No products in the cart.
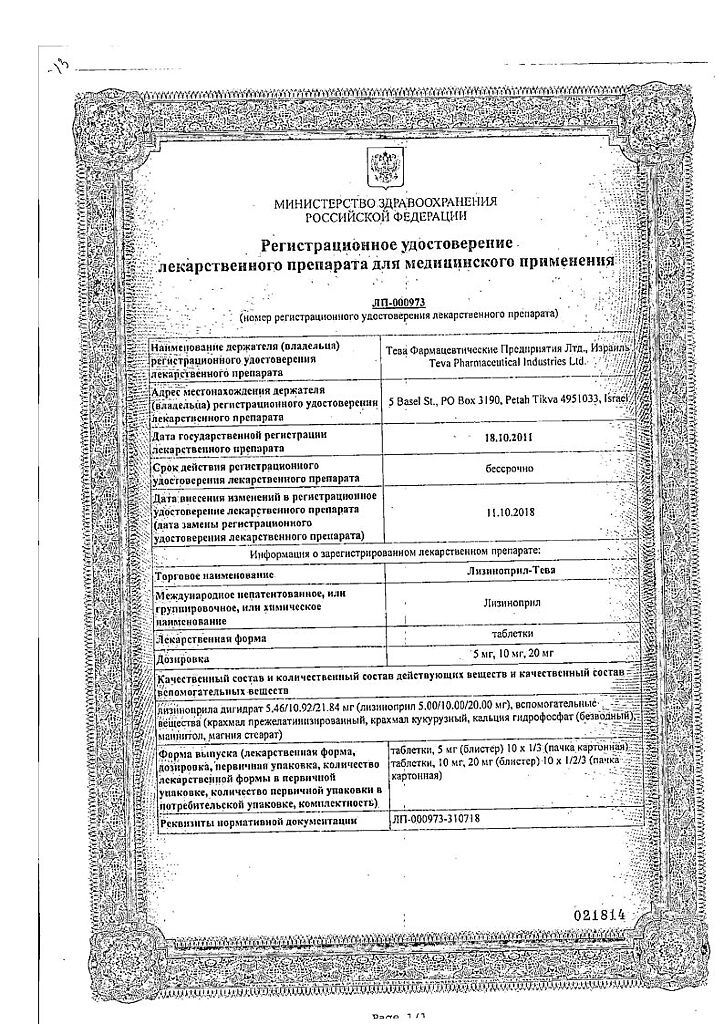
Lisinopril-Teva, tablets 10 mg 20 pcs
€3.91 €3.26
Description
Pharmacotherapeutic group: angiotensin-converting enzyme inhibitor
ATX code: C09AA03
Pharmacological properties
Pharmacodynamics. Angiotensin-converting enzyme (ACE) inhibitor, reduces the formation of angiotensin II from angiotensin I. Decreased angiotensin II leads to a direct reduction in aldosterone release. Reduces bradykinin degradation and increases prostaglandin synthesis. Reduces total peripheral vascular resistance (TPR), blood pressure (BP), preload, pulmonary capillary pressure, causes an increase in minute blood volume and increases myocardial tolerance to exercise in patients with chronic heart failure. Dilates arteries more than veins. Some effects are attributed to effects on the renin-angiotensin-aldosterone system (RAAS). Long-term use reduces myocardial hypertrophy and resistive arterial wall hypertrophy. It improves the blood supply to the ischemic myocardium.
The ACE inhibitors prolong life expectancy in patients with chronic heart failure (CHF), slow the progression of left ventricular dysfunction in patients who have had acute myocardial infarction without clinical manifestations of heart failure. Onset of action of the drug is within 1 hour, the maximum antihypertensive effect is achieved after 6-7 hours and is maintained for 24 hours. The duration of the effect also depends on the dose taken. In arterial hypertension, the effect is noted in the first days after the start of treatment, a stable effect develops after 1-2 months of therapy. When lisinopril is abruptly withdrawn, no pronounced increase in BP has been observed.
Lisinopril decreases albuminuria. It does not affect blood glucose concentrations in patients with diabetes mellitus and does not lead to increased incidence of hypoglycemia.
Pharmacokinetics
Intake. After oral administration, lisinopril is absorbed from the gastrointestinal tract (GIT) by an average of 25%, but absorption can vary from 6 to 60%. Bioavailability is 29%. Maximum plasma concentration (Cmax) is reached after 7 h. Food intake does not affect the absorption of lisinopril.
Distribution. Lisinopril binds insignificantly to plasma proteins. Permeability through the blood-brain barrier and the placental barrier is low.
Metabolism. Lisinopril is not biotransformed in the body.
Elimination. It is excreted unchanged by the kidneys. The elimination half-life (T1/2) is 12.6 h. Clearance of lisinopril is 50 ml/min. Decrease in serum concentration of lisinopril occurs in two phases. The bulk of lisinopril is excreted during the initial alpha phase (effective T1/2 – 12 h), followed by the terminal distant beta phase (about 30 h).
Pharmacokinetics in selected patient groups
In patients with CHF the absorption and clearance of lisinopril is decreased and the bioavailability is 16%.
In patients with renal impairment (creatinine clearance (CK) less than 30 ml/min), lisinopril concentrations are several times higher than plasma concentrations in healthy volunteers, with increased time to reach Cmax in plasma and increased T1/2.
In elderly patients, the plasma concentration of the drug and the area under the concentration-time curve are 2 times greater than in younger patients.
In patients with cirrhosis the bioavailability of lisinopril is reduced by 30% and clearance by 50% compared to patients with normal liver function.
In elderly patients, the blood concentration of lisinopril is increased by an average of 60%.
Indications
Indications
– Arterial hypertension (in monotherapy or in combination with other hypotensive agents).
– Chronic heart failure (as part of combined therapy).
– Early treatment of acute myocardial infarction (in the first 24 h with stable hemodynamic parameters to maintain these parameters and prevent left ventricular dysfunction and heart failure).
– Diabetic nephropathy (reduction of albuminuria in patients with diabetes mellitus type 1 with normal blood pressure and in patients with diabetes mellitus type 2 with arterial hypertension).
Active ingredient
Active ingredient
Composition
Composition
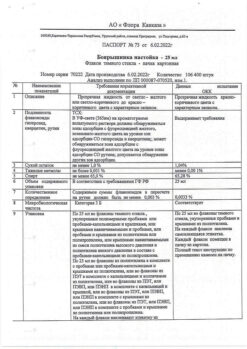
1 tablet contains: the active ingredient lisinopril dihydrate (lisinopril) – 5.46 mg (5.00 mg); 10.92 mg (10.00 mg); 21.84 mg (20.00 mg);auxiliary substances: Pregelatinized starch (12.00/12.00/12.00 mg), corn starch (40.00/40.00/40.00 mg), calcium hydrophosphate (anhydrous) (90.34/84.88/73.96 mg), mannitol (70.00/70.00/70.00 mg), magnesium stearate (2.20/2.20/2.20 mg).
How to take, the dosage
How to take, the dosage
The drug Lisinopril-Teva is taken orally once a day, regardless of the time of meals, preferably at the same time of the day. The dose is adjusted individually.
In patients with arterial hypertension who are not receiving other hypotensive agents, 5 mg per day is used. If there is no therapeutic effect, the dose is increased every 2-3 days by 5 mg to a dose of 20-40 mg/day (an increase in dose over 40 mg/day usually does not lead to further BP reduction).
The average daily maintenance dose is 20 mg. The maximum daily dose is 40 mg.
Therapeutic effect usually develops in 2-4 weeks from the beginning of treatment, which should be taken into account when increasing the dose. If the effect is insufficient, concomitant use of the drug with other hypotensive agents is possible.
If the patient has received prior treatment with diuretics, the administration of these drugs should be stopped 2-3 days before the start of the drug Lisinopril-Teva. If this is not possible, the initial dose of Lisinopril-Teva should not exceed 5 mg per day. In this case, after the first dose it is recommended to have a physician’s control for several hours (the maximum effect is reached after about 6 hours), since a marked decrease in BP may occur.
In renovascular hypertension associated with increased RAAS activity, a low initial dose of 2.5 mg per day should also be used in the follow-up, under increased medical monitoring (BP, renal function, serum potassium control). The maintenance dose, while continuing close medical supervision, should be determined depending on the dynamics of BP.
In chronic heart failure, the initial dose is 2.5 mg per day, the dose is gradually increased (by no more than 10 mg, at intervals of at least 2 weeks) depending on the BP. The maximum daily dose is 20 mg.
In early treatment of acute myocardial infarction, the dose is 5 mg in the first day, then 5 mg every other day, 10 mg after two days and then 10 mg daily as maintenance therapy. In patients with acute myocardial infarction, the drug should be used for at least 6 weeks. At the beginning of treatment or during the first 3 days after myocardial infarction in patients with low systolic blood pressure (120 mm Hg or less), a lower dose of 2.5 mg of Lisinopril-Teva should be used. It is not recommended to use Lisinopril-Teva if systolic blood pressure is lower or equal to 100 mmHg. In concomitant renal failure (CKR less than 80 ml/min), the drug dose should be adjusted accordingly.
In diabetic nephropathy in patients with type 1 diabetes mellitus, Lisinopril-Teva is used in a dose of 10 mg daily. If necessary, the dose may be increased to 20 mg per day to achieve a diastolic BP below 75 mmHg in sitting position. In patients with diabetes mellitus type 2, Lisinopril-Teva is used in the same dose with the goal of achieving diastolic BP below 90 mmHg in sitting position.
In renal failure and in patients on hemodialysis, the starting dose is set according to CK. The maintenance dose is determined depending on BP (under control of renal function and blood potassium and sodium levels).
KCK (ml/min.)
Starting dose (mg/day)
30-80
5-10
10-29
2.5-5
less than 10 (including patients on hemodialysis)
2.5
Interaction
Interaction
Caution should be exercised when using lisinopril concomitantly with potassium-saving diuretics (spironolactone, triamterene, amiloride, eplerenone), potassium preparations, salt substitutes containing potassium, cyclosporine: the risk of hyperkalemia increases, especially with impaired renal function. Therefore, these combinations should be used only on the basis of individual decision of a physician with regular monitoring of serum potassium and renal function.
The antihypertensive effect of lisinopril is enhanced when used concomitantly with diuretics and other hypotensive agents.
Concomitant use with NSAIDs (including selective cyclooxygenase-2 (COX-2) inhibitors), acetylsalicylic acid at a dose greater than 3 g/day, estrogens, and sympathomimetics reduces the antihypertensive effect of lisinopril. NSAIDs, including those from COX-2 selective inhibitors group, as well as ACE inhibitors may increase serum potassium content and in some cases worsen renal function. This effect is usually reversible.
Lisinopril slows excretion of lithium preparations, therefore concomitant use causes reversible increase in its plasma concentration. This may increase the likelihood of adverse events, therefore serum lithium concentration should be monitored regularly.
Concomitant use with antacids and colestiramine decreases gastrointestinal absorption of lisinopril.
Ethanol increases the effect of lisinopril.
Concomitant use with insulin and hypoglycemic agents for oral administration increases the risk of hypoglycemia.
Concomitant use of lisinopril with vasodilators, barbiturates, antipsychotics (neuroleptics), tricyclic antidepressants, slow calcium channel blockers, beta-adrenoblockers may increase the antihypertensive effect.
When concomitant use of ACE inhibitors andgold preparations intravenously (sodium aurothiamalate), a symptom complex including facial hyperemia, nausea, vomiting and BP decrease has been described.
The co-administration with allopurinol, procainamide, cytostatics may lead to leukopenia.
Double RAAS blockade with angiotensin receptor antagonistsII (ARA II), ACE inhibitors or aliskiren (renin inhibitor) is associated with an increased risk of arterial hypotension, syncope, hyperkalemia, and renal dysfunction (including acute renal failure) compared to monotherapy. Regular monitoring of BP, renal function and blood electrolytes is necessary. See also section “Special Precautions”.
Concomitant use with mTOR inhibitors such as sirolimus, everolimus, temsirolimus may increase the risk of angina.may increase the risk of angioedema accompanied by swelling of the larynx or tongue, which may lead to airway obstruction (see Special Precautions). See section “Special Precautions”).
Concomitant use with trimoxazole (trimethoprim+sulfamethoxazole) may increase the risk of hyperkalemia (see section “Special Precautions”).
When used concomitantly with dipeptidyl peptidase inhibitors IVtype (DFS-IV) (glyptins) such as sitagliptin, saxagliptin, wildagliptin, linagliptin increases the risk of angioedema.
Concomitant use with racecadotril (encephalinase inhibitor) increases the risk of angioedema.
The simultaneous use of ACE inhibitors with drugs containing sacubitril (neprilysin inhibitor) increases the risk of angioedema, therefore simultaneous use of these drugs is contraindicated. ACE inhibitors should not be prescribed earlier than 36 hours after withdrawal of the drugs containing Sacubitril. Administration of the drugs containing Sacubitril is contraindicated in patients receiving ACE inhibitors and also within 36 hours after the last ACE inhibitor administration.
Concomitant use with estramustine also increases the risk of angioedema.
In observational studies, an increased incidence of angioedema was found in patients taking ACE inhibitors after the use of alteplase for thrombolytic therapy of ischemic stroke.
Special Instructions
Special Instructions
Synopsis
Synopsis
Contraindications
Contraindications
Side effects
Side effects
The most common side effects are dizziness, headache, increased fatigue, diarrhea, dry cough, nausea.
The frequency of side effects is classified according to the recommendations of the World Health Organization: very common – at least 10%; common – at least 1%, but less than 10%; infrequent – at least 0.1%, but less than 1%; rare – at least 0.01%, but less than 0.1%; very rare – less than 0.01%.
Cardiovascular system disorders: often – marked decrease in BP, orthostatic hypotension; infrequently – acute myocardial infarction, tachycardia, palpitations, Raynaud’s syndrome; rarely – bradycardia, tachycardia, worsening of symptoms of CHF course, atrioventricular conduction disorder, chest pain.
On the central nervous system:often – dizziness, headache; infrequently – mood lability, paresthesias, sleep disturbances, stroke; rarely – confusion, asthenic syndrome, convulsive twitching of muscles of the limbs and lips, drowsiness; frequency is unknown – depression, fainting.
With the hematopoietic system and lymphatic system: rare – decrease in hemoglobin, hematocrit; very rare – leukopenia, neutropenia, agranulocytosis, thrombocytopenia, eosinophilia, erythropenia, hemolytic anemia, lymphadenopathy, autoimmune diseases, suppression of bone marrow function.
In the respiratory system:often – cough; infrequently – rhinitis; very rarely – sinusitis, bronchospasm, allergic alveolitis/eosinophilic pneumonia, shortness of breath.
Digestive system disorders: often – diarrhea, vomiting; infrequently – dyspepsia, changes in taste, abdominal pain; rarely – dry mouth mucosa; very rarely – pancreatitis, jaundice (hepatocellular or cholestatic), hepatitis, liver failure, intestinal edema, anorexia.
Skin side: infrequent – skin itching, rash; rarely – angioedema of the face, extremities, lips, tongue, throat, urticaria, alopecia, psoriasis; very rarely – increased sweating, vasculitis, vesicular rash, photosensitization, toxic epidermal necrolysis (Lyell syndrome), erythema multiforme, Stevens-Johnson syndrome, cutaneous pseudolymphoma.
In the urinary system:often – renal dysfunction; infrequently – uremia, acute renal failure; very rarely – anuria, oliguria, proteinuria.
Reproductive system disorders: infrequent – impotence; rarely – gynecomastia.
Metabolic disorders:very rarely – hypoglycemia.
Laboratory disorders: infrequent – increased blood urea concentration, hypercreatininemia, hyperkalemia, increased activity of liver transaminases; rare – hyperbilirubinemia, hyponatremia, increased erythrocyte sedimentation rate, false positive results of antinuclear antibodies test.
Musculoskeletal system disorders: frequently – arthralgia/arthritis, myalgia.
Others: rarely, a symptom complex including facial hyperemia, nausea, vomiting, and decreased BP has been described when concomitant use with intravenous gold drugs (see “Interaction with other medications”).
Overdose
Overdose
Pregnancy use
Pregnancy use
Similarities
Similarities
Additional information
| Shelf life | 2 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | Store at a temperature not exceeding 25 C. Keep out of reach of children! |
| Manufacturer | Teva LLC, Russia |
| Medication form | pills |
| Brand | Teva LLC |
Other forms…
Related products
Buy Lisinopril-Teva, tablets 10 mg 20 pcs with delivery to USA, UK, Europe and over 120 other countries.