angina pectoris. In approximately 20% of patients with angina pectoris, beta-blockers are ineffective (the main reasons are severe coronary atherosclerosis with a low ischemic threshold and heart rate at the time of an anginal attack less than 100 beats/min and increased end-diastolic pressure of the left ventricle, disrupting subendocardial blood flow).
With simultaneous therapy with clonidine, its use can be stopped only a few days after stopping Lokren.
Lokren should be discontinued before testing the content of catecholamines in the blood and urine (catecholamines in the blood, catecholamines in the urine), normetanephrine (free normetanephrine in the urine) and vanillinmandelic acid; antinuclear antibody titers.
In bronchial asthma and chronic obstructive pulmonary disease, beta-blockers can be prescribed only for moderate disease, with the choice of a selective beta-blocker in a low initial dose. Before starting treatment, it is recommended to assess respiratory function. If attacks develop during treatment, bronchodilators (β2-adrenergic agonists) can be used.
In patients with heart failure controlled therapeutically, if necessary, betaxolol can be used in very low, gradually increasing doses under strict medical supervision.
The dose of the drug must be reduced if the heart rate at rest is below 50-55 beats/min and the patient has clinical manifestations of bradycardia.
Given the negative dromotropic effect of beta-blockers, the drug should be used with caution in case of first-degree AV blockade.
Beta blockers may increase the number and duration of attacks in Prinzmetal’s angina. Use of cardioselective ? 1-blockers are possible for less severe and mixed forms, provided that treatment is carried out in combination with vasodilators.
Beta-blockers can lead to a deterioration in the condition of patients with peripheral circulatory disorders (Raynaud’s disease or syndrome, arteritis or chronic occlusive diseases of the arteries of the lower extremities).
When beta-blockers are used to treat hypertension caused by pheochromocytoma, careful monitoring of blood pressure is required.
Patients with diabetes mellitus should be warned about the need to strengthen self-monitoring of blood glucose levels at the beginning of treatment. Initial symptoms of hypoglycemia may be masked, especially tachycardia, palpitations, and sweating.
For psoriasis, a careful assessment of the need to prescribe the drug is required, because There are reports of worsening of the disease during treatment with beta-blockers.
In patients with a tendency to severe anaphylactic reactions (especially associated with the use of floctafenine or during desensitization), therapy with beta-blockers may lead to a further increase in reactions and a decrease in the effectiveness of treatment. When using the drug, the risk of developing anaphylactic reactions should be taken into account.
When performing general anesthesia, it should be taken into account that beta-blockers mask reflex tachycardia and increase the risk of developing arterial hypotension. Continuing therapy with beta-blockers reduces the risk of arrhythmia, myocardial ischemia and hypertensive crises. The anesthesiologist should be informed that the patient has been treated with beta-blockers.
In case of planned surgery and the need to discontinue drug therapy, it should be taken into account that discontinuation of the drug for 48 hours allows you to restore sensitivity to catecholamines. Therapy with beta-blockers should not be interrupted in patients with coronary insufficiency; it is recommended that treatment be continued until surgery, given the risk associated with sudden withdrawal of beta-blockers. In emergency operations or in cases where cessation of treatment is not possible, the patient should be protected from the effects of vagus nerve stimulation by appropriate premedication with atropine (repeated if necessary). For general anesthesia, it is necessary to use drugs with minimal negative inotropic effect.
Symptoms of thyrotoxicosis may be masked by therapy with beta-blockers.
Athletes should be aware that the drug may give a positive reaction during doping control tests.
When using the drug, you should avoid drinking alcohol.
Patients who use contact lenses should take into account that during treatment, tear fluid may decrease.
Beta blockers are less effective in smokers.
Treatment of elderly patients should begin with a low dose and under strict supervision.
The drug should not be used in children, because There are no clinical data on the effectiveness and safety of its use in this category of patients.
Active ingredient
Active ingredient
Betaxolol
Composition
Composition
1 film-coated tablet contains:
Betaxolol hydrochloride 20 mg,
Excipients:
lactose monohydrate,
sodium amylopectin glycolate,
microcrystalline cellulose,
anhydrous colloidal silicon dioxide,
magnesium stearate,
hypromellose,
macrogol 400,
titanium dioxide (E171).
Pregnancy
Pregnancy
Experimental studies on animals did not reveal the teratogenic effect of Lokren. To date, no teratogenic effects have been observed in humans, and no congenital malformations have been observed in controlled prospective studies.
The use of the drug during pregnancy is possible only if the expected benefit to the mother outweighs the potential risk to the fetus.
Betaxolol is excreted to a small extent in breast milk. The risk of hypoglycemia or bradycardia in a child has not been studied. If it is necessary to use Lokren during lactation, the issue of stopping breastfeeding should be decided.
It has been established that betaxolol has an effect on the fetus (intrauterine growth retardation, hypoglycemia, bradycardia). With the development of heart failure (decompensation) in newborns whose mothers took beta-blockers during pregnancy, they are hospitalized in the ICU; glucagon is prescribed at a rate of 0.3 mg/kg; isoprenaline and dobutamine are usually in fairly high doses and for a long time, which requires careful monitoring.
It should be borne in mind that in newborns whose mothers received beta-blockers, the effect of the latter persists for several days after birth. Although this residual effect may not have clinical consequences, it is nevertheless possible that a heart defect may develop, requiring intensive care in the newborn. In such a situation, you should avoid administering solutions that increase blood volume (risk of developing acute pulmonary edema). There have also been reports of bradycardia, respiratory distress syndrome and hypoglycemia. Therefore, careful monitoring of newborns in specialized conditions is recommended (monitoring heart rate and blood glucose levels during the first 3-5 days of life).
Contraindications
Contraindications
– Chronic heart failure stage II B–III.
– Cardiogenic shock.
– AV blockade II and III degrees (without connecting an artificial pacemaker).
– Prinzmetal’s angina.
– SSSU (including sinoatrial block).
– Severe bradycardia.
– Arterial hypotension.
– Cardiomegaly (without signs of heart failure).
– Simultaneous use with sultopride and floctafenine.
– Concomitant use of MAO inhibitors.
– Age up to 18 years (efficacy and safety have not been established).
– Hypersensitivity to betaxolol.
– The drug is contraindicated in cases of congenital galactosemia, impaired absorption of glucose/galactose, or lactase deficiency (since the composition contains lactose).
The drug should be used with caution in patients with a history of allergic reactions, with pheochromocytoma, metabolic acidosis, obliterating diseases of peripheral vessels (intermittent claudication, Raynaud’s syndrome), with liver failure, chronic renal failure, with hemodialysis, myasthenia gravis, depression (including a history), in the elderly, with AV blockade of the first degree, with chronic obstructive lung diseases (bronchial asthma, emphysema), in patients with psoriasis, chronic heart failure, thyrotoxicosis, diabetes mellitus.
Side Effects
Side Effects
From the central nervous system and peripheral nervous system: increased fatigue, weakness, dizziness, headache, drowsiness, insomnia, nightmares, depression, anxiety, confusion or short-term memory loss, hallucinations, asthenic syndrome, muscle weakness, paresthesia in the limbs (with intermittent claudication, Raynaud’s syndrome), tremor.
From the cardiovascular system: sinus bradycardia, palpitations, orthostatic hypotension, myocardial conduction disturbances, AV blockade (up to cardiac arrest), arrhythmias, weakening of myocardial contractility, development (or worsening) of symptoms of heart failure (swelling of the ankles, feet, legs), pronounced decrease in blood pressure, manifestation of vasospasm (decreased peripheral circulation, coldness of the lower extremities, Raynaud’s syndrome), chest pain.
From the digestive system: dryness of the mucous membranes of the oral cavity, nausea, vomiting, abdominal pain, constipation or diarrhea, liver dysfunction (dark urine, yellowness of the sclera or skin, cholestasis), changes in taste.
From the respiratory system: nasal congestion, difficulty breathing when prescribed in high doses (loss of selectivity); laryngo- and bronchospasm (in predisposed patients).
From the senses: visual disturbances, decreased secretion of the lacrimal gland, dry and sore eyes, conjunctivitis.
From the endocrine system: hyperglycemia in patients with non-insulin-dependent diabetes mellitus, hypoglycemia in patients receiving insulin, hypothyroid state.
Dermatological reactions: increased sweating, skin hyperemia, exanthema, psoriasis-like skin reactions, exacerbation of psoriasis.
Allergic reactions: skin rash, itching, urticaria.
Other: back pain, arthralgia, weakened libido, decreased potency, withdrawal syndrome (increased angina attacks, increased blood pressure); rarely – the appearance of antinuclear antibodies (only in exceptional cases is accompanied by clinical manifestations of the SLE type, which disappear when treatment is stopped).
Interaction
Interaction
Many drugs can cause bradycardia. This group includes beta-blockers, class IA antiarrhythmic drugs (quinidine, disopyramide), amiodarone and sotalol from class III antiarrhythmic drugs, diltiazem and verapamil from class IV, as well as digitalis glycosides, clonidine, guanfacine, mefloquine and cholinesterase inhibitors indicated for the treatment of Alzheimer’s disease.
Contraindicated combinations
When used simultaneously with floctafenine (in the event of shock or arterial hypotension caused by floctafenine), beta-blockers may lead to a decrease in compensatory reactions from the cardiovascular system. When used simultaneously with sultopride, severe bradycardia develops (additive effect).
Combinations that should be avoided When used simultaneously with calcium channel blockers (bepridil, diltiazem and verapamil), automaticity disorders occur (severe bradycardia, sinus node arrest), AV conduction disorders, heart failure (synergism). This combination can only be used under close clinical supervision and ECG monitoring (especially in the elderly or at the beginning of therapy). With simultaneous use with amiodarone, it is possible to develop disorders of contractility, automaticity and conduction (suppression of sympathetic compensatory mechanisms).
Combinations to use with caution
When using halogen-containing inhalation agents for general anesthesia, it should be taken into account that during surgery the effect of blockade of β-adrenergic receptors can be eliminated by beta-agonists. In general, beta-blocker therapy should not be discontinued, and abrupt discontinuation of the drug should be avoided in any case. The anesthesiologist must be informed of the treatment being carried out. When used simultaneously with Lokren, antiarrhythmic drugs of class IA (quinidine, hydroquinidine and disopyramide) and class III (amiodarone, dofetilide, ibutilide, sotalol), some antipsychotics from the phenothiazine group (chlorpromazine, cyamemazine, levomepromazine, thioridazine), benzamides (amisulpride, sulpiride, tiapride), butyrophenones (droperidol, haloperidol), other antipsychotics (pimozide), as well as cisapride, diphemanil, erythromycin (for IV administration), halofantrine, mizolastine, moxifloxacin, pentamidine, spiramycin (for IV administration) and vincamine (for IV administration) may increase the risk of ventricular arrhythmia, especially of the “pirouette” type. (if combination therapy is necessary, monitoring of the clinical condition and ECG is required). When used simultaneously with propafenone, it is possible to develop disorders of contractility, automaticity and conduction (due to suppression of sympathetic compensatory mechanisms), which requires monitoring of the clinical condition and ECG. When used together with baclofen, the antihypertensive effect may be enhanced (blood pressure monitoring and dose adjustment are necessary if necessary). When used together with insulin and oral sulfonylurea hypoglycemic agents, it should be taken into account that all beta-blockers can mask the symptoms of hypoglycemia (palpitations and tachycardia). The patient should be warned about the need to increase control of blood glucose levels, especially at the beginning of treatment. When used simultaneously with cholinesterase inhibitors (donepezil, galantamine, ambenonium chloride, neostigmine, pyridostigmine, rivastigmine, tacrine), the risk of bradycardia may increase (additive effect), which requires monitoring the clinical condition. When used together with centrally acting antihypertensive drugs (clonidine, apraclonidine, alpha-methyldopa, guanfacine, moxonidine, rilmenidine), a significant increase in blood pressure is possible with abrupt discontinuation of the centrally acting antihypertensive drug (it is necessary to avoid abrupt withdrawal of the antihypertensive drug and monitor the clinical condition). With intravenous administration of lidocaine, an increase in the concentration of lidocaine in the blood plasma is possible with a possible increase in undesirable neurological symptoms and effects from the cardiovascular system (decreased metabolism of lidocaine in the liver), which requires monitoring of the clinical condition and ECG and, possibly, monitoring the concentration of lidocaine in the blood plasma during treatment with beta-blockers and after its cessation. If necessary, adjust the dose of lidocaine.
Combinations to consider
When used simultaneously with NSAIDs for systemic use (including selective COX-2 inhibitors), the hypotensive effect may be reduced (inhibition of prostaglandin synthesis and water and sodium retention). When used simultaneously with calcium channel blockers, arterial hypotension and circulatory failure may develop in patients with latent or uncontrolled heart failure. Treatment with beta-blockers may minimize reflex sympathetic mechanisms. When used together with tricyclic antidepressants (such as imipramine), antipsychotics, the hypotensive effect may be enhanced and the risk of developing orthostatic hypotension may be increased (additive effect). When used simultaneously with mefloquine, the risk of developing bradycardia increases (additive effect). When used together with dipyridamole (for intravenous administration), the antihypertensive effect may be enhanced. When administered simultaneously with alpha-blockers used in urology (alfuzosin, doxazosin, prazosin, tamsulosin, terazosin), the antihypertensive effect is enhanced and the risk of orthostatic hypotension increases. When used together with amifostine, the antihypertensive effect may be enhanced. Allergens used for immunotherapy or allergen extracts for skin testing increase the risk of severe systemic allergic reactions or anaphylaxis in patients receiving betaxolol. Phenytoin, when administered intravenously, increases the severity of the cardiodepressive effect and the likelihood of a decrease in blood pressure in patients taking betaxolol. When used together, betaxolol reduces the clearance of xanthines (except diphylline) and increases their concentration in the blood plasma, especially in patients with initially increased clearance of theophylline (for example, under the influence of smoking). The hypotensive effect of betaxolol is weakened by estrogens (sodium retention). When used together with betaxolol, cardiac glycosides, methyldopa, reserpine and guanfacine increase the risk of developing or worsening bradycardia, AV block, and cardiac arrest. When used together with betaxolol, nifedipine, diuretics, clonidine, sympatholytics, hydralazine and other antihypertensive drugs can lead to a significant decrease in blood pressure. When used together, betaxolol prolongs the duration of action of non-depolarizing muscle relaxants and enhances the anticoagulant effect of coumarins. When used together with betaxolol, ethanol, sedatives and hypnotics increase CNS depression. Concomitant use with MAO inhibitors is not recommended due to a significant increase in the hypotensive effect; the break in treatment between taking MAO inhibitors and betaxolol should be at least 14 days. When used together with betaxolol, non-hydrogenated ergot alkaloids increase the risk of developing peripheral circulatory disorders.
Overdose
Overdose
Symptoms: Severe bradycardia, Dizziness, Severe decrease in blood pressure, Arrhythmias, ventricular extrasystole, AV block, Fainting, Heart failure, Difficulty breathing, bronchospasm, Cyanosis of fingernails and palms, Convulsions.
Storage conditions
Storage conditions
Store at temperatures below 25 °C out of the reach of children.
Shelf life
Shelf life
5 years.
Manufacturer
Manufacturer
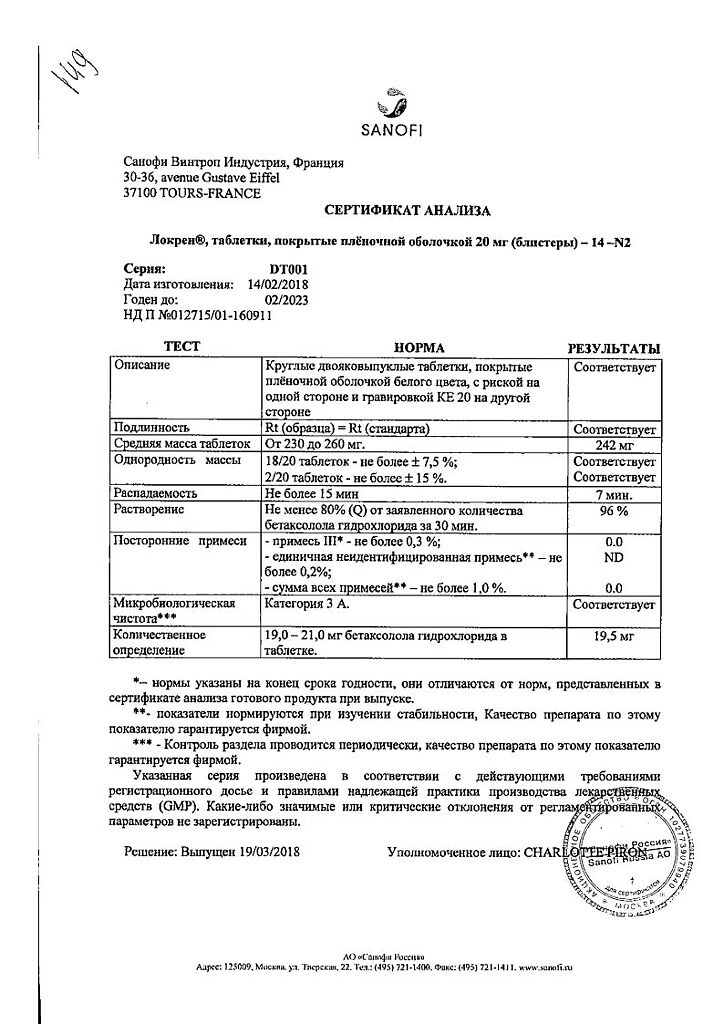
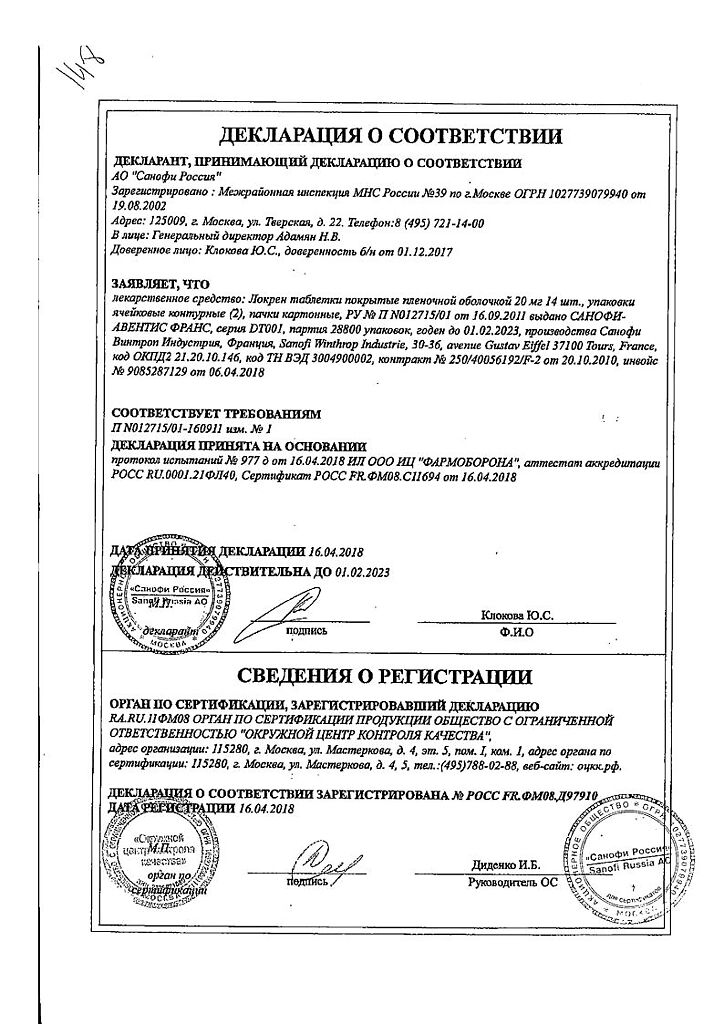
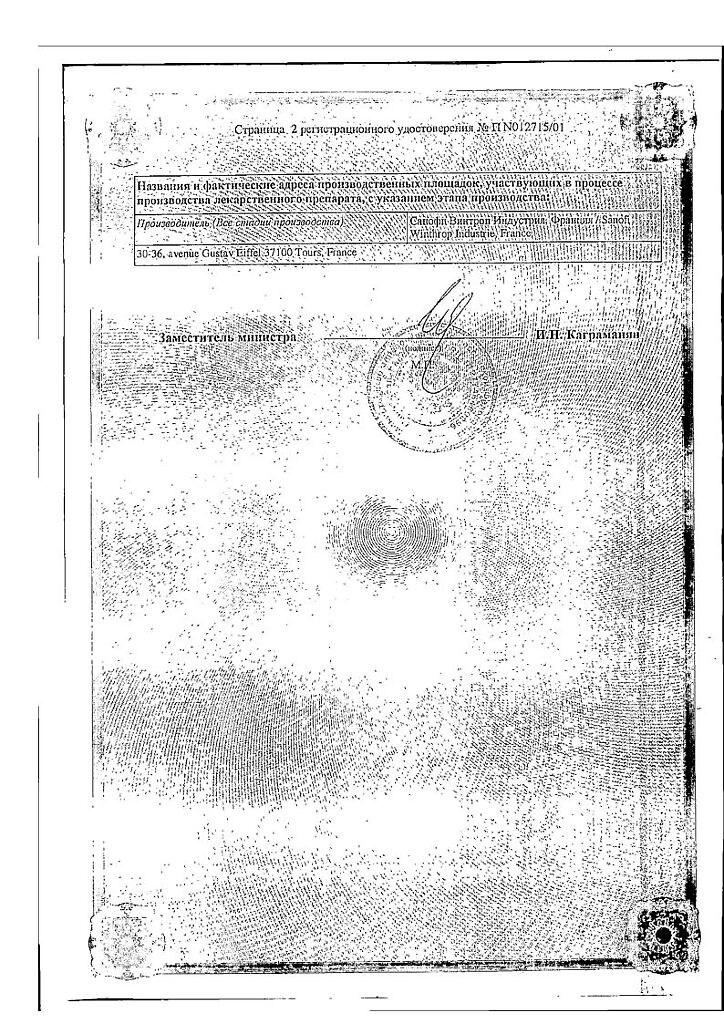
Sanofi Winthrop Industries, France
Additional information
| Shelf life | 5 years. |
|---|---|
| Conditions of storage | Store at temperatures below 25 °C and out of the reach of children. |
| Manufacturer | Sanofi Winthrop Industry, France |
| Medication form | pills |
| Brand | Sanofi Winthrop Industry |
Related products
Buy Lokren, 20 mg 28 pcs. with delivery to USA, UK, Europe and over 120 other countries.